|
 |
- Search
| Psychiatry Investig > Volume 19(10); 2022 > Article |
|
Abstract
Objective
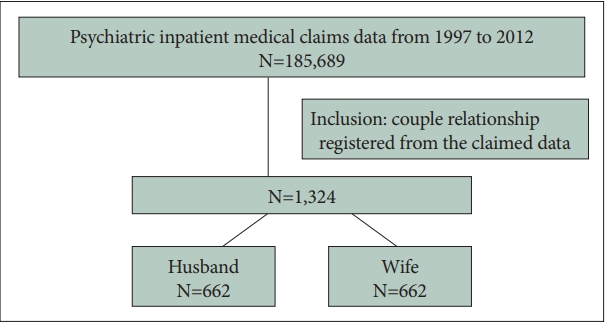
Methods
Results
Conclusion
Supplementary Materials
Supplementary Table 3.
Supplementary Table 4.
Notes
Availability of Data and Material
All data generated or analyzed during the study are included in this published article (and its supplementary information files).
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Cheng-Chen Chang, Jeng-Yuan Chiou. Data curation: Yu-Hsun Wang, Jong-Yi Wang. Formal analysis: Yu-Hsun Wang, Jong-Yi Wang. Funding acquisition: Po-Chung Ju, Jong-Yi Wang. Investigation: Ming-Hong Hsieh, Jeng-Yuan Chiou, Yu-Hsun Wang. Methodology: Cheng-Chen Chang, Jeng-Yuan Chiou, Jong-Yi Wang. Writing—original draft: Cheng-Chen Chang, Jong-Yi Wang. Writing—review & editing: Ming-Hong Hsieh, Po-Chung Ju.
Funding Statement
This research was supported by Ministry of Science and Technology, Taiwan (Grant No. MOST110-2410-H-039-001).
ACKNOWLEDGEMENTS
Table 1.
Table 2.
| Mental disorder | N1* |
Concordant mental disorders |
Cross-cordant mental disorders |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N2 | %† | κ | p value | N3 (1st) | %‡ | N4 (2nd) | %§ | ||||
| Anxiety disorder | 1,005 | 820 | 61.9 | 0.2368 | <0.001 | Depressive disorder | 657 | 49.6 | Bipolar disorder | 511 | 38.6 |
| Depressive disorder | 831 | 582 | 44.0 | 0.1992 | <0.001 | Anxiety disorder | 657 | 49.6 | Bipolar disorder | 430 | 32.5 |
| Bipolar disorder | 634 | 394 | 29.8 | 0.2836 | <0.001 | Anxiety disorder | 511 | 38.6 | Depressive disorder | 430 | 32.5 |
| Schizophrenia | 628 | 376 | 28.4 | 0.2456 | <0.001 | Anxiety disorder | 470 | 35.5 | Depressive disorder | 377 | 28.5 |
| Sleep disorder | 415 | 190 | 14.4 | 0.2106 | <0.001 | Anxiety disorder | 341 | 25.8 | Depressive disorder | 274 | 20.7 |
| Substance use disorder | 322 | 144 | 10.9 | 0.2845 | <0.001 | Anxiety disorder | 274 | 20.7 | Depressive disorder | 239 | 18.1 |
| Dementia | 283 | 118 | 8.9 | 0.2762 | <0.001 | Anxiety disorder | 201 | 15.2 | Depressive disorder | 178 | 13.4 |
| Alcoholism | 231 | 44 | 3.3 | 0.0910 | 0.001 | Anxiety disorder | 184 | 13.9 | Depressive disorder | 163 | 12.3 |
Concordant mental disorder: a married couple is defined to have a concordance of mental disorders if both spouses were diagnosed with mental disorder of an identical category in the International Classification of Diseases, Ninth Revision, Clinical Modification. Cross-cordant mental disorders: a married couple has different types of mental disorders.
Table 3.
Table 4.
REFERENCES