Differences in Functional Level and Central Symptom of Network Structures in the Patients Seeking Treatment for Panic Disorder Before and During the COVID-19 Pandemic
Article information
Abstract
Objective
Mental health problems such as anxiety, panic, and depression have been exacerbated by the coronavirus disease-2019 (COVID-19). This study aimed to compare the symptom severities and overall function before and during the COVID-19 pandemic among patients with panic disorder (PD) seeking treatment compared to healthy controls (HCs).
Methods
Baseline data were collected from the two groups (patients with PD and HCs) in two separate periods: before COVID-19 (Jan 2016–Dec 2019) and during COVID-19 (Mar 2020–Jul 2022). A total 453 participants (before COVID-19: 246 [139 patients with PD and 107 HCs], during COVID-19: 207 [86 patients with PD and 121 HCs]) was included. Scales for panic and depressive symptoms and overall function were administered. Additionally, network analyses were performed to compare the two groups within the patients with PD.
Results
The results of two-way analysis of variance analyses showed that patients with PD enrolled during COVID-19 showed higher levels of interoceptive fear and lower overall functioning. In addition, a network comparison test revealed that a significantly high strength and expected influence for agoraphobia and avoidance in patients with PD during COVID-19.
Conclusion
This study suggested that the overall function could have worsened, and the importance of agoraphobia and avoidance as a central symptom may have increased in patients with PD seeking treatment during COVID-19.
INTRODUCTION
In March 2020, the World Health Organization declared the coronavirus disease-2019 (COVID-19) pandemic caused by the novel severe acute respiratory syndrome coronavirus-2 [1]. COVID-19 has caused physical problems, including psychiatric and neuropsychiatric manifestations, in every facet of human life [2]. Fear of illness and uncertainty about the future precipitated anxiety and stress-related disorders, along with the direct effects of the severe acute respiratory syndrome coronavirus-2 and the subsequent host immunological response on the human central nervous system [3].
Huge stressors, such as images of older adults and dead bodies shown by the media, social distancing, loss of loved ones without seeing them, strong quarantine methods that deprived people of freedom, fear of vaccines, and economic crisis with unemployment, resulted in significant burden and functional impairment in daily life [4,5]. Stress, anxiety, and depression were prevalent at the peak of the COVID-19 outbreak [6] as well as in non-peak situations [7]. Furthermore, distress from uncertainty and unpredictability regarding the endpoint of the COVID-19 pandemic led to mental health issues, such as anxiety, depression, and panic symptoms [4,5].
A recent case report suggested that COVID-19 infection exacerbates existing psychiatric illness and induces panic disorder (PD), characterized by recurrent panic attacks, anticipatory anxiety, agoraphobia, and related functional impairment [8,9]. Additionally, another study showed a 3% new incidence of PD during the COVID-19 pandemic in 2020 in 11 countries, including the UK, Belgium, Netherlands, Bulgaria, Czech Republic, Finland, India, Latvia, Poland, Romania, and Sweden [10].
Network analysis can help analyze anxiety symptoms and functional decline using different indices, such as edge weight and centrality, which focuses on the relationship between symptoms and functioning during the COVID-19 outbreak. In a cross-sectional network analysis study among nurses, psychological symptoms, such as irritability, uncontrollable worry, trouble relaxing, and depressed mood, had the highest centrality values during the COVID-19 pandemic [11]. Furthermore, the analysis revealed that sad mood, irritability, worry, and guilt formed central symptoms in adolescents during COVID-19 [12]. However, these are all cross-sectional studies conducted during the COVID-19 pandemic and are not comparisons between findings before and during the COVID-19 pandemic. Therefore, it is important to conduct research that compares the symptoms and functioning of mental health problems before and during COVID-19.
Therefore, the initial psychological symptoms, functioning, and network structures of patients seeking treatment for PD at the hospital before and during the COVID-19 pandemic should be compared with those of the healthy control (HC) group before and during that period. Thus, the study proposes the following hypotheses: 1) the psychological symptoms and functioning of patients with PD seeking treatment will differ from those of HCs before and during the COVID-19 pandemic and 2) the central nodes (psychological symptoms or functional levels) and edge weights during the COVID-19 pandemic were different from those before the COVID-19 pandemic in patients with PD.
METHODS
Participants
Two cross-sectional studies included 453 Korean participants aged 16–75 years, comprising 225 patients with PD and 228 healthy individuals. We recruited a pool of patients with PD who visited the psychiatry outpatient clinic at the CHA Bundang Medical Center in Gyeonggi-do, Korea for the first time for diagnosis and treatment, and HCs from the same local community through advertisements. Participants’ individual and family histories were collected through interviews.
The first baseline data collection was conducted before the COVID-19 pandemic from January 2016 to December 2019. Of the 279 initial participants, six HCs were excluded because they did not meet the inclusion criteria and 27 patients with PD who did not satisfy the inclusion criteria were excluded. Finally, 246 individuals, including 139 patients with PD and 107 healthy individuals, participated in the first stage of the study. The second baseline data collection was performed during the COVID-19 pandemic, from March 2020 to July 2022. There were 207 participants, including 86 patients with PD and 121 HCs; this was after seven patients with PD and 13 HCs, who did not satisfy the inclusion criteria of the 227 participants, at baseline were excluded (Figure 1). Additionally, consistency in data collection was maintained until the end of recruitment to achieve homogeneity among all participants.
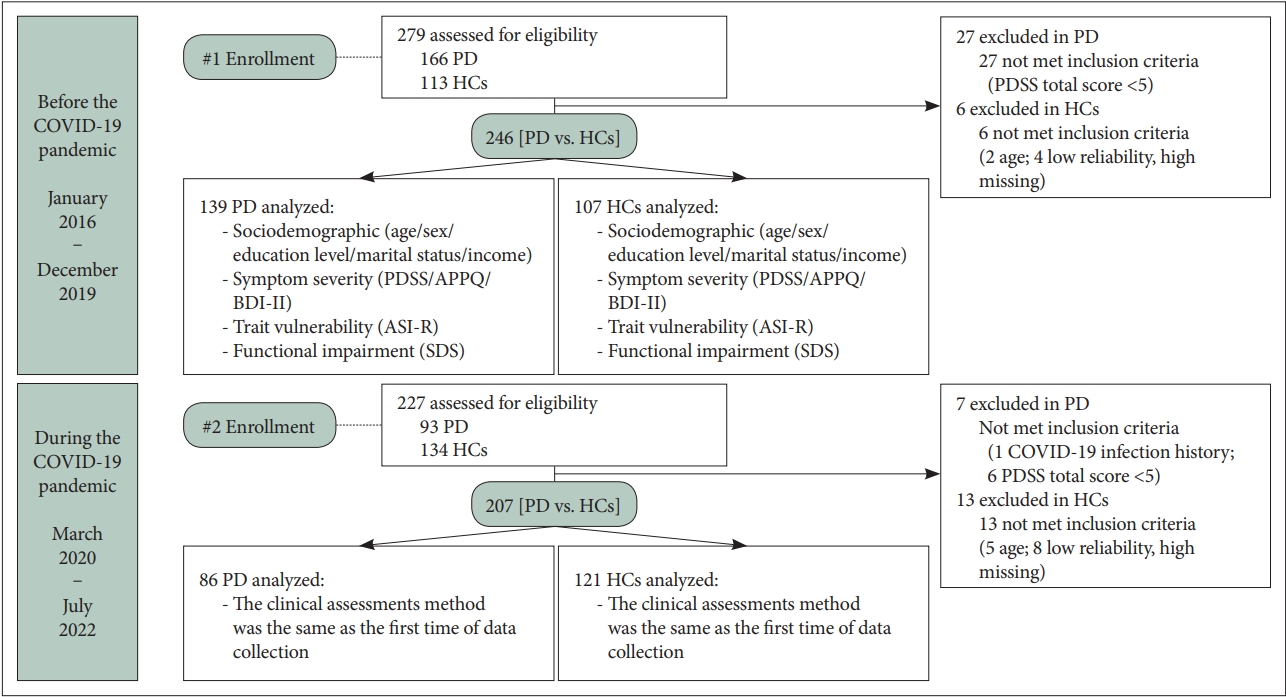
Flow diagram of participant recruitment before and during the COVID-19 pandemic period. COVID-19, coronavirus disease-2019; PD, panic disorder; HCs, healthy controls; PDSS, Panic Disorder Severity Scale; APPQ, Albany Panic and Phobia Questionnaire; BDI-II, Beck Depression Inventory; ASI-R, Anxiety Sensitivity Index-Revised; SDS, Sheehan Disability Scale.
Regarding PD, the inclusion criteria were only primary patients with PD, with or without agoraphobia, diagnosed by practising psychiatrists using the Structured Clinical Interview to evaluate the Diagnostic and Statistical Manual of Mental Disorders, fourth edition, Text Revision Axis I Disorder. Moreover, the exclusion criteria for participants with PD included any history of past or ongoing anxiety disorders other than PD, schizophrenia and other psychotic disorders, depressive disorders, bipolar disorders, mental retardation, substance-related disorders, significant medical problems that included neurological disorders or brain damage, anaphylactic reactions to vaccines, COVID-19 infection, and pregnancy. The exclusion criteria for healthy individuals were as follows: 1) any history of major psychiatric disorders, 2) patients infected with COVID-19 and their families, 3) neurological disorders and traumatic brain injury, 4) pregnancy, and 5) person who made an unreliable questionnaire report.
All procedures were performed per the recommendations and ethics of the Institutional Review Board of the CHA Bundang Medical Center (2019-05-030). The study was explained in detail to the participants, following which written informed consent was obtained from the latest version of the Declaration of Helsinki. Additionally, principles of good clinical practice were acquired.
Clinical assessments
The Panic Disorder Severity Scale (PDSS), Albany Panic and Phobia Questionnaire (APPQ), Beck Depression Inventory (BDI-II), Anxiety Sensitivity Inventory-Revised (ASI-R), and Sheehan Disability Scale (SDS) were used to evaluate anxiety and depressive symptom severity and functional impairment in all participants.
The PDSS measures the severity of panic symptoms [13]. The PDSS is a 7-item self-rated measure of PD-specific symptoms, including 1) frequency of panic attacks, 2) distress during panic attacks, 3) severity of anticipatory anxiety, 4) phobic avoidance of situations, 5) phobic avoidance of physical sensation, 6) functional impairment in work, and 7) social functional impairment. Responses were scored on a 5-point scale ranging from 0 to 4. The Korean version of the PDSS has high reliability, validity, and internal consistency (Cronbach’s α=0.88).
The APPQ can evaluate agoraphobia, social phobia, and interoceptive fear in patients with PD. 14 We used the Korean version of the APPQ, which showed good internal consistency (Cronbach’s α=0.95) and high test-retest reliability (r=0.77) [15].
Additionally, the Korean version of the BDI-II was used to evaluate depression severity. The BDI-II consists of 21 self-administered items rated on a scale from 0 to 3, ranging from 0 to 63 [16]. The BDI-II has high internal consistency, with a Cronbach’s α coefficient of 0.93 among healthy adults [17]. Furthermore, in previous research on the Korean adult population, Cronbach’s α coefficient was 0.91, and the test-retest reliability was 0.84 [18].
The Korean version of the ASI-R (K-ASI-R) was used to evaluate anxiety sensitivity (AS) in all participants [19,20]. It is a commonly used measure of sensitivity to anxiety. Furthermore, it consists of the following items: fear of respiratory symptoms, cardiovascular symptoms, a publicly observable anxiety reaction, and cognitive dyscontrol. The K-ASI-R has high internal consistency (Cronbach’s α=0.92) and good test-retest reliability (r=0.82).
Developed by David Sheehan, the SDS is a simple, brief, and cost-effective self-report instrument to measure functional impairment levels through psychiatric or medical symptoms in three major domains. Therefore, it shows adequate levels of reliability (Cronbach’s α=0.56–0.83) and validity for patients with PD across the following domains: 1) work or school, 2) social life or leisure, and 3) family life or home responsibilities [21,22]. Each domain was measured on a scale ranging from 0 (not at all) to 1–3 (mild), 4–6 (moderate), 7–9 (marked), and 10 (extreme).
Analytical strategies
We used an independent t-test and chi-square test, with the significance level set at 0.05, to analyse the sociodemographic characteristics before and during the COVID-19 pandemic in each group of patients with PD and HCs. Furthermore, we performed Levene’s test for equality and homogeneity of variances for all demographic findings across the two samples during the two periods.
Regarding the clinical measurement of psychological symptoms, the two-factor analyses of variance (ANOVA) were applied to compare between before and during the COVID-19 pandemic in each group and determine the group-by COVID-19 period interaction effects. In addition, the Benjamini– Hochberg false discovery rate (FDR) method was used for each item or subscale for multiple correction tests. Statistical analyses were conducted using SPSS Windows software version 27.0 (IBM Corp., Armonk, NY, USA).
Network analysis was then performed regarding estimation, accuracy or stability, and comparison of networks among participants. We could not find network structures of HCs that were stable and accurate; therefore, we analyzed only the network structures of patients with PD before and during the COVID-19 pandemic.
Network estimation
To analyse the relationship between nodes (symptoms and functionality) among patients with PD as a network, the R software was used to estimate associations between nodes separately before and during the COVID-19 pandemic [23]. Initially, we constructed the network using Pairwise Markov Random Field (PMRF) [24]. The PMRF can construct a network in which each variable serves as a node. This network is represented by an undirected graph demonstrating the conditional dependence between two variables. Using the extended Bayesian information criterion model, the graphical least absolute shrinkage and selection operator was applied to reduce false associations and estimate a sparse network [25,26].
For node selection in our network analysis, 13 nodes were included for network estimation among patients with PD as shown Table 1: seven panic nodes (each score of 7-item in the PDSS), three phobic nodes (mean score of the APPQ-agoraphobia, social phobia, and interoceptive subscales), one depressive node (total score of the BDI-II), one AS node (total score of the ASI-R), and one functional impairment node (total score of three SDS subscales: 1) work/school, 2) social life/leisure, and 3) family life/home responsibilities).
In each network, two centrality measures were used to determine the central nodes and perform essential roles: 1) strength and 2) expected influence (EI) [27,28]. Strength is the sum of the absolute weights of all edges from a target node to a neighborhood. Contrastingly, EI is the summed edge weight from a target node, considering the sign of the association connecting the neighbors.
Network stability and accuracy
Bootstrapping was used to demonstrate the accuracy and reliability of the networks. The edge weights’ accuracy was calculated using 95% confidence intervals and bootstrapped mean edges [26,29]. The correlation stability coefficient (CS-C) was measured to evaluate the stability of the two centrality measurements using subset bootstrapping [30]. CS-C indicates the stability and reliability of the measured centrality index. Epskamp and Fried discussed in their previous work [26,31] that a CS-C of 0.5 or greater is a reliable measurement and should not be less than 0.25. Bootstrapped edge-weight difference tests were performed to evaluate the differences between edges [26].
Networks comparison test of before and during the COVID-19 pandemic among patients with PD
To assess network differences before and during the COVID-19 pandemic among patients with PD, we performed a network comparison test (NCT) using the R package “Network Comparision Test.” [32] A NCT was performed with 10,000 permutation samplings to evaluate the differences in invariance measures, including edge weights, strength, and EI [32,33] Furthermore, significant differences between the two networks were estimated separately using a p<0.05 (two-tailed) significance level.
RESULTS
Sociodemographic characteristics of patients seeking treatment for PD and HCs before and during the COVID-19 pandemic
Table 2 shows the sociodemographic characteristics of the patients with PD and HCs. There was no significant diagnosis-by-COVID-19 interaction effect in age, sex, education level, marital status, and income level. And there were no significant main diagnosis effects in age, sex, and monthly income, except for education level (p<0.001), between patients with PD and HCs. Additionally, among the patients with PD, there were no significant differences in the frequencies of agoraphobia, duration of illness, and the presence of medication, types, and doses of pharmacotherapy between before and during COVID-19 period group.
Comparison of the clinical characteristics of patients seeking treatment for PD and HCs before and during the COVID-19 pandemic
Table 3 shows clinical characteristics between the two groups divided before and during the COVID-19 pandemic within each group of patients with PD and HCs.

Comparison of clinical characteristics between patients with panic disorder (PD) and healthy controls (HCs)
As results of the two-factor ANOVA, there were significant diagnosis-by-COVID-19 interaction effects in the impairment in social functioning (PDSS item 7) (F=5.25, p=0.02), APPQ total score (F=4.72, p=0.03), interoceptive fear (F=5.91, p=0.02), SDS total score (F=5.33, p=0.02), work/school (SDS subscale) (F=4.03, p=0.045), social life (SDS subscale) (F=4.84, p=0.03), and family life/home responsibilities (SDS subscale) (F=5.32, p=0.02), including significant diagnostic effects in these variables. After FDR multiple corrections for each item or subscale, three subscales of the SDS remained (all FDR-adjusted p=0.045).
Network analysis
Among patients seeking treatment for PD, both network structures comprising 13 nodes showed non-zero 39 edges (50.0%) and 44 edges (56.4%) of the total 78 edges before and during the COVID-19 pandemic, respectively (Figure 2).
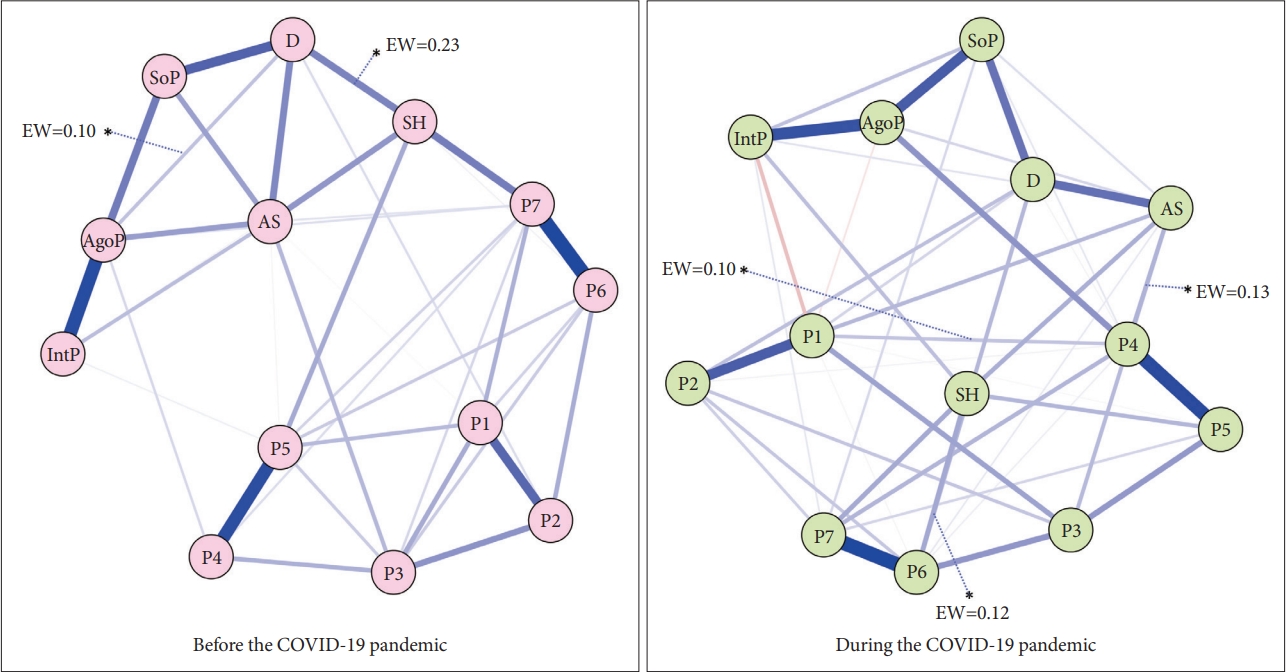
Clinical characteristics network before and during of the COVID-19 pandemic among patients with panic disorder. Blue edges indicate positive associations and red edges indicate negative associations. *indicates the edge weight which shows significant differences between the two networks. EW, edge weight; P1, panic attack frequency; P2, distress during panic attacks; P3, severity of anticipatory anxiety; P4, agoraphobic fear/avoidance; P5, panic-related sensation fear/avoidance; P6, impairment in work functioning; P7, impairment in social functioning; SoP, social phobia; SH, functional impairment; IntP, interoceptive fear; D, Beck Depression Inventory (BDI-II); AS, Anxiety Sensitivity Index-Revised (ASI-R); AgoP, agoraphobia; COVID-19, coronavirus disease-2019.
Estimated network structures before the COVID-19 pandemic among patients seeking treatment for PD
In the network before the COVID-19 pandemic (Figure 2), the strongest connection between the nodes was found in impairment in work functioning (P6)–impairment in social functioning (P7) (r=0.52), followed by agoraphobia (AgoP)–interoceptive fear (IntP) (r=0.47) and agoraphobic fear/avoidance (P4)–panic-related sensation fear/avoidance (P5) (r=0.45).
Figure 3 shows the strength and EI of all the nodes in the networks at different periods of patients with PD. In the before the COVID-19 pandemic network, P7 showed the highest strength and EI, while IntP reported the lowest value in both centrality measures in patients with PD. The second and third-highest strengths were demonstrated by AgoP and AS, and this tendency was also seen for EI.
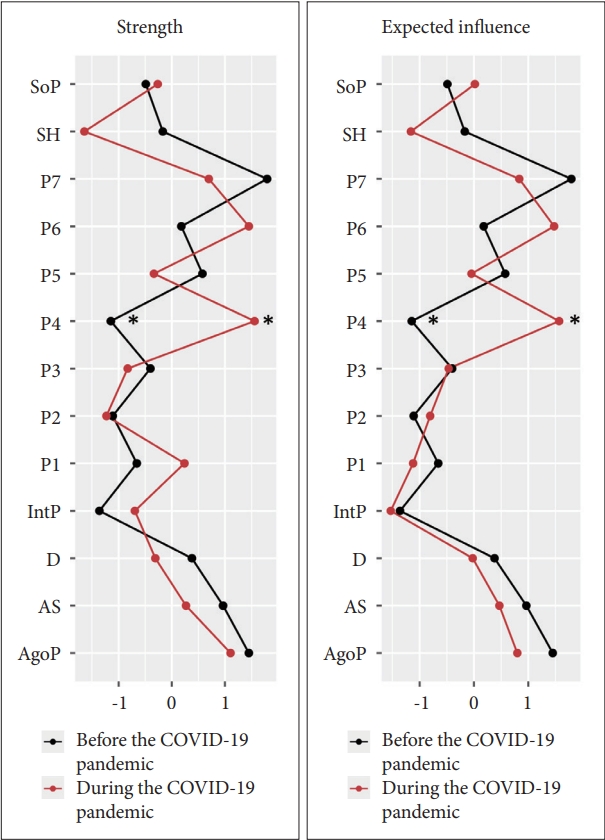
Strength and expected influence plots of all nodes within the network at different periods of the COVID-19 pandemic among patients with panic disorder. This figure shows strength and expected influence of all nodes within the network (z-scores). *metrics that are significantly different between before and during the COVID- 19 pandemic among patients with panic disorder networks. SoP, social phobia; SH, functional impairment; P7, impairment in social functioning; P6, impairment in work functioning; P5, panicrelated sensation fear/avoidance; P4, agoraphobic fear/avoidance; P3, severity of anticipatory anxiety; P2, distress during panic attacks; P1, panic attack frequency; IntP, interoceptive fear; D, Beck Depression Inventory (BDI-II); AS, Anxiety Sensitivity Index-Revised (ASIR); AgoP, agoraphobia; COVID-19, coronavirus disease-2019.
Estimated network structures during the COVID-19 pandemic among patients seeking treatment for PD
Meanwhile, in the network during the COVID-19 pandemic (Figure 2), P6–P7 (r=0.54) were the most substantial edge, like the before COVID-19 period group. However, the second strongest association was found in P4–P5 (r=0.50) and AgoP–IntP (r=0.44) as opposed to the before COVID-19 period group.
In the during the COVID-19 pandemic network as shown Figure 3, P4 showed the highest strength and EI. The second and third-highest strengths were demonstrated by P6 and P7, and this tendency was also seen for EI. And the overall functional impairment (SH) showed the lowest value in strength and IntP reported the lowest value in EI, respectively.
NCT of before and during the COVID-19 among patients with PD
The strength and EI invariance test before and during the COVID-19 period using the NCT are shown with asterisks in Figure 3. In terms of centrality, before the COVID-19 pandemic group has significantly higher strength (diff=0.49, p=0.001) and EI (diff=2.71, p=0.002) in the P4 than during the COVID-19 pandemic group.
Additionally, the edge weight scores were higher at the three edges during COVID-19 than before the COVID-19 pandemic: 1) P4–AS (diff=0.13, p=0.01); 2) P6–depressive symptoms (D) (diff=0.01, p=0.01); and 3) P4–panic attack frequency (P1) (diff=0.10, p=0.02). Notably, the scores of edge weights in D–SH (diff=-0.23, p=0.01) and D–AgoP (diff=-0.10, p=0.04) during the pandemic were significantly lower than those before the pandemic.
Network stability and accuracy before and during the COVID-19 pandemic among patients seeking treatment for PD
All edges were observed to fall within the range of 95% bootstrapped-confidence interval, suggesting a nonparametric bootstrapping procedure for verifying the edge weight accuracy of the two networks among patients with PD (Supplementary Figure 1 in the online-only Data Supplement). The bootstrapped edge weight difference test results are shown in Supplementary Figure 2 (in the online-only Data Supplement).
Strength, among centrality indices, showed fair stability to interpretation before and during the COVID-19 network (CS-C=0.36 and 0.36). And the CS-Cs for EI by case-dropping subset bootstrapping were 0.44 and 0.36 in the network before and during the COVID-19 pandemic, respectively (Supplementary Figure 3 in the online-only Data Supplement).
DISCUSSION
To the best of our knowledge, this is the first study to compare the baseline clinical characteristics and network structures before and during the COVID-19 pandemic between PD and HCs groups. Patients with PD seeking treatment in Korea during the COVID-19 pandemic had higher functional impairments in work, interpersonal relationships, and family life/home responsibilities than before the COVID-19 pandemic. In network analyses to estimate the relationship between psychological symptoms within a group of patients with PD, the centrality of agoraphobic fear/avoidance was higher than that in the period before the COVID-19 pandemic.
Patients with PD experienced significant functional impairments in work, interpersonal, and family relationships during the COVID-19 pandemic compared to before the COVID-19 pandemic. After controlling for confounding variables and considering the functional levels of HCs before and during the COVID-19, a significant group-by-period interaction effect was revealed. According to the previous study [34], the odds of functional impairment significantly increased by 27% for higher scores in separation distress, 25% for higher scores in dysfunctional grief, and 13% for higher scores in posttraumatic stress symptoms during the COVID-19 pandemic. Further, COVID-19 related to stress predicted large proportions of variance in anxiety, depression, health anxiety, and functional impairment in American adults [35]. Our results are also in line with those of the aforementioned previous studies. Our finding of changes in functional impairment in patients with PD suggests that during a pandemic, anxiety disorders such as PD, with high health concerns and high AS, may show a higher level of functional impairment in patients with PD than in healthy people. Therefore, policymakers in public mental health should consider these patients with PD.
Within the PD group, there was no significant difference in panic symptoms during the COVID-19 pandemic compared to before the COVID-19 pandemic. However, the interoceptive fear symptom tended to increase over the study period compared with before the COVID-19 pandemic in patients with PD. This can be explained by the possibility that during the COVID-19 pandemic, concerns about infection increased the sense of visceral organs, which may have increased somatic symptoms. Patients with PD were more vulnerable to various social and occupational situations during the COVID-19 pandemic.
In the network analysis of the PD group, NCT showed that the agoraphobic fear/avoidance symptom showed significantly higher scores on the strength and EI centrality measures during COVID-19 pandemic than before COVID-19. Notably, the agoraphobic fear/avoidance symptom was the second highest during the pandemic compared to the 12th-highest before the pandemic among the 13 symptoms in network analysis in patients with PD. In network analysis, the agoraphobic fear/avoidance increased its essentiality because they are newly associated with AS and social functional impairment during the COVID-19 pandemic. Our network analysis results are in line with those of the previous studies that exhibited an increase in avoidance behaviors during the COVID-19 pandemic in healthy individuals [36,37].
During the COVID-19 pandemic, patients with PD respond by avoiding virus-related cues or crowded places because they are overwhelmed by anxiety or fear of infection. During the COVID-19 pandemic, various social phenomena, such as stigma, racism, religious discrimination, and invasion of privacy, have emerged as socially controversial. In these social situations, patients with PD have a high sense of fear suppression in various areas of their lives. These continuous changes in behavior would have appeared as a response to avoiding unspecified situations. This response suggests that behavioral changes, such as agoraphobic fear/avoidance, during the COVID-19 pandemic in patients with PD may lead to other avoidance, vulnerability or sensitivity to anxiety, as well as functional impairment in the workplace and interpersonal or family relationships. However, it is necessary to study the changes in symptoms in patients with PD in situations where the spread of COVID-19 continues using a longitudinal design.
Despite these implications, this study had several limitations. First, it was designed using two cross-sectional studies. Therefore, it might be challenging to determine the exact causal effect and relationship of time changes because we did not follow up on the patients. Second, although there was no statistically significant difference in sociodemographics (except education level between HCs and PD) between the participants recruited before and during the COVID-19 pandemic, our study may have had a sampling bias, as all participants were recruited from one hospital in one region.
In summary, this study, including network analysis of PD during and before the COVID-19 pandemic, showed that patients with PD during the COVID-19 pandemic had significantly higher levels of social phobia and overall functional impairments in work, social, and family relationships than before the COVID-19 period. In addition, the importance of agoraphobic fear and avoidance as a central symptom may have increased during the COVID-19 period than before COVID-19 in patients with PD. It is necessary to focus on changes in central symptom patterns in patients with PD in future studies, as social situations continue to change according to the COVID-19 pandemic.
Supplementary Materials
The online-only Data Supplement is available with this article at https://doi.org/10.30773/pi.2022.0318.
Accuracy of edge weight parameters and their bootstrapped confidence intervals. The gray indicates the bootstrapped confidence intervals; and the red line represents the values of real sample. The y-axis represents all observed edges of the network. This accuracy analysis results showed accurate and small confidence intervals for all edge weights, suggesting that the sample is similar to the population. The name of the edge is omitted due to large number of edges. COVID-19, coronavirus disease-2019.
Edge weight bootstrapped difference test result of the network before and during the COVID-19 pandemic. Black boxes show edges that differ significantly form each other. Gray boxes show edges that do not significantly differ from each other. The number of black boxes is higher before than during the COVID-19 pandemic, indicating that the stability in the network is relatively high. P6, impairment in work functioning; P7, impairment in social functioning; AgoP, agoraphobia; IntP, interoceptive fear; P4, agoraphobic fear/avoidance; P5, panic-related sensation fear/avoidance; SoP, social phobia; D, Beck Depression Inventory-II (BDI-II); SH, functional impairment; AS, Anxiety Sensitivity Index-Revised (ASI-R); P1, panic attack frequency; P2, distress during panic attacks; P3, severity of anticipatory anxiety; COVID-19, coronavirus disease-2019.
Stability of strength and expected influence by case dropping subset bootstrap. The x-axis represents the percentage of cases of original sample used at each step. The y-axis represents the average of associations between the expected influence from the original network and that from the re-estimated networks after dropping increasing percentages of cases. The line indicates the average correlations of with original sample in the expected influence, while areas indicate 95% confidence interval. COVID-19, coronavirus disease-2019.
Notes
Availability of Data and Material
The data underlying this study will be shared on reasonable request to the corresponding authors.
Conflicts of Interest
Minji Bang, a contributing editor of the Psychiatry Investigation, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Author Contributions
Conceptualization: Hyun-Ju Kim, Sang-Hyuk Lee. Formal analysis: Hyun-Ju Kim, Sang-Hyuk Lee. Funding acquisition: Sang-Hyuk Lee. Investigation: Hyun-Ju Kim, Sang-Hyuk Lee. Methodology: Chongwon Pae, Sang-Hyuk Lee. Project administration: Sang-Hyuk Lee. Resources: Hyun- Ju Kim, Sang-Hyuk Lee. Software: Hyun-Ju Kim, Sang-Hyuk Lee. Supervision: Minji Bang, Chun Il Park, Chongwon Pae, Sang-Hyuk Lee. Validation: Sang-Hyuk Lee. Visualization: Hyun-Ju Kim, Sang-Hyuk Lee. Writing—original draft: Hyun-Ju Kim, Chongwon Pae, Sang-Hyuk Lee. Writing—review & editing: all authors.
Funding Statement
This study was supported by the Basic Science Research Program through the National Research Foundation of Korea, funded by the Ministry of Science and ICT [grant number NRF-2019M3C7A1032262], [grant number NRF-2021M3E5D9025026]. It was also funded in part by the Healthcare AI Convergence Research & Development Program through the National IT Industry Promotion Agency of Korea (NIPA), funded by the Ministry of Science and ICT [grant number S0254-22-1002]. Both sets of funding were secured by S.H. Lee.


