 |
 |
- Search
| Psychiatry Investig > Volume 20(7); 2023 > Article |
|
Abstract
Objective
Methods
Results
Conclusion
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Ki Won Jang, Hae Kook Lee, Byung Joo Park, HoonChul Kang, Sang-Kyu Lee, Chan-Hyung Kim, Daeyoung Roh. Formal analysis: Hae Kook Lee. Methodology: Ki Won Jang, Hae Kook Lee. Project administration: Daeyoung Roh. Resources: Byung Joo Park, Hoon-Chul Kang, Sang-Kyu Lee, Chan-Hyung Kim. Software: Sang Kyu Nam. Supervision: Byung Joo Park, Hoon-Chul Kang, Chan-Hyung Kim, Daeyoung Roh. Validation: Sang-Kyu Lee. Visualization: Sang Kyu Nam. WritingŌĆöoriginal draft: Ki Won Jang, Hae Kook Lee. WritingŌĆöreview & editing: Ki Won Jang, Hae Kook Lee, Daeyoung Roh.
Funding Statement
This work was supported by the National Academy of Medicine of Korea, KYOBO Life, Life Insurance Social Contribution Committee (2020), a National Research Foundation of Korea (NRF) grant funded by the Korean government (NRF-2022R1A2C1005797), and R&D Program for Forest Science Technology (Project No. 2021390A00-2123-0105) provided by Korea Forest Service (Korea Forestry Promotion Institute).
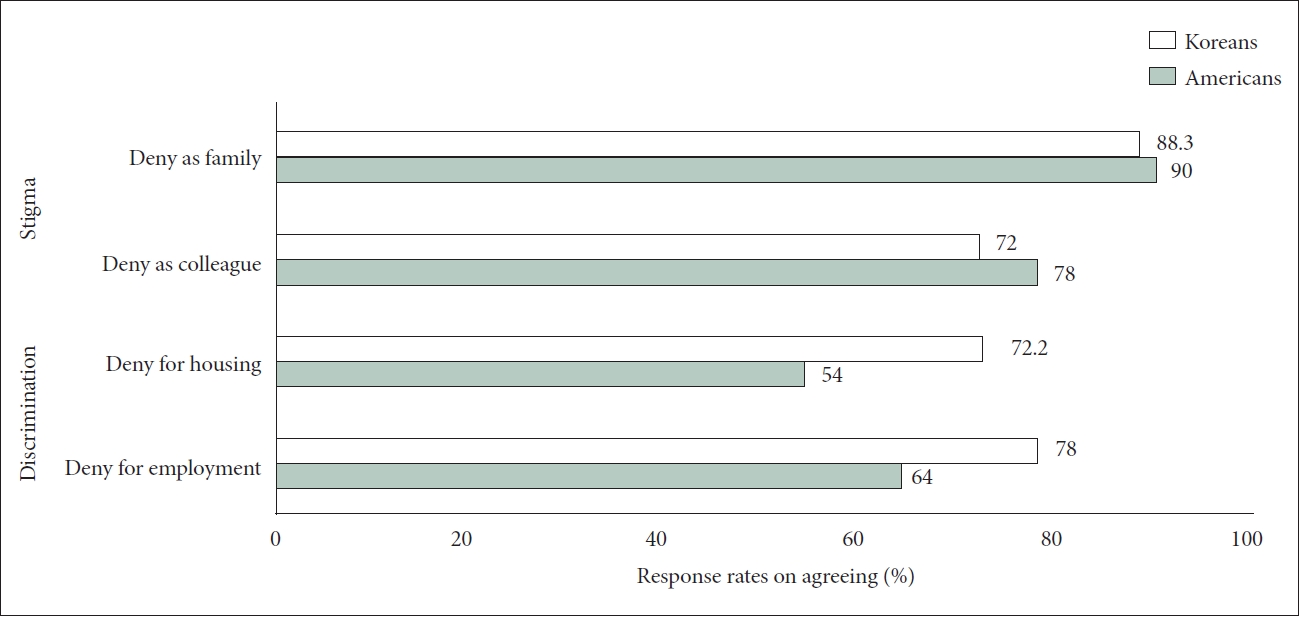
Figure┬Ā1.
Table┬Ā1.
Table┬Ā2.
| Categories | Stigma | F/p | Discrimination | F/p | |
|---|---|---|---|---|---|
| Gender | 27.24/<0.001 | 2.73/0.099 | |||
| Man | 4.07┬▒0.73 | 3.94┬▒0.83 | |||
| Woman | 4.28┬▒0.59 | 4.03┬▒0.81 | |||
| Age | 19.30/<0.001 | 9.72/0.002** | |||
| 19-39 yr | 4.05┬▒0.75 | 3.87┬▒0.83 | |||
| Ōēź40 yr | 4.24┬▒0.61 | 4.04┬▒0.81 | |||
| Residence | 0.01/0.919 | 1.06/0.303 | |||
| Capital | 4.17┬▒0.72 | 4.03┬▒0.82 | |||
| Other cities | 4.18┬▒0.66 | 3.97┬▒0.82 | |||
| Education | 2.65/0.104 | 0.67/0.412 | |||
| College or lower | 4.12┬▒0.70 | 3.95┬▒0.85 | |||
| College graduate or above | 4.20┬▒0.66 | 3.99┬▒0.80 | |||
| Monthly income | 6.23/0.013* | 25.07/<0.001 | |||
| 1,990,000-3,990,000 KRW | 4.12┬▒0.67 | 3.84┬▒0.84 | |||
| Ōēź4,000,000 KRW | 4.22┬▒0.67 | 4.10┬▒0.78 | |||
| Occupation | 0.25/0.621 | 0/0.983 | |||
| White-collar jobs | 4.16┬▒0.68 | 3.98┬▒0.81 | |||
| Blue-collar jobs | 4.18┬▒0.66 | 3.98┬▒0.83 | |||
| Opioid (narcotic) analgesic misuse | 25.34/<0.001 | 3.04/0.082 | |||
| Yes | 3.34┬▒0.87 | 3.63┬▒0.65 | |||
| No | 4.19┬▒0.66 | 3.98┬▒0.82 | |||
| Drinking | 2.59/0.108 | ||||
| Yes | 4.08┬▒0.69 | 35.64/<0.001 | 3.95┬▒0.80 | ||
| No | 4.34┬▒0.61 | 4.03┬▒0.85 | |||
| Smoking | 21.35/<0.001 | 5.47/0.020* | |||
| Yes | 3.99┬▒0.78 | 3.86┬▒0.86 | |||
| No | 4.22┬▒0.63 | 4.01┬▒0.81 | |||
Table┬Ā3.
| Gender | Age | Income | Opioid | Drinking | Smoking | Stigma | |
|---|---|---|---|---|---|---|---|
| Gender | |||||||
| Age | 0.02 | ||||||
| Income | -0.01 | 0.12*** | |||||
| Opioid | -0.03 | -0.07* | -0.03 | ||||
| Drinking | -0.21*** | -0.01 | 0.09** | 0.08* | |||
| Smoking | -0.30*** | -0.01 | -0.01 | 0.07* | 0.29*** | ||
| Stigma | 0.16*** | 0.14*** | 0.08* | -0.16*** | -0.18*** | -0.14*** | |
| Discrimination | 0.05 | 0.10** | 0.16*** | -0.06 | -0.05 | -0.07* | 0.42*** |
Table┬Ā4.
| Variable |
Stigma |
Discrimination |
|||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | ||
| Gender | |||||||
| Man | 1.000 | 1.000 | |||||
| Woman | 2.087 | 1.295-3.362 | 0.003** | 0.968 | 0.690-1.358 | 0.850 | |
| Age | |||||||
| 19-39 yr | 1.000 | 1.000 | |||||
| Ōēź40 yr | 1.939 | 1.270-2.962 | 0.002** | 1.185 | 0.856-1.639 | 0.306 | |
| Monthly income | |||||||
| 1,990,000-3,990,000 KRW | 1.000 | 1.000 | |||||
| Ōēź4,000,000 KRW | 1.150 | 0.751-1.763 | 0.520 | 1.989 | 1.444-2.739 | <0.001*** | |
| Opioid (narcotic) analgesics misuse | |||||||
| Yes | 1.000 | 1.000 | |||||
| No | 8.172 | 2.481-26.920 | 0.001** | 1.184 | 0.384-3.648 | 0.768 | |
| Drinking | |||||||
| Yes | 1.000 | 1.000 | |||||
| No | 1.269 | 0.762-2.113 | 0.360 | 1.102 | 0.774-1.570 | 0.590 | |
| Smoking | |||||||
| Yes | 1.000 | 1.000 | |||||
| No | 2.011 | 1.240-3.259 | 0.005** | 1.608 | 1.083-2.386 | 0.018* | |
| Therapeutic effect | 1.364 | 0.890-2.091 | 0.154 | 1.374 | 0.998-1.893 | 0.052 | |
| Medical treatment | 1.998 | 1.250-3.193 | 0.004** | 1.105 | 0.752-1.626 | 0.611 | |
| Government support | 8.251 | 1.100-61.914 | 0.040* | 2.598 | 0.991-6.807 | 0.052 | |
| Causes of addiction | |||||||
| 1. Character, will, and bad habits | 1.388 | 0.898-2.147 | 0.140 | 1.223 | 0.885-1.691 | 0.222 | |
| 2. Mental illness, loss of brain control | 1.000 | 1.000 | |||||
REFERENCES







