 |
 |
- Search
| Psychiatry Investig > Volume 20(5); 2023 > Article |
|
Abstract
Objective
This study aimed to evaluate the consistency or stability of mental disorders diagnosed in the psychiatry ward setting, investigate factors associated with consistency, and observe the disease distribution over the decade.
Methods
A total of 20,359 psychiatric inpatients were included in this retrospective study from June 2011 to December 2020. Diagnoses from the first admission to discharge were evaluated to determine the diagnostic consistency during hospitalization. Readmissions were selected as the subgroup, whose first and last discharge diagnoses were compared to analyze the relatively long-term diagnostic stability. Demographic and clinical characteristics were collected to identify predictors of diagnostic discrepancy.
Results
From 2011-2020, the hospitalization rate decreased from 42.7% to 20.7% for schizophrenia and grew from 13.3% to 23.8% for depression. Diagnoses were retained by 92.6% of patients at their first discharge diagnosis, ranging from 100% for disorders of psychological development to 16.3% for unspecified mental disorders. About 33.9% of diagnostic conversions were to bipolar disorder in patients having inconsistent diagnoses. However, among rehospitalizations, the diagnostic stability notably dropped to 71.3%. For rehospitalizations, mood disorders and schizophrenia spectrum disorders were relatively stable diagnoses categories, with 72.6% to 76.7% of patients receiving the same diagnosis, although results of specified diagnoses within these categories ranged from 5.9% to 91.0%. Except for mood disorders and schizophrenia spectrum disorders, the diagnoses of all other categories were below 70%. Long lengths of hospitalization and old age were associated with short-term diagnosis alterations.
Diagnosis stability is critical in disease research and clinical practice. Currently, due to the lack of objective and effective biomarkers [1], the final diagnosis of mental disorders can only be made by integrating multiple sources of information from the perspective of symptomatology under the nosology guidance of mainstream diagnostic criteria or manuals, like the ICD (the International Classification of Diseases Version) or DSM (The Diagnostic and Statistical Manual of Mental Disorder). In this situation, the accuracy of diagnosis highly depends on the effectiveness of the diagnostic criteria and the clinical level of physicians.
Maintaining high stability in clinical diagnosis is a challenge. In the fact, most psychiatric symptoms are not specific to one particular disorder and one symptom may exist in a variety of diseases given the complexity of the mental disorder [2], which may increase the degree of clinical diagnosis uncertainty. When comorbid with other diseases, such as substance use [3,4] and organic disease [5], the stability of diagnosis will be affected. The length of the duration also means a lot to it. The notion of differentiation in functional psychosis was proposed in previous studies [6,7], which revealed that clinical manifestations may become clearer as time passed.
Consistent diagnosis, as a cornerstone, promotes the progress of the diseases research field. Accurate disease classification contributes to revealing the genetic and pathophysiological mechanisms of the disease [6,7], and diagnosis misclassification affected the genetic pattern of psychiatric research [8]. Meanwhile, the discovery of biological dysfunction plays positive feedback on diagnostic stability, which would improve early diagnosis and provide personalized effective treatment [9]. For patients, inconsistent diagnosis can give rise to delays in treatment, unnecessary tests, increased care costs, poor prognosis, and negative hospital impacts [10,11].
The admission diagnosis is a hypothesis, based on the patientŌĆÖs problems and the physicianŌĆÖs experience, which will be tested by the clinician during hospitalization. Usually, complete information collected (like psychological, relevant physical examinations, neurological, psychopharmacological evaluations, observations and responses in the milieu, and more clinical interviews with the patient and his parents) after admission will often help the clinician to confirm their hypothesis [12]. Therefore, during hospitalization, additional evidence gathered about the patientŌĆÖs mental symptoms, physical condition, and other social factors can change the diagnosis. However, to our knowledge, few studies have focused on diagnostic stability during short-term hospitalization, even though an accurate and stable diagnosis was essential to patientsŌĆÖ prognosis and disease research field.
Hence, considering the implications of diagnostic inconsistencies to clinical practice and the development of disciplinary research, we conducted a retrospective study of psychiatric inpatients based on the International Classification of Diseases Version 10 (ICD-10) code from 2011 to 2020. The purpose of this study was to evaluate: 1) the diagnostic distribution of first admissions in the past decade; 2) the diagnostic consistency between first admission and discharge, the readmission diagnostic stability; and 3) potential predictors of discrepant diagnosis in short hospitalization.
This study was executed at the Second Xiangya Hospital of Central South University, China. Established in 1958, the Second Xiangya hospital was one of the largest general hospitals in China, which has the top psychiatry department in China, and there are a large number of difficult cases from all over the country per year. In addition, as a large comprehensive grade-A hospital, it can provide authoritative and standard diagnoses and treatments.
All patient data were collected from non-emergency admission between June 2011 and December 2020, which recorded patient admission and discharge dates, diagnoses, and procedures. Each patient had an exclusive admission number that did not change by the number of hospitalizations. We excluded patients without diagnostic information, and further excluded patients who were hospitalized for less than two days, because psychiatrists may not have enough time and adequate evidence to make reliable diagnoses. In the end, a total of 20,359 patients were included in our study. Of 20,359 patients, 3,762 (18.5%) were hospitalized more than once, with an average interval of 1.7 years between their first and last admission.
All admission and discharge diagnoses were finished by two or three psychiatrists with specialty training in psychiatry using the ICD-10 [13]. It was generally considered that discharge diagnosis is more definitive and reliable than admission diagnosis, so only discharge diagnosis will be used to observe the distribution of mental disorders in this study.
The present study received approval by the Human Research and Ethics Committee of Second Xiangya Hospital, Central South University, China (2022033, jsjbtzdx). The board waived off the requirement for patient informed consent in this retrospective study because of the anonymous nature of the data. All methods were performed following the relevant guidelines and regulations.
After analyzing the demographic characteristics of patients, the distribution and discrepancy of diagnosis were measured. The consistency of short-term diagnosis was assessed by analyzing the first admission and discharge diagnoses of 20,359 patients. In addition, rehospitalizations were selected as a subgroup, and their first and last discharge diagnoses were compared to determine the relatively long-term diagnostic stability.
In the present study, the consistency of diagnoses was compared according to the first two-digit of the mental illness ICD-10 code (Fxx.). Due to fewer samples and the scattered distribution of some diagnoses categories, these diseases were grouped into a broad category, e.g., F8x (Disorder of psychological development). For the case of more than one admission diagnosis, only the principal diagnoses of admission and discharge were compared to study the consistency. The principal diagnosis was often defined as a ŌĆ£lifetimeŌĆØ diagnosis. For example, if a patient was admitted with a diagnosis of bipolar affective disorder (BD) and nonorganic insomnia, but discharged with the diagnosis of BD, we would compare the main diagnoses ŌĆ£BDŌĆØ and still consider the diagnoses to be consistent. For readmission patients, their discharge diagnosis was compared using the same criteria mentioned above. Besides, the frequencies of discrepant diagnoses were tabulated.
Data management and analysis were performed in IBM SPSS 25.0 (IBM Corp., Armonk, NY, USA). The results of continuous and categorical variables were presented as mean┬▒ standard deviations and percentages, respectively. T-test was used for two normal independent samples and the rank-sum test was used for non-normal samples to compare age, length of stay (LOS), etc. between the diagnostic consistency and inconsistency groups. The chi-square test was conducted for categorical variables. After that, a binary logistics regression analysis prediction model was used to identify predictors of diagnostic discrepancy. Age, gender, marital status, occupation, LOS, and comorbidities of physical diseases were used as predictors of the model. All p values were bilateral, and p<0.05 was considered statistically significant.
The demographic characteristics of the sample were presented in Table 1. The mean age was 25.1 (standard deviation [SD] 9.2) years old and 55.5% were female at their first admission. The mean LOS was 18.9 (SD 10.9) days. The most prevailing comorbidities in this study were cardiovascular system and glucose metabolism diseases, of which hypertension was the most common.
Among 20,359 subjects, 36.3% of the patients had schizophrenia (SCZ) spectrum diagnosis, including 85.9% for SCZ, 7.5% for the acute and brief psychotic disorder (ATPD), 3.8% for unspecified nonorganic psychosis, 1.6% for persistent delusion disorder, and 1.3% for schizoaffective disorder (SAD). The 19.7% of the patients were diagnosed with BD, 19.2% with depression, and 15.8% with neurotic-stress-related and somatoform disorders (NSRD), as well as other mental disorder percentages were shown in Figure 1.
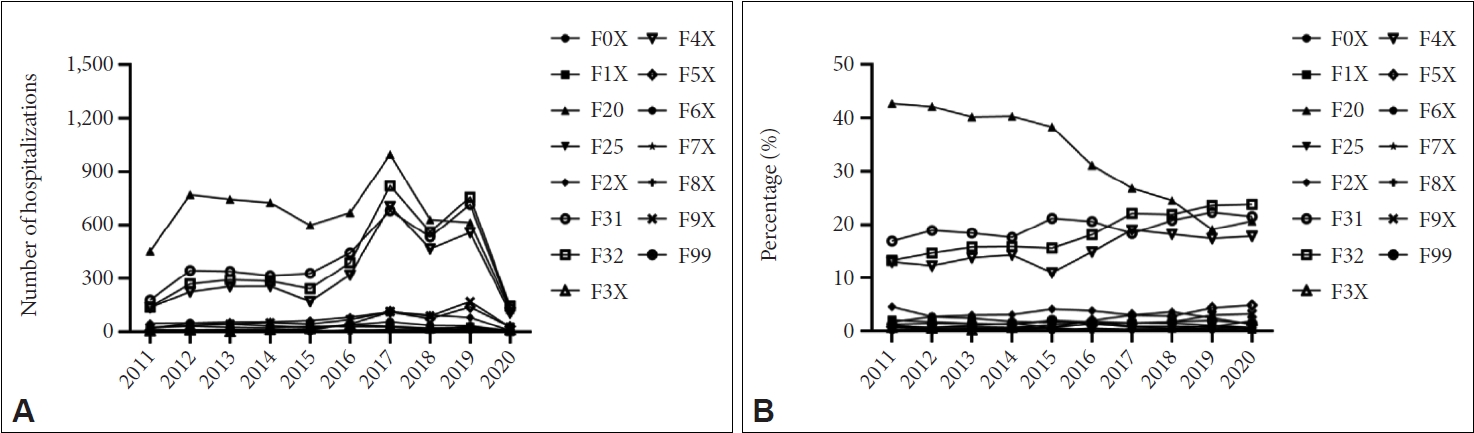
According to Figure 2, despite the rising number of admission patients with schizophrenia since 2011 (except in 2020, the ward was closed due to the coronavirus outbreak), the percentage of annual psychiatric inpatients with SCZ constantly dropped from 42.7% to 20.7% from 2011 to 2020. In contrast, hospitalization rates for depression grew from 13.3% to 23.8%, BD increased slowly from 16% to 21.6%, and NSRD raised from 13% to 17.8% (Figure 2B).
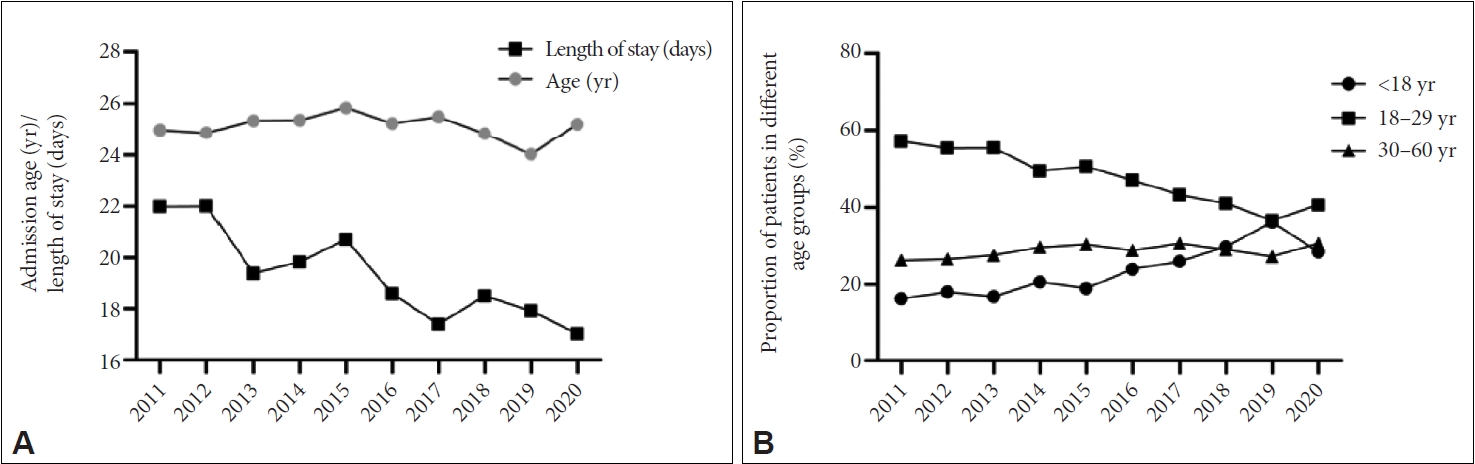
In Figure 3, the average hospital age of patients changed slightly from 2011 to 2020, but hospitalization rates significantly changed for different age groups (Figure 3B). Hospitalization rates among adolescents increased from 16.4% in 2011 to 36.4% in 2019, while hospitalization proportions among 18-29 year-olds decreased from 57.2% to 36.6%, and hospitalization proportions among 30-60 year-olds showed a small increase. Meanwhile, the average LOS decreased from 22 days in 2011 to 17 days in 2020.
In short term, of 20,359 admissions, 92.6% of patients were diagnosed consistently between first admission and discharge. Table 2 gives a brief overview. Disorders of psychological development (such as child autism and AspergerŌĆÖs syndrome), substance use, and NSRD had the highest consistency, at 100%, 97.4%, and 96.5%, respectively. ŌĆ£Unspecified mental disordersŌĆØ (F99) diagnosis was unstable during admission, with the lowest consistency of 16.3%. Most diagnoses are ambiguous until a disease was identified. The consistency of the three most prevailing psychosis was 94.4% for SCZ, 96.4% for BD, and 94.1% for depression.
In long term, among 3,762 readmission patients, 71.3% of patients received the same diagnosis at their first and last discharge diagnosis. The rate of diagnostic consistency varied widely among readmissions which ranged from 91.0% for bipolar disorder to 9.5% for unspecified mental disorders. The diagnosis consistency of SCZ and depression was 86.8% and 55.9%, respectively. However, except for mood disorder and SCZ spectrum categories had the highest consistency at 76.7% and 72.6%, respectively, the diagnoses of all other categories were below 70%.
The diagnostic consistency of all psychiatric categories in rehospitalizations was significantly lower than the consistency of diagnosis in first-admission inpatients.
The relatively short-term and long-term discrepancies between initial and final diagnoses across multiple diagnosis categories were detailed (Supplementary Table 1 and 2 in the online-only Data Supplement).
Of 20,359 subjects of first admissions in short-term hospitalization, 1,490 (7.4%) patients presented substantial diagnostic conversion. Among all inconsistent diagnoses, the main admission diagnoses were SCZ at 23.9%, unspecified mental disorders at 17.2%, and depression at 15.7% (Supplementary Table 1 in the online-only Data Supplement).
Diagnoses shifted to BD were most frequent, accounting for 33.9% of patients having diagnostic switches. The proportion of the patients whose diagnoses were converted to BD was 33.1% (168) from depression, 29.5% (150) from SCZ, 9.3% (47) from unspecified mental disorders, and 28.1% (142) from other mental disorders.
Besides, frequent diagnostic conversion to SCZ was mainly from ATPD at 33.6% and BD at 21.2%. Notably, there were 40 of 257 patients diagnosed with unspecified mental disorders shifted into SCZ. Conversely, no patients were initially diagnosed with SCZ shifting into unspecified mental disorder. The majority of patients admitted with unspecified psychosis diagnosis mainly turned to SCZ spectrum (34.6%), mood disorder (30%), and organic disorder (19%), followed by NSRD (8.2%).
In the subgroup, 28.7% (1,078 of the 3,762) rehospitalizations occurred during diagnosis conversion. In patients with discrepant diagnoses, the most common initial diagnosis was depression at 34.2%, followed by SCZ at 13.8% (Supplementary Table 2 in the online-only Data Supplement).
Similar to the characteristic of diagnostic discrepancy of first admission patients, diagnoses shifted to BD were most frequently (40.2%), followed by SCZ (21.6%). Diagnostic conversion to BD was mainly from depression (46.4%) and SCZ (12.1%). The diagnostic inconsistency of ATPD was 94.1% and 60.3% of ATPD eventually shifted to SCZ. ATPD was the most common disease revised to SCZ. Among 19 rehospitalizations diagnosed with SAD, 7 (24%) shifted to SCZ and 9 (32%) shifted to BD. Most unspecified psychosis eventually turned to SCZ and BD. These patients whose baseline diagnosis was NSRD mainly converted to mood disorders (66.4%).
In terms of years, the overall consistency of psychiatric diagnoses was 92.1% to 94.9% from 2011 to 2019, and 88.5% in 2020 (Supplementary Figure 1 in the online-only Data Supplement).
To determine predictors in a diagnostic shift during a short hospitalization, first-admission patients were divided into two groups according to whether the diagnosis was consistent. By comparing the LOS, age, gender, marital status, occupation, and co-morbidity of physical diseases between the two groups, significant differences were found in the LOS (Z=-7.57, p<0.001) and mean age (Z=12.40, p<0.001). LOS increased with inconsistent diagnoses (mean 21.1 days as compared to mean 18.9 days without discrepant diagnoses). The mean age of the discrepant group was 22.1 (SD 8.3) years old compared with 25.3 (SD 9.2) years old of the consistent group. Then, stepwise logistic regression analysis was used to analyze the predictor of diagnoses discrepancy. The LOS and age were independent predictors of a diagnosis of shifts (Table 3).
This retrospective study covered 20,359 inpatients (3,762 of which were rehospitalizations) from 2011 to 2020 and investigated the distribution and diagnostic consistency of mental disorders. The results found that three major mental disorders remain the leading cause of hospitalization. During short-term hospitalization, most mental disorder diagnoses were highly stable, however, among rehospitalizations, the diagnostic consistency of all mental illness categories was strikingly decreased. Meanwhile, LOS and age were major predictors of inconsistent diagnosis.
Our results showed that despite the number of SCZ patients increasing [14], hospitalization rates for SCZ had noticeably decreased each year in our findings. Conversely, hospitalization rates for BD and depression were both on the rise. In line with previous studies, admission rates for SCZ decreased while mood disorders increased in Taiwan from 1998 to 2007 [15]. Twenge et al. [16] also reported that the proportion of inpatients with mood disorders has been increasing [17]. Notably, the decade development of community-based mental health services has contributed to substantial improvements in the early recognition of mental illness, the immediate treatment rates of patients, the continuity of treatment, and personalized rehabilitation [18]. Thus, patients with stable serious mental disorders will receive effective intervention and treatment in community hospitals, which may account for the decreased hospitalization rates for SCZ in general hospitals.
When patients were divided into age groups, we found the proportion of adolescents hospitalized significantly increased every year. Recent surveys reported that the proportion of mood disorders relative to all psychiatric was increased among children and adolescents [19,20], which might be one possible reason for the young age of this sample. Besides, most adult mental disorders began in adolescence [21,22], and with improving mental health awareness in general, mental illness was identified and treated at an early stage.
Moreover, consistent with previous reports [23,24], a notable finding was the mean LOS decreased by 5 days during the last decade. On the one hand, it was reported that the hospitalization time for mood disorders was shorter than that of SCZ [25,26]. With the increase in the effectiveness of antipsychotics and related psychological or physical interventions [27], hospital treatment times were shorted given the rapid recovery of patients. On the other hand, previous studies have reported the impact of healthcare reform on the LOS [6,28,29]. It is worth mentioning that, to promote the realization of the international UHC (universal health coverage) goals, which means all individuals and communities have access to the health services they need without suffering financial hardship, China has launched a series of healthcare reforms since 2009. In 2018, more than 95% of the population was covered by health insurance [30]. Zhou et al. [31] found that insurance plans with lower co-payments were predictors of longer hospital stays. Gao et al. [32] reported that the payment reform reduced the LOS by 17.7% but did not affect the quality of care. Therefore, changes in these measures may have a substantial impact on reducing the LOS. Despite this, some studies reported that shorter hospital stays were associated with the number of rehospitalizations [33,34], whereas discordant views reported that shorter hospital stays did not affect patient quality of care and were not directly associated with readmission [23,35,36].
In our results, the 10-year overall cumulative rate of conversion to another mental illness among first admissions in this general hospital was 7.3%, which confirmed a high degree of diagnostic consistency during short-term hospitalization. However, for patients who were hospitalized at least twice, 28.7% had diagnostically switched in their last discharge diagnosis. This time-mediated instability may be more reflective of the natural transformation of the mental disease.
Consistent with the results of previous studies, diagnostic discrepancies were high in unspecified psychosis [37-39] and ATPD [40-42]. A significant proportion of patients with unspecified psychosis shifted to the SCZ spectrum and mood disorder classifications. ATPD was the most common disorder converted to SCZ, followed by bipolar disorder among the first and repeated hospitalizations. These findings provided new evidence for the idea of a differentiated process in functional psychosis, that clarity and stability of clinical images would get increased with the decreasing of comorbidity and atypical symptoms over time and consequently contribute to a more definitive diagnosis [43]. Therefore, it is more meaningful to expand the longitudinal sample and find potential predictors of the transition from other functional psychosis to the SCZ spectrum or affective psychosis [44].
Our findings showed cross-conversion between SCZ, SAD, and mood disorder. The diagnostic stability of depression and SAD among the readmissions were 55.9% and 32.1%, respectively, still, which were above 85% among the first admission. The 24% of readmissions with depression developed BD in our study that in line with previous studies reported unipolar depression frequently developed into BD [45-47]. Previous reports have illustrated these disorders were difficult to identify when there was a significant overlap of symptoms [48,49]. In clinical practice, both prominent psychotic symptoms and affective symptoms may occur in a person at the same time, which may confuse clinicians hard to find a clear boundary to making a pure SCZ or mood disorder. Since the lack of a clear boundary between SCZ and mood disorders, Jacob Kasanin proposed a hybrid concept, SAD [50]. However, 32% of readmissions with SAD converted to BD and 24% to SCZ in this study. Thus, emphasis should be placed on the classification and revisioning of criteria among mood disorders, SAD, and SCZ.
Nevertheless, we found the rate of short-term hospitalization misdiagnosis fluctuated by less than 2.5% (except compared with 2020) despite vast scientific and technological advances in medicine over the last decade. This result may be related to the natural evolution of certain disorders and also underscores the inherent weaknesses in the diagnostic classification system. The introduction of comprehensive diagnostic criteria and so-called ŌĆ£operational definitionsŌĆØ of these criteria in DSM-III since the 1980s has valuably improved the reliability of psychiatric diagnostics [51]. However, the limitations of this approach have become increasingly apparent. Due to the interdisciplinary nature of psychiatry, the operationalism of psychiatric diagnosis simplifies the diagnostic process, making the assessment of subjective experience almost excluded and undervalued on the theoretical level, further affecting the validity and heterogeneity of diagnosis [52,53]. Especially for disorders only with short follow-up, it is difficult for psychiatrists to reach the right diagnosis in enough time or to combine humanistic and environmental factors, leading to inappropriate treatment or intervention [54]. Although to overcome the limitations of empirical classification, the DSM-5 combined the classification approach and the partial adoption of a dimensional approach [55], which clinical utility and diagnostic validity of the new diagnostic classification still needs further evaluation, and person-centered individualized evaluation and multi-level exploration are essential for diagnostic classification.
The interrater reliability of diagnoses is controlled by the subjective experience of each evaluator and the hierarchical differences in communication with the object. It should be noted that in this study the psychiatrists who assigned the diagnosis were not aware of this program in progress, and each diagnosis was determined jointly by two or more psychiatrists with specialty training in psychiatry. This training (including assessment of symptom scales, collection of medical information, and clinical interviews) may partially reduce diagnostic inconsistencies. Therefore, our findings accurately reflect the practical application of diagnostic classification in psychiatric clinical practice.
Patients with inconsistent diagnoses were younger and had longer hospital stays than those with stable diagnoses. Our results showed no significant difference in other demographic characteristics between these two groups. Since children and adolescents were at the peak of the onset of mental disorders and the risk of conversion to other disorders [21,22]. Especially patients and families have a potential influence on doctorsŌĆÖ diagnoses. Clinicians may make a mild admission diagnosis than real symptoms, which affects the stability of the diagnosis. This reminds psychiatrists to pay more attention and be more cautiously on young patients when making diagnoses. Longer hospital stays and younger age were associated with increased odds of diagnosis alteration, this result validates the findings of previous studies [56], suggesting that inconsistent diagnosis increases inpatient care costs and may result in delays in treatments or interventions. Therefore, systematically identifying misdiagnosis and reducing diagnosis delay is conducive to the rehabilitation of patients.
Uncommon mental disorders should also get our focus. In the past period, most studies had focused on changes in a single disease category such as SCZ [7,8], BD [9-11], and personality disorder [12,13], but our study included uncommon diagnostic classifications. For example, NSRD was ever shifted to BD. These inconsistencies may be related to comorbidity, which increased diagnostic complexity. Thus, cliniciansŌĆÖ comprehensive observations and evaluations of symptoms were still important means to determine the correct trend of the disease.
Also, our study has certain limitations. Firstly, the study only compared inpatient changes in a single environment, further research needs to be expanded to other settings. Secondly, affected by the quality of documents, there may be some deviation in diagnosis in different periods. However, this research center has a strict medical record management system, and two or more doctors make diagnoses simultaneously, so the samples in this retrospective study are of high quality and representativeness. Finally, it is necessary to compare more characteristics of patients between the diagnoses consistent group and discrepant group to find out the related factors that may affect the accuracy of diagnosis.
In summary, our results proved that ICD-10 has high diagnostic stability in hospitalized patients, but it still shows some inherent limitations when the diagnosis needs to be made in a long-term follow-up. Further training in clinical assessment and proper revision of diagnostic criteria could be beneficial.
Supplementary Materials
The online-only Data Supplement is available with this article at https://doi.org/10.30773/pi.2022.0349.
Supplementary┬ĀTable┬Ā1.
Cross-tabulation of admission and discharge ICD-10 discrepancy diagnosis in patients (N=1,490)
Supplementary┬ĀTable┬Ā2.
Cross-tabulation of discrepancy diagnosis in readmission patients (N=1,078)
Supplementary┬ĀFigure┬Ā1.
Changes in inconsistent rates of psychiatric diagnosis from 2011 to 2020. N, number.
Notes
Availability of Data and Material
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request [JH].
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Furu Liu, Renrong Wu, Ping Shao, Jing Huang. Data curation: Furu Liu, Menghui Gao, Jing Huang. Formal analysis: Furu Liu, Qiongqiong Wu. Project administration: Meiqi Yan, Ping Shao, Jing Huang. Supervision: Ping Shao, Jing Huang. WritingŌĆöoriginal draft: Furu Liu. WritingŌĆöreview & editing: all authors.
Funding Statement
This work was supported by the National Natural Science Foundation of China (Grant No.81622018 and No.82072096).
Figure┬Ā1.
Cumulative percentage of different mental disorders from 2011 to 2020. F0X, organic mental disorders; F1X, mental and behavioral disorders due to psychoactive substance use; F20, schizophrenia; F22, persistent delusional disorders; F23, acute and brief psychotic disorder; F25, schizoaffective disorders; F29, unspecified nonorganic psychosis; F31, bipolar disorder; F32, depression; F33, recurrent depressive disorder; F3X, another mood (affective) disorder; F4X, neurotic, stress-related and somatoform disorders; F5X, behavioral syndromes associated with physiological disturbances and physical factors; F6X, disorders of adult personality and behavior; F7X, mental retardation; F8X, disorders of psychological development; F9X, behavioral and emotional disorders with onset usually occur in childhood and adolescence; F99, unspecified mental disorder; ICD-10, the International Classification of Diseases Version- 10.

Figure┬Ā2.
The number (A) and the annual percentage (B) of hospitalization for different mental disorders from 2011 to 2020. F0X, organic mental disorders; F1X, mental and behavioral disorders due to psychoactive substance use; F20, schizophrenia; F25, schizoaffective disorders; F2X, other schizophrenia spectrum disorders; F31, bipolar disorder; F32, depression; F3X, other mood affective disorders; F4X, neurotic, stress-related and somatoform disorders; F5X, behavioral syndromes associated with physiological disturbances and physical factors; F6X, disorders of adult personality and behavior; F7X, mental retardation; F8X, disorders of psychological development; F9X, behavioral and emotional disorders with onset usually occur in childhood and adolescence; F99, unspecified mental disorder.
Figure┬Ā3.
Mean length of stay and age (A) and different age groups (B) changes in hospitalizations patients from 2011 to 2020.
Table┬Ā1.
Demographic characteristics of patients
Table┬Ā2.
Percentage of diagnostic consistency for first admission patients and rehospitalizations
| ICD-10 code | Total (N=20,359)* |
Diagnostic consistency in first hospitalized patients |
Total (N=3,762)ŌĆĀ |
Diagnostic consistency in repeat hospitalized patients |
|||
|---|---|---|---|---|---|---|---|
| Consistency | Inconsistency | Consistency | Inconsistency | ||||
| Organic, including symptomatic, mental disorders: F00-F09 | 298 | 274 (91.9) | 24 (8.1) | 48 | 22 (45.8) | 26 (54.2) | |
| Substance use related to mental or behavior disorders: F10-F19 | 234 | 228 (97.4) | 6 (2.6) | 31 | 21 (67.7) | 10 (32.3) | |
| Schizophrenia, schizotypal and delusional disorder: F20-F29 | 7,542 | 6,911 (91.6) | 631 (8.4) | 1,323 | 1,015 (76.7) | 308 (23.3) | |
| Schizophrenia: F20 | 6,409 | 6,053 (94.4) | 356 (5.6) | 1,129 | 980 (86.8) | 149 (13.2) | |
| Persistent delusional disorders: F22 | 107 | 102 (95.3) | 5 (4.7) | 19 | 11 (57.9) | 8 (42.1) | |
| Acute and brief psychotic disorder: F23 | 658 | 486 (73.9) | 172 (26.1) | 118 | 7 (5.9) | 111 (94.1) | |
| Schizoaffective disorders: F25 | 80 | 69 (86.3) | 11 (13.8) | 28 | 9 (32.1) | 19 (67.9) | |
| Unspecified nonorganic psychosis: F29 | 288 | 201 (69.8) | 87 (30.2) | 29 | 8 (27.6) | 21 (72.4) | |
| Mood (affective) disorders: F30-F39 | 7,792 | 7,404 (95.0) | 388 (5.0) | 1,794 | 1,302 (72.6) | 492 (27.4) | |
| Bipolar disorder: F31 | 3,642 | 3,510 (96.4) | 132 (3.6) | 898 | 817 (91.0) | 81 (9.0) | |
| Depression: F32 | 3,970 | 3,736 (94.1) | 234 (5.9) | 837 | 468 (55.9) | 369 (44.1) | |
| Recurrent depressive disorder: F33 | 149 | 130 (87.2) | 19 (12.8) | 31 | 13 (41.9) | 18 (58.1) | |
| Another mood (affective) disorder: F3X | 31 | 28 (90.3) | 3 (9.7) | 28 | 4 (14.3) | 24 (85.7) | |
| Neurotic, stress-related, and somatoform disorders: F40-F48 | 3,188 | 3,075 (96.5) | 113 (3.5) | 405 | 265 (65.4) | 140 (34.6) | |
| Behavioral syndromes related to physiological factors: F50-F59 | 472 | 450 (95.3) | 22 (4.7) | 39 | 20 (51.3) | 19 (48.7) | |
| Disorders of adult personality and behavior: F60-F69 | 58 | 55 (94.8) | 3 (5.2) | 8 | 2 (25.0) | 6 (75.0) | |
| Mental retardation: F70-F79 | 103 | 96 (93.2) | 7 (6.8) | 10 | 6 (60.0) | 4 (40.0) | |
| Disorders of psychological development: F80-F89 | 36 | 36 (100.0) | 0 | 6 | 4 (66.7) | 2 (33.3) | |
| Behavioral and emotional disorders with onset usually occur in childhood and adolescence: F90-F98 | 329 | 290 (88.1) | 39 (11.9) | 77 | 27 (32.5) | 52 (67.5) | |
| Unspecified mental disorder: F99 | 307 | 50 (16.3) | 257 (83.7) | 21 | 2 (9.5) | 19 (90.5) | |
| Total | 20,359 | 18,869 (92.6) | 1,490 (7.4) | 3,762 | 2,864 (71.3) | 1,078 (28.7) | |
REFERENCES
1. Kapur S, Phillips AG, Insel TR. Why has it taken so long for biological psychiatry to develop clinical tests and what to do about it? Mol Psychiatry 2012;17:1174-1179.



2. Boschloo L, van Borkulo CD, Rhemtulla M, Keyes KM, Borsboom D, Schoevers RA. The network structure of symptoms of the diagnostic and statistical manual of mental disorders. PLoS One 2015;10:e0137621



3. Pope MA, Joober R, Malla AK. Diagnostic stability of first-episode psychotic disorders and persistence of comorbid psychiatric disorders over 1 year. Can J Psychiatry 2013;58:588-594.



4. Sara GE, Burgess PM, Malhi GS, Whiteford HA, Hall WC. The impact of cannabis and stimulant disorders on diagnostic stability in psychosis. J Clin Psychiatry 2014;75:349-356.


5. Marneros A. Schizophrenic first-rank symptoms in organic mental disorders. Br J Psychiatry 1988;152:625-628.


6. Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. Int J Epidemiol 2002;31:285-293.


7. Henriksen MG, Nordgaard J, Jansson LB. Genetics of schizophrenia: overview of methods, findings and limitations. Front Hum Neurosci 2017;11:322



9. Fond G, dŌĆÖAlbis MA, Jamain S, Tamouza R, Arango C, Fleischhacker WW, et al. The promise of biological markers for treatment response in first-episode psychosis: a systematic review. Schizophr Bull 2015;41:559-573.



10. Schimmelmann BG, Conus P, Edwards J, McGorry PD, Lambert M. Diagnostic stability 18 months after treatment initiation for first-episode psychosis. J Clin Psychiatry 2005;66:1239-1246.


11. Giardina TD, Haskell H, Menon S, Hallisy J, Southwick FS, Sarkar U, et al. Learning from patientsŌĆÖ experiences related to diagnostic errors is essential for progress in patient safety. Health Aff (Millwood) 2018;37:1821-1827.



12. Aronen ET, Noam GG, Weinstein SR. Structured diagnostic interviews and cliniciansŌĆÖ discharge diagnoses in hospitalized adolescents. J Am Acad Child Adolesc Psychiatry 1993;32:674-681.


13. World Health Organization. ICD-10: international statistical classification of diseases and related health problems: tenth revision. 2nd ed. Geneva: World Health Organization; 2004.
14. He H, Liu Q, Li N, Guo L, Gao F, Bai L, et al. Trends in the incidence and DALYs of schizophrenia at the global, regional and national levels: results from the global burden of disease study 2017. Epidemiol Psychiatr Sci 2020;29:e91.



15. Chiang CL, Chen PC, Huang LY, Kuo PH, Tung YC, Liu CC, et al. Time trends in first admission rates for schizophrenia and other psychotic disorders in Taiwan, 1998-2007: a 10-year population-based cohort study. Soc Psychiatry Psychiatr Epidemiol 2017;52:163-173.



16. Twenge JM, Cooper AB, Joiner TE, Duffy ME, Binau SG. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005-2017. J Abnorm Psychol 2019;128:185-199.


17. Blader JC, Carlson GA. Increased rates of bipolar disorder diagnoses among U.S. child, adolescent, and adult inpatients, 1996-2004. Biol Psychiatry 2007;62:107-114.



18. Zhu Y, Li X, Zhao M. Promotion of mental health rehabilitation in China: community-based mental-health services. Consortium Psychiatricum 2020;1:21-27.


19. Sherwood SN, Carlson GA, Freeman AJ. Decreasing rate of inpatient pediatric bipolar disorder diagnosis in the US between 2004 and 2010. Bipolar Disord 2022;24:149-160.



20. Shorey S, Ng ED, Wong CHJ. Global prevalence of depression and elevated depressive symptoms among adolescents: a systematic review and meta-analysis. Br J Clin Psychol 2022;61:287-305.



21. Jones PB. Adult mental health disorders and their age at onset. Br J Psychiatry Suppl 2013;54:s5-s10.


22. Solmi M, Radua J, Olivola M, Croce E, Soardo L, Salazar de Pablo G, et al. Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry 2022;27:281-295.



23. Druss BG, Bruce ML, Jacobs SC, Hoff RA. Trends over a decade for a general hospital psychiatry unit. Adm Policy Ment Health 1998;25:427-435.

24. Ajnakina O, Stubbs B, Francis E, Gaughran F, David AS, Murray RM, et al. Hospitalisation and length of hospital stay following first-episode psychosis: systematic review and meta-analysis of longitudinal studies. Psychol Med 2020;50:991-1001.


25. Huntley DA, Cho DW, Christman J, Csernansky JG. Predicting length of stay in an acute psychiatric hospital. Psychiatr Serv 1998;49:1049-1053.


26. Newman L, Harris V, Evans LJ, Beck A. Factors associated with length of stay in psychiatric inpatient services in London, UK. Psychiatr Q 2018;89:33-43.



27. McCrone P, Singh SP, Knapp M, Smith J, Clark M, Shiers D, et al. The economic impact of early intervention in psychosis services for children and adolescents. Early Interv Psychiatry 2013;7:368-373.


28. Kroneman M, Nagy J. Introducing DRG-based financing in Hungary: a study into the relationship between supply of hospital beds and use of these beds under changing institutional circumstances. Health Policy 2001;55:19-36.


29. Wang H, Zhang L, Yip W, Hsiao W. An experiment in payment reform for doctors in rural China reduced some unnecessary care but did not lower total costs. Health Aff (Millwood) 2011;30:2427-2436.


30. Tao W, Zeng Z, Dang H, Lu B, Chuong L, Yue D, et al. Towards universal health coverage: lessons from 10 years of healthcare reform in China. BMJ Glob Health 2020;5:e002086.



31. Zhou Y, Rosenheck RA, He H. Health insurance in China: variation in co-payments and psychiatric hospital utilization. J Ment Health Policy Econ 2014;17:25-32.

32. Gao C, Xu F, Liu GG. Payment reform and changes in health care in China. Soc Sci Med 2014;111:10-16.


33. Tadesse S, Gizaw AT, Abraha GK, Gebretsadik LA. Patterns of psychiatric admissions and predictors of patientŌĆÖs outcome in Jimma University Teaching and Referral Hospital: a retrospective study. Int J Ment Health Syst 2017;11:41




34. Capdevielle D, Ritchie K, Villebrun D, Boulenger JP. [Schizophrenic patientsŌĆÖ length of stay: clinical factors of variability and consequences]. Encephale 2009;35:90-96. French.

35. Ries RK, Russo J, Wingerson D, Snowden M, Comtois KA, Srebnik D, et al. Shorter hospital stays and more rapid improvement among patients with schizophrenia and substance disorders. Psychiatr Serv 2000;51:210-215.


36. Smith P, Nicaise P, Giacco D, Bird VJ, Bauer M, Ruggeri M, et al. Use of psychiatric hospitals and social integration of patients with psychiatric disorders: a prospective cohort study in five European countries. Soc Psychiatry Psychiatr Epidemiol 2020;55:1425-1438.




37. Addington J, Chaves A, Addington D. Diagnostic stability over one year in first-episode psychosis. Schizophr Res 2006;86:71-75.


38. Amin S, Singh SP, Brewin J, Jones PB, Medley I, Harrison G. Diagnostic stability of first-episode psychosis. Comparison of ICD-10 and DSMIII-R systems. Br J Psychiatry 1999;175:537-543.


39. Schwartz JE, Fennig S, Tanenberg-Karant M, Carlson G, Craig T, Galambos N, et al. Congruence of diagnoses 2 years after a first-admission diagnosis of psychosis. Arch Gen Psychiatry 2000;57:593-600.


40. Castagnini A, Bertelsen A, Berrios GE. Incidence and diagnostic stability of ICD-10 acute and transient psychotic disorders. Compr Psychiatry 2008;49:255-261.


41. Queirazza F, Semple DM, Lawrie SM. Transition to schizophrenia in acute and transient psychotic disorders. Br J Psychiatry 2014;204:299-305.


42. J├Ėrgensen P, Bennedsen B, Christensen J, Hyllested A. Acute and transient psychotic disorder: a 1-year follow-up study. Acta Psychiatr Scand 1997;96:150-154.


43. McGorry PD. The influence of illness duration on syndrome clarity and stability in functional psychosis: does the diagnosis emerge and stabilise with time? Aust N Z J Psychiatry 1994;28:607-619.



44. Chang WC, Pang SL, Chung DW, Chan SS. Five-year stability of ICD-10 diagnoses among Chinese patients presented with first-episode psychosis in Hong Kong. Schizophr Res 2009;115:351-357.


45. Baryshnikov I, Sund R, Marttunen M, Svirskis T, Partonen T, Pirkola S, et al. Diagnostic conversion from unipolar depression to bipolar disorder, schizophrenia, or schizoaffective disorder: a nationwide prospective 15-year register study on 43 495 inpatients. Bipolar Disord 2020;22:582-592.



46. Musliner KL, ├śstergaard SD. Patterns and predictors of conversion to bipolar disorder in 91 587 individuals diagnosed with unipolar depression. Acta Psychiatr Scand 2018;137:422-432.



47. ├śstergaard SD, Straszek S, Petrides G, Skadhede S, Jensen SO, MunkJ├Ėrgensen P, et al. Risk factors for conversion from unipolar psychotic depression to bipolar disorder. Bipolar Disord 2014;16:180-189.


48. Jabben N, Arts B, Krabbendam L, van Os J. Investigating the association between neurocognition and psychosis in bipolar disorder: further evidence for the overlap with schizophrenia. Bipolar Disord 2009;11:166-177.


49. OConghaile A, DeLisi LE. Distinguishing schizophrenia from posttraumatic stress disorder with psychosis. Curr Opin Psychiatry 2015;28:249-255.


50. J├żger M, Haack S, Becker T, Frasch K. Schizoaffective disorder--an ongoing challenge for psychiatric nosology. Eur Psychiatry 2011;26:159-165.


51. Fuchs T. Subjectivity and intersubjectivity in psychiatric diagnosis. Psychopathology 2010;43:268-274.



52. Andreasen NC. DSM and the death of phenomenology in america: an example of unintended consequences. Schizophr Bull 2007;33:108-112.


53. Modestin J, Huber A, Satirli E, Malti T, Hell D. Long-term course of schizophrenic illness: BleulerŌĆÖs study reconsidered. Am J Psychiatry 2003;160:2202-2208.


- TOOLS







