 |
 |
- Search
| Psychiatry Investig > Volume 19(8); 2022 > Article |
|
Abstract
Objective
Methods
Results
Conclusion
Supplementary Materials
Supplementary Table 1.
Supplementary Figure 1.
Supplementary Figure 2.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Tak Kyu Oh, In-Ae Song. Data curation: Hye Yoon Park. Formal analysis: Tak Kyu Oh, In-Ae Song. Investigation: In-Ae Song. Methodology: Tak Kyu Oh. Project administration: Tak Kyu Oh, In-Ae Song. Resources: Hye Yoon Park. Software: Tak Kyu Oh, In-Ae Song. Supervision: In-Ae Song. Validation: Hye Yoon Park. Writing—original draft: Tak Kyu Oh. Writing—review & editing: In-Ae Song, Hye Yoon Park.
Funding Statement
None
Figure 1.
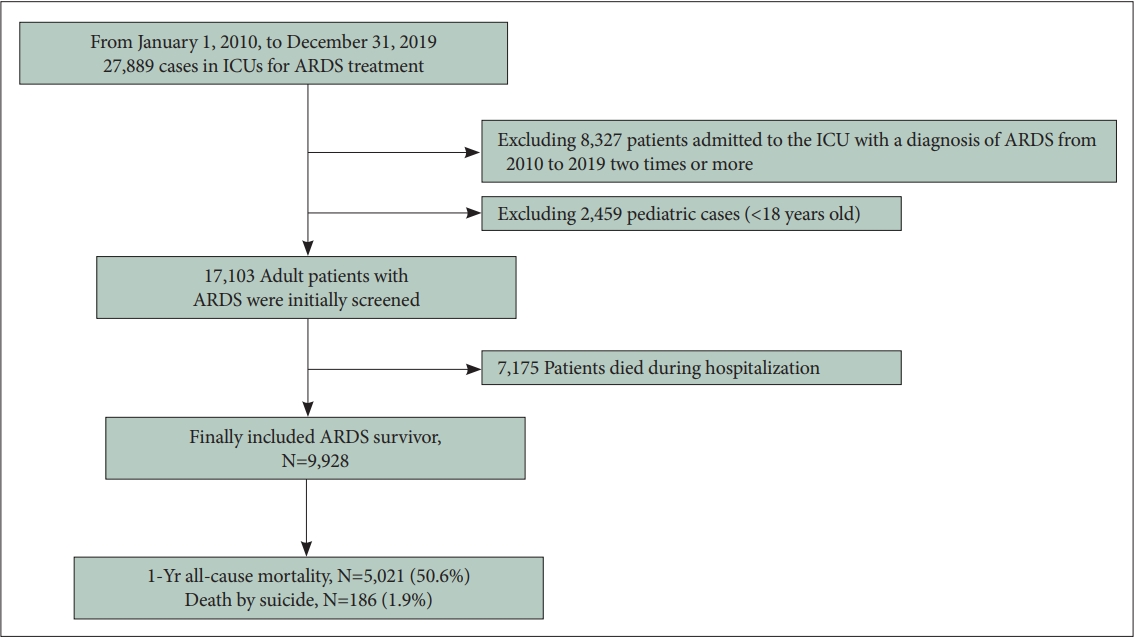
Table 1.
Values are presented as mean±standard deviation or number (%).
ARDS, acute respiratory distress syndrome; IM, internal medicine; USD, United States Dollar; CCI, Charlson comorbidity index; ECMO, extracorporeal membrane oxygenation; NMB, neuromuscular blockade; CRRT, continuous renal replacement therapy; CPR, cardiopulmonary resuscitation; PTSD, post-traumatic stress disorder
Table 2.
Values are presented as mean±standard deviation or number (%). ARDS, acute respiratory distress syndrome; IM, internal medicine; USD, United States Dollar; CCI, Charlson comorbidity index; ECMO, extracorporeal membrane oxygenation; NMB, neuromuscular blockade; CRRT, continuous renal replacement therapy; CPR, cardiopulmonary resuscitation; PTSD, post-traumatic stress disorder
Table 3.
ARDS, acute respiratory distress syndrome; HR, hazard ratio; CI, confidence interval; IM, internal medicine; USD, United States Dollar; CCI, Charlson comorbidity index; ECMO, extracorporeal membrane oxygenation; NMB, neuromuscular blockade; CRRT, continuous renal replacement therapy; CPR, cardiopulmonary resuscitation; PTSD, post-traumatic stress disorder
REFERENCES
- TOOLS







