1. Klein DF, Ross DC, Cohen P. Panic and avoidance in agoraphobia. Application of path analysis to treatment studies. Arch Gen Psychiatry 1987;44:377-385.


2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (5th ed). Arlington, VA: American Psychiatric Association; 2013.
3. Başoğlu M, Marks IM, Kiliç C, Swinson RP, Noshirvani H, Kuch K, et al. Relationship of panic, anticipatory anxiety, agoraphobia and global improvement in panic disorder with agoraphobia treated with alprazolam and exposure. Br J Psychiatry 1994;164:647-652.


4. Carleton RN, Sharpe D, Asmundson GJ. Anxiety sensitivity and intolerance of uncertainty: requisites of the fundamental fears? Behav Res Ther 2007;45:2307-2316.


5. Freeston MH, Rhéaume J, Letarte H, Dugas MJ, Ladouceur R. Why do people worry? Pers Individ Differ 1994;17:791-802.

6. Boelen PA, Reijntjes A. Intolerance of uncertainty and social anxiety. J Anxiety Disord 2009;23:130-135.


7. Carleton RN, Collimore KC, Asmundson GJ. “It’s not just the judgement--It’s that I don’t know”: intolerance of uncertainty as a predictor of social anxiety. J Anxiety Disord 2010;24:189-195.

8. Counsell A, Furtado M, Iorio C, Anand L, Canzonieri A, Fine A, et al. Intolerance of uncertainty, social anxiety, and generalized anxiety: differences by diagnosis and symptoms. Psychiatry Res 2017;252:63-69.


9. Fetzner MG, Horswill SC, Boelen PA, Carleton RN. Intolerance of uncertainty and PTSD symptoms: exploring the construct relationship in a community sample with a heterogeneous trauma history. Cogn Ther Res 2013;37:725-734.


10. Oglesby ME, Boffa JW, Short NA, Raines AM, Schmidt NB. Intolerance of uncertainty as a predictor of post-traumatic stress symptoms following a traumatic event. J Anxiety Disord 2016;41:82-87.


11. Tolin DF, Abramowitz JS, Brigidi BD, Foa EB. Intolerance of uncertainty in obsessive-compulsive disorder. J Anxiety Disord 2003;17:233-242.


12. Sarawgi S, Oglesby ME, Cougle JR. Intolerance of uncertainty and obsessive-compulsive symptom expression. J Behav Ther Exp Psychiatry 2013;44:456-462.


13. Carleton RN, Mulvogue MK, Thibodeau MA, McCabe RE, Antony MM, Asmundson GJ. Increasingly certain about uncertainty: intolerance of uncertainty across anxiety and depression. J Anxiety Disord 2012;26:468-479.


14. Carleton RN, Duranceau S, Freeston MH, Boelen PA, McCabe RE, Antony MM. “But it might be a heart attack”: intolerance of uncertainty and panic disorder symptoms. J Anxiety Disord 2014;28:463-470.


15. Bar-Haim Y, Lamy D, Pergamin L, Bakermans-Kranenburg MJ, van IJzendoorn MH. Threat-related attentional bias in anxious and nonanxious individuals: a meta-analytic study. Psychol Bull 2007;133:1-24.


16. Hazlett-Stevens H, Borkovec TD. Interpretive cues and ambiguity in generalized anxiety disorder. Behav Res Ther 2004;42:881-892.


17. Richards JC, Austin DW, Alvarenga ME. Interpretation of ambiguous interoceptive stimuli in panic disorder and nonclinical panic. Cogn Ther Res 2001;25:235-246.
20. Shankman SA, Gorka SM, Nelson BD, Fitzgerald DA, Phan KL, O’Daly O. Anterior insula responds to temporally unpredictable aversiveness: an fMRI study. Neuroreport 2014;25:596-600.


21. Simmons A, Matthews SC, Paulus MP, Stein MB. Intolerance of uncertainty correlates with insula activation during affective ambiguity. Neurosci Lett 2008;430:92-97.


22. Krain AL, Gotimer K, Hefton S, Ernst M, Castellanos FX, Pine DS, et al. A functional magnetic resonance imaging investigation of uncertainty in adolescents with anxiety disorders. Biol Psychiatry 2008;63:563-568.


23. Schienle A, Köchel A, Ebner F, Reishofer G, Schäfer A. Neural correlates of intolerance of uncertainty. Neurosci Lett 2010;479:272-276.


24. Gorman JM, Kent JM, Sullivan GM, Coplan JD. Neuroanatomical hypothesis of panic disorder, revised. Am J Psychiatry 2000;157:493-505.


25. Bang M, Park YW, Eom J, Ahn SS, Kim J, Lee SK, et al. An interpretable radiomics model for the diagnosis of panic disorder with or without agoraphobia using magnetic resonance imaging. J Affect Disord 2022;305:47-54.


28. Sakai Y, Kumano H, Nishikawa M, Sakano Y, Kaiya H, Imabayashi E, et al. Cerebral glucose metabolism associated with a fear network in panic disorder. Neuroreport 2005;16:927-931.


30. Grillon C. Associative learning deficits increase symptoms of anxiety in humans. Biol Psychiatry 2002;51:851-858.


33. Carleton RN, Norton MA, Asmundson GJ. Fearing the unknown: a short version of the Intolerance of Uncertainty Scale. J Anxiety Disord 2007;21:105-117.


34. Kim SH. The relationship of fear of negative and positive evaluation, intolerance of uncertainty, and social anxiety [dissertation]. Seoul, Ewha Womans University. 2010;p.26.
35. Shear MK, Brown TA, Barlow DH, Money R, Sholomskas DE, Woods SW, et al. Multicenter collaborative panic disorder severity scale. Am J Psychiatry 1997;154:1571-1575.


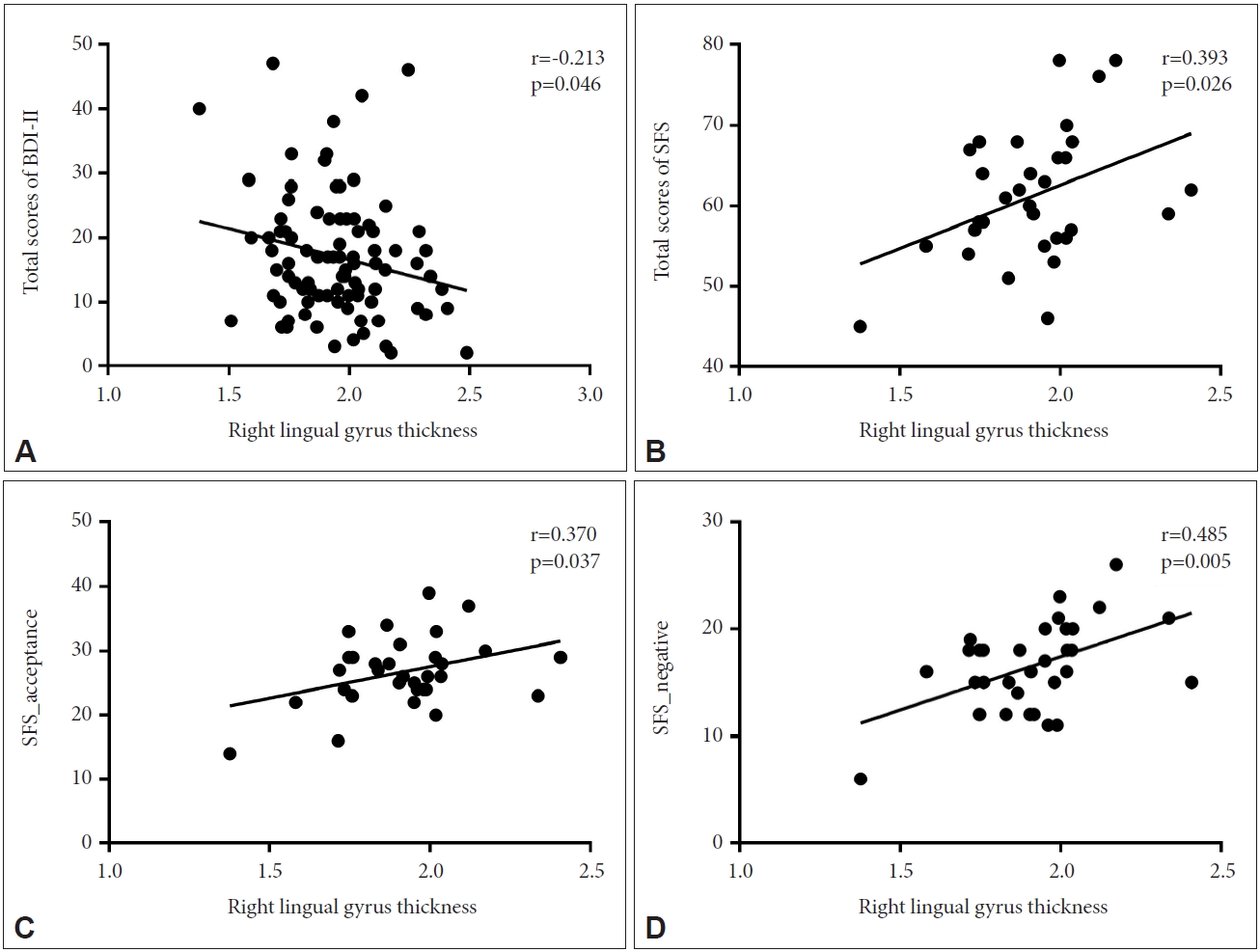
36. Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996.
37. Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 1988;56:893-897.


38. Brown TA, Antony MM, Barlow DH. Psychometric properties of the Penn State Worry Questionnaire in a clinical anxiety disorders sample. Behav Res Ther 1992;30:33-37.


39. Kim JB. Development of the Korean version of the panic disorder severity scale. Korean J Psychopathol 2001;10:140-151.
40. Jeon JW, Kim D, Kim E, Roh S. Exploratory and confirmatory factor analysis of the Korean version of the Penn State Worry Questionnaire. Anxiety Mood 2017;13:86-92.
41. Lim SY, Lee EJ, Jeong SW, Kim HC, Jeong CH, Jeon TY, et al. The validation study of Beck Depression Scale 2 in Korean version. Anxiety Mood 2011;7:48-53.
42. Lee HK, Lee EH, Hwang ST, Hong SH, Kim JH. Psychometric properties of the Beck Anxiety Inventory in the community-dwelling sample of Korean adults. Kor J Clin Psychol 2016;35:822-830.

43. Kim BJ, Lee D, Kim JG, Kim YS, Hwang JE. Development and validation of the self-forgiveness scale. Korean J Couns 2013;14:973-993.

44. Nam BH, Lee SU. Testing the validity of the Korean SF-36 health survey. J Korean Info Stat 2003;28:3-25.
45. Dale AM, Fischl B, Sereno MI. Cortical surface-based analysis. I. Segmentation and surface reconstruction. Neuroimage 1999;9:179-194.


47. Fischl B, Sereno MI, Dale AM. Cortical surface-based analysis. II: inflation, flattening, and a surface-based coordinate system. Neuroimage 1999;9:195-207.


48. Hagler DJ Jr, Saygin AP, Sereno MI. Smoothing and cluster thresholding for cortical surface-based group analysis of fMRI data. Neuroimage 2006;33:1093-1103.


49. Desikan RS, Ségonne F, Fischl B, Quinn BT, Dickerson BC, Blacker D, et al. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. Neuroimage 2006;31:968-980.


50. Fischl B, van der Kouwe A, Destrieux C, Halgren E, Ségonne F, Salat DH, et al. Automatically parcellating the human cerebral cortex. Cereb Cortex 2004;14:11-22.


52. Morriss J, Zuj DV, Mertens G. The role of intolerance of uncertainty in classical threat conditioning: recent developments and directions for future research. Int J Psychophysiol 2021;166:116-126.


53. McEvoy PM, Mahoney AE. To be sure, to be sure: intolerance of uncertainty mediates symptoms of various anxiety disorders and depression. Behav Ther 2012;43:533-545.


54. Wever M, Smeets P, Sternheim L. Neural correlates of intolerance of uncertainty in clinical disorders. J Neuropsychiatry Clin Neurosci 2015;27:345-353.


56. Lieberman L, Gorka SM, Sarapas C, Shankman SA. Cognitive flexibility mediates the relation between intolerance of uncertainty and safety signal responding in those with panic disorder. Cogn Emot 2016;30:1495-1503.


57. Craske MG, Rauch SL, Ursano R, Prenoveau J, Pine DS, Zinbarg RE. What is an anxiety disorder? Depress Anxiety 2009;26:1066-1085.


58. Carlson JM, Reinke KS, Habib R. A left amygdala mediated network for rapid orienting to masked fearful faces. Neuropsychologia 2009;47:1386-1389.


60. Kircher T, Arolt V, Jansen A, Pyka M, Reinhardt I, Kellermann T, et al. Effect of cognitive-behavioral therapy on neural correlates of fear conditioning in panic disorder. Biol Psychiatry 2013;73:93-101.


63. Weilnhammer V, Fritsch M, Chikermane M, Eckert AL, Kanthak K, Stuke H, et al. An active role of inferior frontal cortex in conscious experience. Current Biology 2021;31:2868-2880.


64. Sterzer P, Kleinschmidt A, Rees G. The neural bases of multistable perception. Trends Cogn Sci 2009;13:310-318.


68. Couvy-Duchesne B, Strike LT, de Zubicaray GI, McMahon KL, Thompson PM, Hickie IB, et al. Lingual gyrus surface area is associated with anxiety-depression severity in young adults: a genetic clustering approach. eNeuro 2018;5:ENEURO.0153-17.2017.

70. GEÇGİN FM, SAHRANÇ Ü. [The relationships between intolerance of uncertainty and psychological well-being]. Sakarya Univ J Educ 2017;7:739-756. Turkish.
72. Akgün Şahin Z, Deniz M, Akça D, Uymaz Aras G, Doğan S. The relationship between intolerance of uncertainty and spiritual well-being levels of COVID-19 among elderly: a cross sectional and correlational study. OMEGA (Westport) 2023;Mar 9 [Epub].
https://doi.org/10.1177/00302228231163208.

73. Koç M, Iskender M, Çolak TS, Düşünceli B. [Investigation of the effect of intolerance of uncertainty and the effect of anger control on the relationship between forgiveness and psychological well-being through structural equation modelling]. Sakarya Univ J Educ 2016;6:201-209. Turkish.