1. Ladame F, Jeanneret O. Suicide in adolescence: some comments on epidemiology and prevention. J Adolesc 1982;5:355-366.


2. O’Carroll PW, Berman AL, Maris RW, Moscicki EK, Tanney BL, Silverman MM. Beyond the Tower of Babel: a nomenclature for suicidology. Suicide Life Threat Behav 1996;26:237-252.


5. Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry 2013;70:300-310.


6. Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol 1979;47:343-352.


7. Kumar G, Steer RA. Psychosocial correlates of suicidal ideation in adolescent psychiatric inpatients. Suicide Life Threat Behav 1995;25:339-346.


9. Horowitz LM, Bridge JA, Pao M, Boudreaux ED. Screening youth for suicide risk in medical settings: time to ask questions. Am J Prev Med 2014;47:S170-S175.


11. Brezo J, Paris J, Turecki G. Personality traits as correlates of suicidal ideation, suicide attempts, and suicide completions: a systematic review. Acta Psychiatr Scand 2006;113:180-206.


12. Sinclair SJ, Roche MJ, Temes C, Massey C, Chung WJ, Stein M, et al. Evaluating chronic suicide risk with the Personality Assessment Inventory: Development and initial validation of the Chronic Suicide Risk Index (S_Chron). Psychiatry Res 2016;245:443-450.


13. Patry MW, Magaletta PR. Measuring suicidality using the Personality Assessment Inventory: a convergent validity study with federal inmates. Assessment 2015;22:36-45.


14. Nam JS, Kim DH, Kim EK. Psychological characteristics of psychiatric outpatients with high suicide risk: using MMPI-2-RF. Korean J Psychosom Med 2020;28:8-19.
15. Burke TA, Ammerman BA, Jacobucci R. The use of machine learning in the study of suicidal and non-suicidal self-injurious thoughts and behaviors: A systematic review. J Affect Disord 2019;245:869-884.


19. Walsh CG, Ribeiro JD, Franklin JC. Predicting risk of suicide attempts over time through machine learning. Clin Psychol Sci 2017;5:457-469.

20. Morey LC. The Personality Asssessment Inventory Manaual. Odessa, FL: Psychological Assessent Resources; 1991.
21. Kim YH, Kim JH, Oh SW, Lim YR, Hong SH. Standardization study of personality assessment inventory (PAI): reliability and validity. Kor J Clin Psychol 2001;20:311-329.
22. Lim SH, Hwang ST, Kweon HS, Kim JH, Park EY, Park JK, et al. Restandardization Study of the Korean Personality Assessment Inventory for Adolescent (PAI-A): Reliability and validity. Clin Psychol Kor Res Pract 2018;4:435-454.
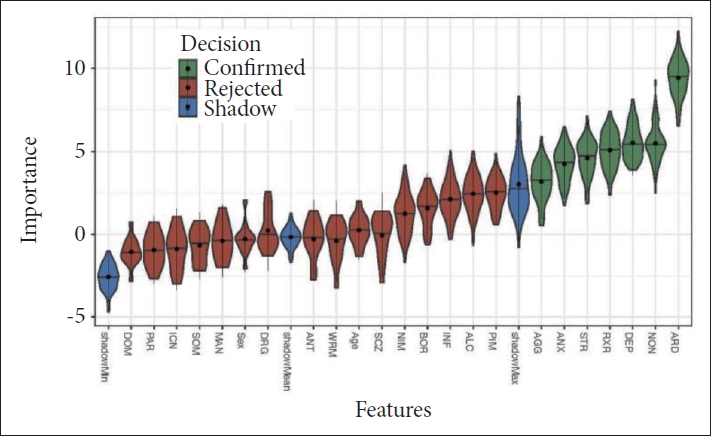
23. Kursa MB, Rudnicki WR. Feature selection with the Boruta package. J Stat Softw 2010;36:1-13.
24. Jeon HJ, Bae JM, Woo JM. Recent statistics and risk factors of suicide in children and adolescents. J Korean Med Assoc 2013;56:93-99.

25. Heo EH, Jeong SH, Kang HY. Comparative study on Personality Assessment Inventory and MMPI-2 profiles of groups with high and low depression and suicide ideation in psychiatry patients and discriminant variables of depression and suicide ideation. J Korean Neuropsychiatr Assoc 2018;57:86-95.

27. Charles NE, Bullerjahn MR, Barry CT. Understanding at-risk youths: average PAI-A scores and their associations with impulsivity-related constructs. J Pers Assess 2021;103:33-47.


29. Blakemore SJ, Choudhury S. Development of the adolescent brain: implications for executive function and social cognition. J Child Psychol Psychiatry 2006;47:296-312.


30. Wei HT, Lan WH, Hsu JW, Bai YM, Huang KL, Su TP, et al. Risk of suicide attempt among adolescents with conduct disorder: a longitudinal follow-up study. J Pediatr 2016;177:292-296.


31. Pompili M, Serafini G, Innamorati M, Biondi M, Siracusano A, Di Giannantonio M, et al. Substance abuse and suicide risk among adolescents. Eur Arch Psychiatry Clin Neurosci 2012;262:469-485.


33. Randell BP, Wang WL, Herting JR, Eggert LL. Family factors predicting categories of suicide risk. J Child Fam Stud 2006;15:247-262.

36. Angst F, Stassen H, Clayton PJ, Angst J. Mortality of patients with mood disorders: follow-up over 34-38 years. J Affect Disord 2002;68:167-181.


37. Henriksson MM, Aro HM, Marttunen MJ, Heikkinen ME, Isometsa ET, Kuoppasalmi KI, et al. Mental disorders and comorbidity in suicide. Am J Psychiatry 1993;150:935-940.


38. Melton TH, Croarkin PE, Strawn JR, McClintock SM. Comorbid anxiety and depressive symptoms in children and adolescent: a systematic review and analysis. J Psychiatr Pract 2016;22:84-98.


39. Yang CM, Lee SY. Effect of untreated depression in adolesence on the suicide risk and attempt in male young adults. Korean J Psychosom Med 2020;28:29-35.
40. Gunnell D, Harbord R, Singleton N, Jenkins R, Lewis G. Is low IQ associated with an increased risk of developing suicidal thoughts? Soc Psychiatry Psychiatr Epidemiol 2009;44:34-38.


42. Šimundić AM. Measures of diagnostic accuracy: basic definitions. EJIFCC 2009;19:203-211.