The Impact of Depressive Symptoms in Adults with ADHD Symptoms on Family Function and ADHD Symptoms of Their Children
Article information
Abstract
Objective
People with attention-deficit/hyperactivity disorder (ADHD) exhibit considerable impairment in social, academic, or occupational functioning. The present study aimed to examine the patterns of associations between ADHD symptoms, depression, and family functioning.
Methods
The sample consisted of 1,022 adults randomly selected from a district in Seoul, South Korea. Several self-assessment scales were utilized to rate ADHD symptoms (both past and current), current symptoms of depression, and level of family functioning. ADHD symptoms in the children of these participants were also assessed. Pearson's correlation and multiple linear regression analyses were performed; structural equation modeling (SEM) was conducted to determine the best fitting model.
Results
Adult ADHD symptoms were positively associated with depressive symptoms. Depressive symptoms, in turn, mediated the relationship between adult ADHD symptoms and cohesion among family members. In addition, depressive symptoms mediated the relationship between adult ADHD symptoms and their children's ADHD symptoms.
Conclusion
The relationship between adult ADHD symptoms and family dysfunction may be influenced by depressive symptoms. When treating ADHD in adults, clinicians should pay attention to the presence or absence of depression.
INTRODUCTION
Attention-deficit/hyperactivity disorder (ADHD) is a neurodevelopmental disorder with a symptom complex of inattention, hyperactivity, and impulsivity, affecting about 3-7% of school-aged children, according to the criteria of the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV).1 ADHD was once believed to be a childhood psychiatric disorder, but its persistence into adulthood has been recognized,2,3,4,5,6 and an approximately 1-4% prevalence of adult ADHD has been reported.
Childhood ADHD has been reported to show significant correlation with other psychiatric disorders later in adulthood, including mood and anxiety disorders, antisocial personality disorders, substance use disorders, eating disorders, and sleep disorders.7 By definition ADHD subjects endure significant impairment in social, academic, or occupational functioning regardless of their age, and more specifically, adults with ADHD tend to be at a higher risk of experiencing multiple marriages with repeated episodes of spousal separation and divorce, more frequent changes as well as poorer performance in employment, and increased driving risks including more speeding violations or automobile collisions.8,9 In terms of parenting, associations between adult ADHD and maladaptive parenting behaviors have been reported, with fathers using negative, critical, over-reactive, authoritarian, and therefore less effective disciplines when they had symptoms of ADHD, and mothers with ADHD being less consistent toward their children and less effective at solving childrearing problems.10,11,12 It is not difficult to assume that the impairments detailed above might compromise the parent-child and husband-wife cohesions, which is supported by the reportedly higher levels of conflict and lower levels of cohesion in families with an ADHD parent.13 These reports raise questions on the relationship among adults diagnosed with ADHD, other psychiatric disorders, and signs of functional maladaptation noted in various environmental settings.
We evaluated both the current and past severity of ADHD symptoms in a general population of adults. For a comorbid psychiatric disorder, we chose to evaluate the degree of depression, and as an indicator reflecting environmental consequences of the person's functional maladaptation, we chose to evaluate the level of family functioning. The objective of this study was to identify the patterns of interplay among ADHD symptoms, depression, and family functioning in adults. Possible hypothetical models would include, depressive symptoms mediating the relationship between ADHD symptoms and family functioning, or family functioning mediating the other two, or all three directly influencing one another. We also included in our survey the severity of ADHD symptoms found in children of our adult participants, considering the fact that biological offspring of ADHD parents are at higher risk of developing ADHD themselves,13,14 and ADHD symptoms of children in turn contribute to increased parental distress,15 which might be associated with more inappropriate and less compliant behaviors reported in those children.16
METHODS
Subjects
Participants were 1,022 adults living in the Jung-gu district, one of the 25 districts in Seoul, Korea, with a population of over 130,000. They were randomly selected from the general population of the district in collaboration with the Korea Data Network, a professional survey research company, under the administrative support of the local government office, which provided the addresses of its residents. The investigators visited their homes, provided a detailed explanation of the purpose of the study, obtained informed consent from eligible participants, distributed the questionnaires, and collected them on the same day. The questionnaire covered the following assessments, and those participants who had one or more children attending elementary school were also asked to complete an additional questionnaire inquiring about ADHD symptoms in their children. The institutional review board approval was obtained.
Assessments
The Wender Utah Rating Scale (WURS)17 is a 61-item self-reporting scale that retrospectively assesses childhood ADHD symptomatology of adult respondents, and the Brown Attention-Deficit Disorder Scale (BADDS) for Adolescents and Adults18 is a 40-item self-reporting scale that assesses impairments in 5 different clusters of daily executive functioning. Lee had extracted 34 from the 101 items which compose these 2 scales, and reorganized them into a new questionnaire, measuring the degree of ADHD symptoms experienced by the adult within the past month.19,20 This newly organized adult ADHD questionnaire rates each item on a 5-point Likert scale of 1 (never) to 5 (almost every day), thus the total score of all 34 items ranges from 34 to 170. Cronbach's alpha in the original study was 0.92. We used this questionnaire to evaluate the current severity of ADHD symptoms in our adult participants, and we have abbreviated this Korean questionnaire as K-ADHD-Current throughout this paper.
Lee had also introduced a new questionnaire assessing childhood symptoms of ADHD.19,20 By translating into Korean the list of 14 symptoms included in the DSM-III-R diagnostic criteria for ADHD, Lee had organized a 14-item self-reporting questionnaire asking the adult respondents to retrospectively rate their childhood ADHD symptoms on a 5-point Likert scale of 1 (never) to 5 (almost every day). The total score ranges from 14 to 70, and Cronbach's alpha for this questionnaire in the original study was 0.88. We used this questionnaire to evaluate the past severity of childhood ADHD symptoms in our adult participants, and we have abbreviated this Korean questionnaire throughout this paper as K-ADHD-Past.
The Center for Epidemiologic Studies Depression Scale (CES-D) is an adult self-reporting instrument containing 20 items designed to measure the degree of depressive symptoms experienced within the past week.21 A 4-point Likert scale is used, ranging from 0 (rarely or never) to 3 (most or all of the time), thus the total score ranges from 0 to 60. CES-D has been widely used as a screening tool for depression in epidemiologic surveys, and scores on the instrument have shown good correlation with clinical assessments of major depression.22 Reliability and validity of the Korean version of the CESD (CES-D-K) have been confirmed.23,24
The Family Adaptability and Cohesion Evaluation Scale (FACES III),25,26 a 20-item self-reporting questionnaire, measures the degree of family functioning in terms of two separate dimensions, which are cohesion and adaptability. Here cohesion reflects the emotional connectedness among members of the family, and adaptability reflects the flexibility to change the rules of the family, as well as the roles of its members. Ten items are allotted to each dimension, and the items are rated on a 5-point Likert scale of 1 (almost never) to 5 (almost always). Accordingly, the total score of the FACES III questionnaire ranges from 20 to 100, and the score of each dimension from 10 to 50.
The Korean ADHD Rating Scale (K-ARS) is a translated version of the ADHD Rating Scale (ARS),27,28 which consists of 18 items derived from the 18 symptoms list of the DSM-IV criteria for ADHD. Each item is rated on a 4-point Likert scale of 0 (never or rarely) to 3 (very often), thus the total score ranges from 0 to 54. Reliability and validity of the K-ARS among Korean children have been established.29
Statistical analysis
Pearson's correlation tests were performed between each pair of the above-mentioned scale scores using SPSS 19.0 software (SPSS Inc., Chicago, IL, USA). Structural equation modeling (SEM) was conducted with AMOS 5.0 (SmallWaters, Chicago, IL, USA) to determine the best fitting model. The model fit was based on generally accepted thresholds for the root mean square error of approximation (RMSEA), normed fit index (NFI), incremental fit index (IFI), comparative fit index (CFI), goodness of fit (GFI), and adjusted goodness of fit (AGFI). The RMSEA assesses closeness of fit, with values approximating 0.08, 0.05, and 0 indicating reasonable, close, and exact fits, respectively.30 The values of the NFI, IFI, CFI, GFI, and AGFI may range from 0 to 1, with values over 0.9 indicating an acceptable fit.31 In order to confirm the models obtained from the SEM, we performed multiple linear regression analyses using the scale scores included in the best fitting models as the independent and outcome variables. We additionally performed multiple linear regression analyses for all adult participants and for males and females separately. All analyses were tested with a significance level of p<0.05 (two-tailed).
RESULTS
Demographic characteristics
One thousand twenty-two adults, comprising 507 (49.6%) men and 515 (50.4%) women, participated in this study. Their age distribution was as follows: 24.9% in their 20s, 24.6% in their 30s, 21.4% in their 40s, 16.7% in their 50s, and 12.4% in their 60s. Among the total participants, 721 (70.5%) were married, and 506 (49.5%) had graduated from high school.
The ADHD, depression, and family functioning scores of adult participants, and the ADHD scores of their children
The mean scores of the K-ADHD-Current and -Past were 54.6±19.5 and 24.0±9.2, respectively. The mean CES-D-K score was 17.0±7.4, which is below the customary cutoff score of 23, a suggested threshold for indicating a major depressive disorder.32 The mean subscores of cohesion and adaptability derived from the FACES III were 34.3±6.9 and 29.3±5.5, respectively. The mean K-ARS score of the children was 11.5±9.3.
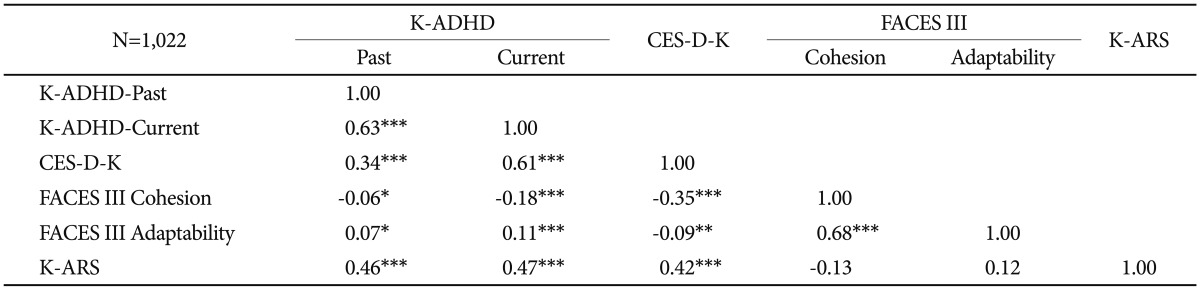
Correlations among the ADHD, depression, and family functioning scores of adult participants, and the ADHD scores of their children
The K-ADHD-Current score of the adult participants positively correlated with their scores on the K-ADHD-Past, the CES-D-K, the FACES III adaptability, and the K-ARS of their children (Table 1). The K-ADHD-Current score correlated negatively with the FACES III cohesion subscore. The K-ARS score of the children also positively correlated with the scores on the K-ADHD-Past and the CES-D-K of the adult participants. The cohesion subscore from the FACES III again negatively correlated with the scores on the K-ADHD-Past and the CES-D-K.
SEM among the ADHD, depression, and family functioning scores of adult participants, and the ADHD scores of their children
The final models of the SEM are shown in Figures 1 and 2. Adult ADHD (latent variable) was composed of the past childhood and current adulthood ADHD symptoms (i.e., the K-ADHD-Past and K-ADHD-Current scores, respectively). Adult ADHD was positively associated with the CES-D-K score, reflecting recent experience of depressive symptoms, which was in turn, negatively associated with the FACES III cohesion subscore, reflecting the emotional connectedness among members of the family (Figure 1, Table 2). These findings suggest that depressive symptoms mediate between symptoms of ADHD and family dysfunction. The proposed model showed an acceptable fit to the data (RMSEA=0.056, IFI=0.977, NFI=0.970, CFI=0.977, GFI=0.970, AGFI=0.952).
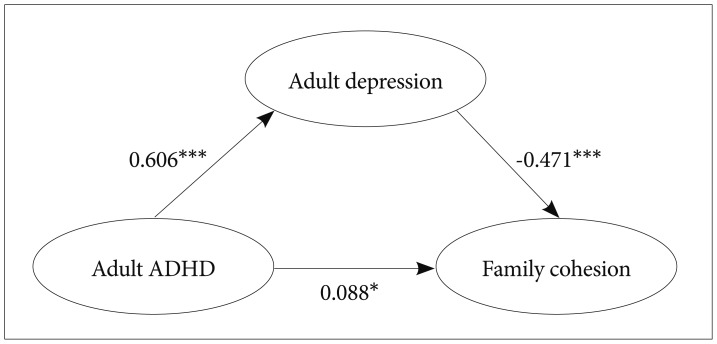
Structural equation modeling among the ADHD, depression, and family functioning scores of adult participants. All values are standardized regression weights. *p<0.05, ***p<0.001. The model showed an acceptable fit to the data (RMSEA=0.056, IFI=0.977, NFI=0.970, CFI=0.977, GFI=0.970, AGFI=0.952). ADHD: attention-deficit/hyperactivity disorder, RMSEA: root mean square error of approximation, IFI: incremental fit index, NFI: normed fit index, CFI: comparative fit index, GFI: goodness-of-fit index, AGFI: adjusted goodness-of-fit index.
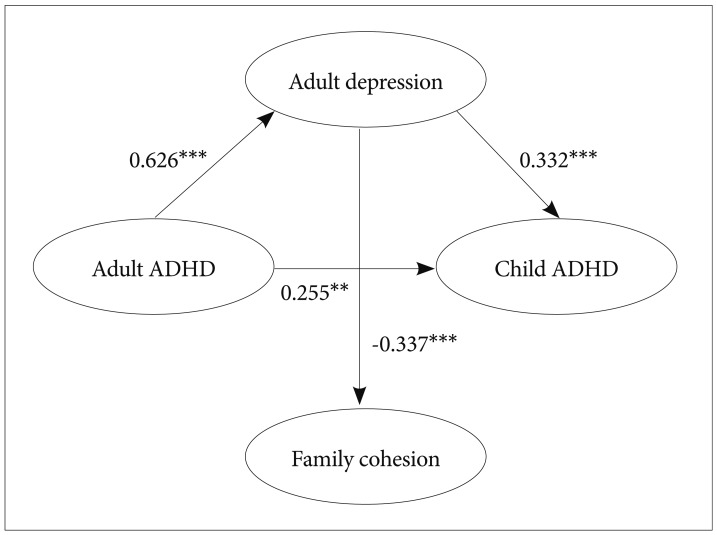
Structural equation modeling among the ADHD, depression, and family functioning scores of adult participants, and the ADHD symptom score of their children. All values are standardized regression weights. **p<0.01, ***p<0.001. The model showed an acceptable fit to the data (RMSEA=0.083, IFI=0.943, NFI=0.903, CFI=0.942, GFI=0.902, AGFI=0.855). ADHD: attention-deficit/hyperactivity disorder, RMSEA: root mean square error of approximation, IFI: incremental fit index, NFI: normed fit index, CFI: comparative fit index, GFI: goodness-of-fit index, AGFI: adjusted goodness-of-fit index.
Structural equation modeling among the ADHD, depression, and family functioning scores of adult participants, and the ADHD symptom score of their children
In the subsequent model including the offspring's ADHD symptoms, significant path from the adult ADHD to their children's ADHD symptoms was partially mediated by the CES-D-K scores of the parents (Figure 2, Table 2). This model demonstrated an acceptable fit to the data as well (RMSEA=0.083, IFI=0.943, NFI=0.903, CFI=0.942, GFI=0.902, AGFI=0.855).
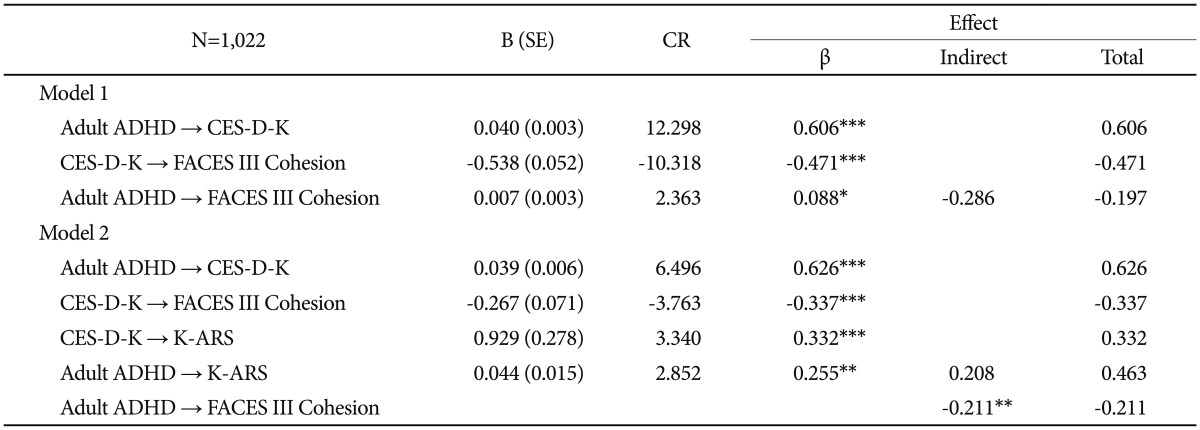
Multiple linear regression analyses among the ADHD, depression, and family functioning scores of adult participants, and the ADHD scores of their children
Using the CES-D-K score as the outcome variable, the K-ADHD-Past and -Current scores showed significant associations. Using the cohesion subscore from the FACES III as the outcome variable, the CES-D-K scores but not the K-ADHD-Past and -Current scores showed significant association. Using the K-ARS score of the children as the outcome variable, the K-ADHD-Past and the CES-D-K scores showed significant associations. These findings detailed in Table 3 are in accordance with the SEM results.
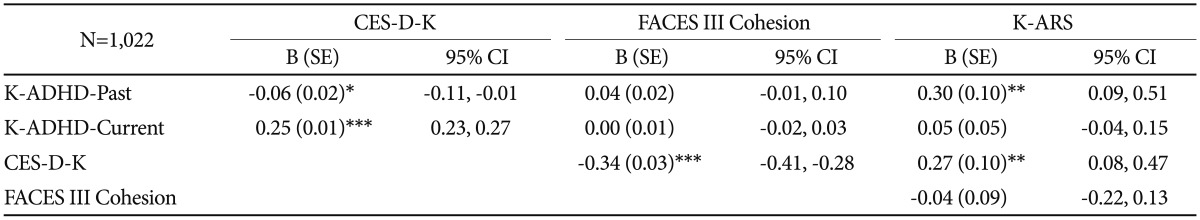
Multiple linear regressions among the ADHD, depression, and family functioning scores of adult participants, and the ADHD symptom score of their children
As supplemental tests, male and female adult participants were analyzed separately. Then, in males, only the K-ADHD-Past score (B=0.59, p=0.00, 95% CI=0.32, 0.85) remained significantly associated with the K-ARS score of their children. However, in females, the CES-D-K score (B=0.40, p=0.00, 95% CI=0.13, 0.66), and the cohesion (B=-0.38, p=0.03, 95% CI=-0.73, -0.03) and adaptability (B=0.50, p=0.01, 95% CI=0.11, 0.89) subscores from the FACES III were significantly associated with the K-ARS score of their children (Supplementary Table 1, online).
DISCUSSION
The present study aimed to examine the patterns of interplay among ADHD symptoms, depression, and family functioning in a general population of adults. We used both the past childhood and current adulthood ADHD symptoms to construct the latent variable of adult ADHD, given that the presence of childhood ADHD symptoms is required for the diagnosis of ADHD in adults. As a result, adult ADHD was associated with depressive symptoms. Symptoms of adult ADHD being directly related to concurrent depression is in accordance with the reports on high comorbidity rates of ADHD and depression.7,33 Depressive symptoms, in turn, mediated the relationship between ADHD symptoms in adults and cohesion among members of their family. In addition, depressive symptoms also mediated the relationship between adult ADHD symptoms and their children's ADHD symptoms.
Adult ADHD symptoms were both directly and indirectly related to ADHD symptoms found in their children. The direct relationship might reflect a genetic link, since the heritability of ADHD is among the highest compared to other psychiatric disorders.9 Meanwhile, the indirect relationship, which was mediated by adult depression, is more complex to interpret. In an adoption study, parental major depression increased the risk for ADHD in both their biological and adopted children, suggesting that depressed parents cannot be ruled out as an environmental liability for the development of ADHD in their offspring.34 Furthermore, studies have shown that severity of maternal depression positively correlates with, not only the mother's but also the father's, high ratings of their child's externalizing behaviors,35,36 and treatment of maternal depression improves the mother-reported behavioral problems of their children.37,38 Although the mechanisms underlying these results are not clearly explored, considering that ADHD ratings in children were also based on parental reports in our study, similar mechanisms might be involved in our results directly linking depression in adults and ADHD in their children.
It is also noteworthy that depression was inversely associated with family cohesion, but no significant path was observed between family cohesion and the offspring's ADHD symptoms. When interpreting this negative finding, however, caution may need to be taken. In families with higher FACES III cohesion or adaptability scores, parents tended to underestimate the severity of ADHD symptoms in their children.39 As the measures of the current study were based on self- or parent-reports, possible reporter bias may have affected the link between family cohesion and the children's ADHD symptoms.
The multiple regression analyses also replicated the results from our SEM. Interestingly, however, when regression analyses were performed separately in each sex, only the past ADHD symptoms remained significantly associated in males (Supplementary Table 1, online). On the other hand, in mothers, their depressive symptoms and level of family functioning were significantly associated with their children's ADHD symptoms: this finding is perhaps related to the fact that mothers rather than fathers are usually the ones who spend much more time with their children in Korean families. Thus, their mood symptoms and perceived family functioning might more closely interact with the behavioral problems of their children. Clinically, in treating children with ADHD, perhaps more attention should be paid to the depressive symptoms of their mothers.
The major limitations of this study include the followings. First, it was a cross-sectional study, which had a key shortcoming in assessing the causal relationships. Prospective studies are required to confirm our inferences discussed above. Second, all of the measures in this study were self- or parent-reported, which are prone to reporter bias, and no formal diagnosis was made of either ADHD or depressive disorder. And third, considering the remarkably higher rates of comorbid major depressive disorder in community samples of ADHD youth,40,41 ranging from 12% to 50%, it would have been more fruitful to evaluate symptoms of depression in the children as well.
Many have reported associations between ADHD, either in the parent or in the child, and disturbances in family functioning.9,10,11,12,13,15,42 Accordingly, we had expected that symptoms of ADHD in our parents would somehow compromise their family life. As a result, both the direct and indirect paths were found to be significant between adult ADHD symptoms and the scores of the FACES III or their children's scores of the K-ARS. The indirect path was mediated by adult depressive symptoms. Considering that the majority of former studies on the relationship between adult ADHD and family dysfunction did not assess the role of depression, further studies including adequate assessment of mood symptoms are needed. As for clinical implications, when treating ADHD in adults, clinicians should pay attention to the presence or absence of depression.
Acknowledgments
The research was performed with the annual budget of the Jung-gu Community Mental Health Center run by the Korean government.
References
Supplementary Material
Supplementary Table 1
Multiple linear regression of the ADHD, depression, and family functioning scores of adult participants on the ADHD symptom score of their children