1. Keller MB, Roland RJ. Implications of failing to achieve successful long-term maintenance treatment of recurrent unipolar major depression. Biol Psychiatry 1998;44:348-360. PMID:
9755357.


2. Goldberg D. The "NICE Guideline" on the treatment of depression. Epidemiol Psichiatr Soc 2006;15:11-15. PMID:
16584098.


3. Gaynes BN, Rush AJ, Trivedi MH, Wisniewski SR, Spencer D, Fava M. The STAR
*D study: treating depression in the real world. Cleve Clin J Med 2008;75:57-66. PMID:
18236731.


4. Mathys M, Mitchell BG. Targeting treatment-resistant depression. J Pharm Pract 2011;24:520-533. PMID:
22095575.


5. Fava M, Davidson KG. Definition and epidemiology of treatment-resistant depression. Psychiatr Clin North Am 1996;19:179-200. PMID:
8827185.


6. Viner MW, Chen Y, Bakshi I, Kamper P. Low-dose risperidone augmentation of antidepressants in nonpsychotic depressive disorders with suicidal ideation. J Clin Psychopharmacol 2003;23:104-106. PMID:
12544386.


7. Dunner DL, Amsterdam JD, Shelton RC, Loebel A, Romano SJ. Efficacy and tolerability of adjunctive ziprasidone in treatment-resistant depression: a randomized, open-label, pilot study. J Clin Psychiatry 2007;68:1071-1077. PMID:
17685744.


8. Papakostas GI, Petersen TJ, Kinrys G, Burns AM, Worthington JJ, Alpert JE, et al. Aripiprazole augmentation of selective serotonin reuptake inhibitors for treatment-resistant major depressive disorder. J Clin Psychiatry 2005;66:1326-1330. PMID:
16259548.


9. Adson DE, Kushner MG, Eiben KM, Schulz SC. Preliminary experience with adjunctive quetiapine in patients receiving selective serotonin reuptake inhibitors. Depress Anxiety 2004;19:121-126. PMID:
15022147.


10. Barbee JG, Conrad EJ, Jamhour NJ. The effectiveness of olanzapine, risperidone, quetiapine, and ziprasidone as augmentation agents in treatment-resistant major depressive disorder. J Clin Psychiatry 2004;65:975-981. PMID:
15291687.


11. Meltzer-Brody S. New insights into perinatal depression: pathogenesis and treatment during pregnancy and postpartum. Dialogues Clin Neurosci 2011;13:89-100. PMID:
21485749.



12. Yonkers KA, Vigod S, Ross LE. Diagnosis, pathophysiology, and management of mood disorders in pregnant and postpartum women. Obstet Gynecol 2011;117:961-977. PMID:
21422871.


13. Birmaher B, Brent D, Bernet W, Bukstein O, Walter H, et al. AACAP Work Group on Quality Issues. Practice parameter for the assessment and treatment of children and adolescents with depressive disorders. J Am Acad Child Adolesc Psychiatry 2007;46:1503-1526. PMID:
18049300.


14. Hughes CW, Emslie GJ, Crismon ML, Posner K, Birmaher B, Ryan N, et al. Texas Children's Medication Algorithm Project: update from Texas Consensus Conference Panel on Medication Treatment of Childhood Major Depressive Disorder. J Am Acad Child Adolesc Psychiatry 2007;46:667-686. PMID:
17513980.


15. Taylor WD, Doraiswamy PM. A systematic review of antidepressant placebo-controlled trials for geriatric depression: limitations of current data and directions for the future. Neuropsychopharmacology 2004;29:2285-2299. PMID:
15340391.


16. Dunner DL. Treatment considerations for depression in the elderly. CNS Spectr 2003;8(12 Suppl 3):14-19. PMID:
14978459.


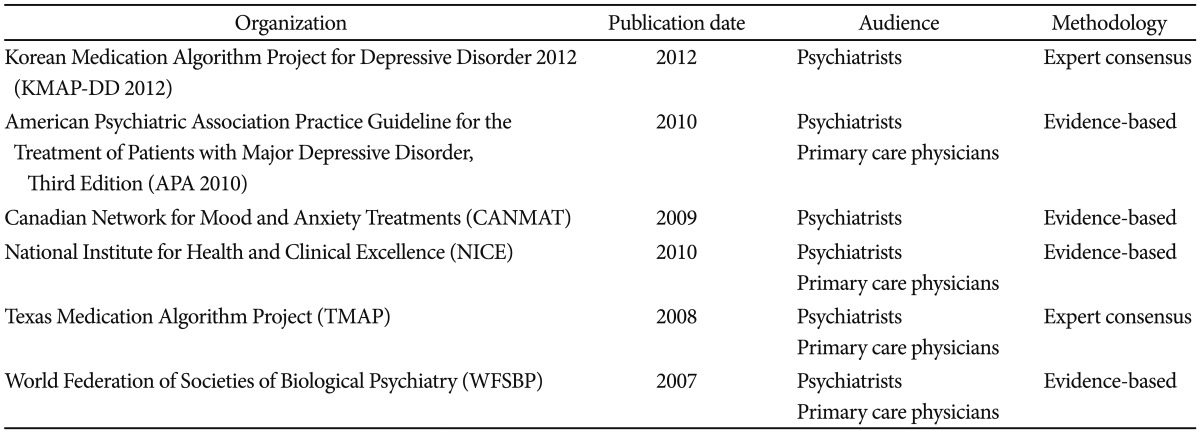
17. Kennedy SH, Lam RW, Parikh SV, Patten SB, Ravindran AV. Canadian Network for Mood and Anxiety Treatments (CANMAT) clinical guidelines for the management of major depressive disorder in adults. Introduction. J Affect Disord 2009;117(Suppl 1):S1-S2. PMID:
19682750.


18. Bauer M, Bschor T, Pfennig A, Whybrow PC, Angst J, Versiani M, et al. World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for Biological Treatment of Unipolar Depressive Disorders in Primary Care. World J Biol Psychiatry 2007;8:67-104. PMID:
17455102.


19. American Psychiatric Association. Treatment of Patients with Major Depression and Practical Guideline. 3rd Edition. Washington DC: American Psychiatric Association; 2010.
20. National Collaborating Centre for Mental Health (commissioned by the National Institute for Health & Clinical Excellence). Depression: the treatment and management of depression in adults. (updated edition). London: The British Psychological Society and The Royal College of Psychiatrists; 2010.
21. Suehs B, Argo TR, Bendele SD, Crimson ML, Trivedi MH, Kurian B. Texas Medication Algorithm Project Procedural Manual Major depressive disorder algorithms. Texas: Texas Department of State health Services; 2008.
22. Ahn YM, Kim DJ, Kwon JS, Bahk WM, Lee HS, Kim YS. Korean Medication Algorithm Projects for Major Psychiatric Disorders(I) : The Genefit and Risk of Algorithm and the General Considerations of Developing Medication Algorithm. Korean J Psychopharmacol 2002;13:18-29.
23. Seo JS, Min KJ, Kim W, Seok JH, Bahk WM, Song HC, et al. Korean Medication Algorithm for Depressive Disorder 2006 (I). J Korean Neuropsychiatr Assoc 2007;46:453-460.

24. Nemeroff CB. Use of atypical antipsychotics in refractory depression and anxiety. J Clin Psychiatry 2005;66(Suppl 8):13-21. PMID:
16336032.
25. Papakostas GI, Shelton RC, Smith J, Fava M. Augmentation of antidepressants with atypical antipsychotic medications for treatment-resistant major dperessive disorder: a meta-analysis. J Clin Psychiatry 2007;68:826-831. PMID:
17592905.


26. Papakostas GI, Petersen TJ, Kinrys G, Burns AM, Worthington JJ, Alpet JE, et al. Aripiprazole augmentation of selective serotonin reuptake inhibitors for treamtent-resistant major depressive disorder. J Clin Psychiatry 2005;66:1326-1330. PMID:
16259548.


27. Executive Committee of Korean Medication Algorithm Project for Depressive Disorder 2012. Korean Medication Guideline for Depressive Disorder 2012. Seoul: ML communication; 2012.
28. Canadian Psychiatric Association. Canadian Network for Mood and Anxiety Treatments (CANMAT). Clinical guidelines for the treatment of depressive disorders. Can J Psychiatry 2001;46(Suppl 1):5S-90S. PMID:
12371438.

29. Sachs GS, PRintz DJ, Kahn DA, Carpenter D, Docherty JP. The Expert Consensus Guideline Series: Medication Treatment of Bipolar Disorder 2000. Postgrad Med 2000;Spec No:1-104. PMID:
10895797.

30. Lam RW, Kenney SH, Grigoriadis S, McIntyre RS, Milev R, Ramasubbu R, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) clinical guidelines for the management of major depressive disorder in adults. III. Pharmacotherapy. J Affect Disord 2009;117(Suppl 1):S26-S43. PMID:
19674794.


31. Lee KU, Kim W, Min KJ, Shin YC, Chung SK, Bahk WM. The Rate and Risk Factors of Early Discontinuation of Antidepressant Treatment in Patients with Major Depressive Disorder. Korean J Psychopharmacol 2006;17:550-556.
32. Kim NS, Kim KH, Lee SM, Paik JW, Lee BR, Hwang JH. Health Services Utilization and Depression Care Quality among Depressed Patients. Seoul: Health Insurance Review and Assessment Service; 2008.
33. Joe SH, Lee HJ. A case of morning light treatment for a depressive episode with seasonal pattern. J Korean Neuropsychiatr Assoc 1998;37:585-592.