1. Simonsen E. The integration of categorical and dimensional approaches to psychopathology. In: Millon T, Krueger RF, Simonsen E, editor. Contemporary directions in psychopathology: scientific foundations of the DSM-V and ICD-11. New York: Guilford Press, 2010, p. 350-361.
2. Kraemer HC, Noda A, OŌĆÖHara R. Categorical versus dimensional approaches to diagnosis: methodological challenges. J Psychiatr Res 2004;38:17-25.


3. LeBeau R, B├Čgels S, M├Čller E, Craske M. Integrating dimensional assessment and categorical diagnosis in DSM-5: the benefits and challenges of the paradigm shift for the anxiety disorders. Psychopathol Rev 2015;2:83-99.


4. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-IV). Washington: American Psychiatric Association; 2000,4th ed.
6. Boyle LH, Smith GT. Spectrum model. In: Cautin RL, Lilienfeld SO, editor. The encyclopedia of clinical psychology. Hoboken: Wiley-Blackwell, 2015, p. 1-5.
7. Zaworka W, Hand I. [Phenomenology of obsessions and compulsions. Experimental diagnosis of obsessive compulsive neurosis. I (authorŌĆÖs transl)]. Arch Psychiatr Nervenkr (1970) 1980;228:257-273. German.

8. Bienvenu OJ, Samuels JF, Wuyek LA, Liang KY, Wang Y, Grados MA, et al. Is obsessive-compulsive disorder an anxiety disorder, and what, if any, are spectrum conditions? A family study perspective. Psychol Med 2012;42:1-13.


9. Fineberg NA, Saxena S, Zohar J, Craig KJ. Obsessive-compulsive disorder: boundary issues. CNS Spectr 2007;12:359-364. 367-375.


10. De Caluwe E, Vergauwe J, Decuyper M, Bogaerts S, Rettew DC, De Clercq B. The relation between normative rituals/routines and obsessive-compulsive symptoms at a young age: a systematic review. Dev Rev 2020;56:100913

11. Stein DJ, Ono Y, Tajima O, Muller JE. The social anxiety disorder spectrum. J Clin Psychiatry 2004;65(Suppl 14):27-33. quiz 34-36.
12. Crome E, Baillie A, Slade T, Ruscio AM. Social phobia: further evidence of dimensional structure. Aust N Z J Psychiatry 2010;44:1012-1020.


13. Schneier FR, Blanco C, Antia SX, Liebowitz MR. The social anxiety spectrum. Psychiatr Clin North Am 2002;25:757-774.


14. Hyett MP, McEvoy PM. Social anxiety disorder: looking back and moving forward. Psychol Med 2018;48:1937-1944.


15. DellŌĆÖOsso L, Rucci P, Cassano GB, Maser JD, Endicott J, Shear MK, et al. Measuring social anxiety and obsessive-compulsive spectra: comparison of interviews and self-report instruments. Compr Psychiatry 2002;43:81-87.


16. DellŌĆÖOsso L, Cassano GB, Sarno N, Millanfranchi A, Pfanner C, Gemignani A, et al. Validity and reliability of the structured clinical interview for obsessiveŌĆÉcompulsive spectrum (SCIŌĆÉOBS) and of the structured clinical interview for social phobia spectrum (SCIŌĆÉSHY). Int J Methods Psychiatr Res 2000;9:11-24.

17. Hahn OS, Ahn JH, Song SH, Cho MJ, Kim JK, Bae JN, et al. Development of Korean version of structured clinical interview schedule for DSM-IV axis I disorder: interrater reliability. J Korean Neuropsychiatr Assoc 2000;39:362-372.
18. Hodgson RJ, Rachman S. Obsessional-compulsive complaints. Behav Res Ther 1977;15:389-395.


20. Min BB, Won HT. Reliability and validity of the Korean translations of Maudsley obsessional-compulsive inventory and Padua inventory. Korean J Clin Psychol 1999;18:163-182.
21. Liebowitz MR. Social phobia. Mod Probl Pharmacopsychiatry 1987;22:141-173.


22. Baker SL, Heinrichs N, Kim HJ, Hofmann SG. The Liebowitz social anxiety scale as a self-report instrument: a preliminary psychometric analysis. Behav Res Ther 2002;40:701-715.


23. Yu ES, Ahn CI, Park KH. Factor structure and diagnostic efficiency of a Korean version of the Liebowitz social anxiety scale. Korean J Clin Psychol 2007;26:251-270.

24. Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika 1951;16:297-334.


25. Taber KS. The use of CronbachŌĆÖs alpha when developing and reporting research instruments in science education. Research in Science Education 2018;48:1273-1296.


26. Ware JE Jr, Gandek B. Methods for testing data quality, scaling assumptions, and reliability: the IQOLA project approach. J Clin Epidemiol 1998;51:945-952.

27. Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 2007;60:34-42.


28. Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale: Lawrence Erlbaum Associates; 1988.
29. Hughes G. YoudenŌĆÖs index and the weight of evidence revisited. Methods Inf Med 2015;54:576-577.


30. Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 1982;143:29-36.


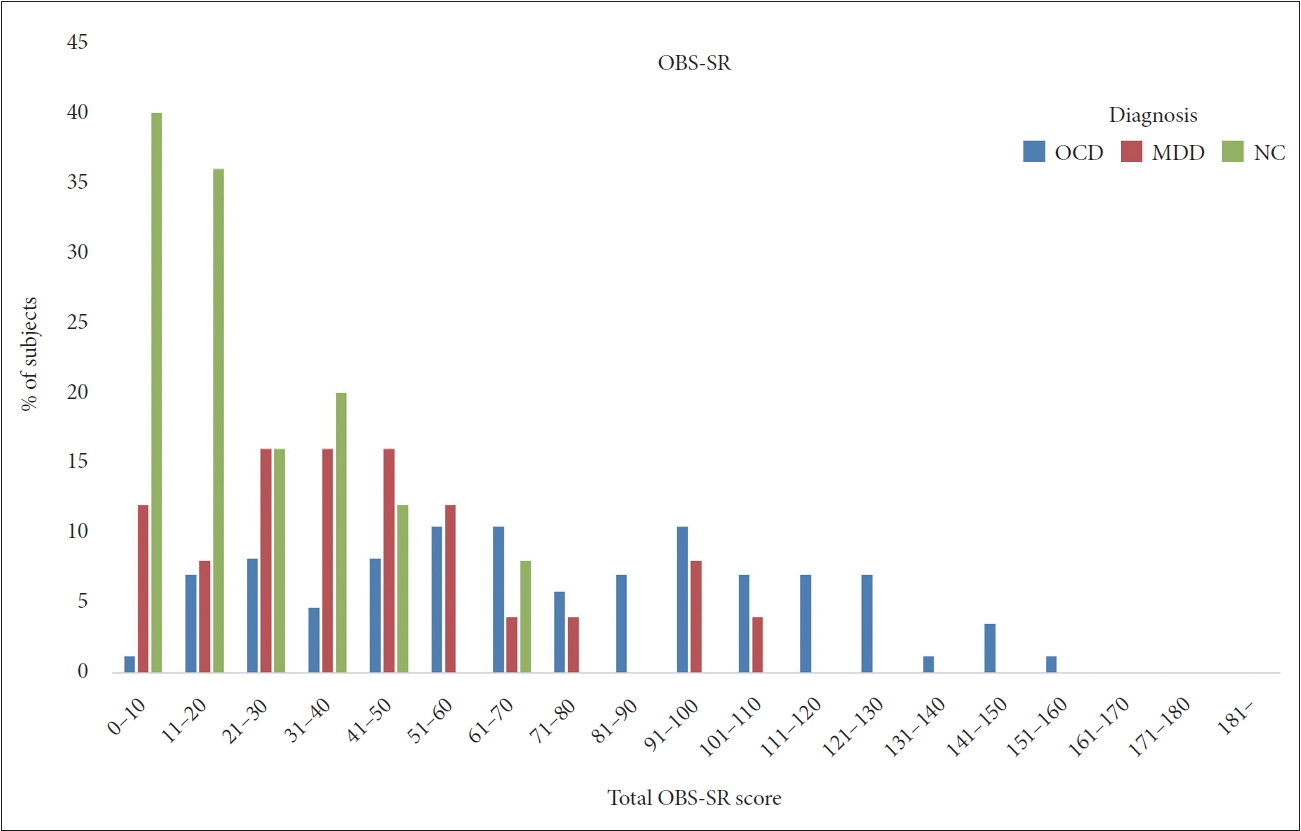
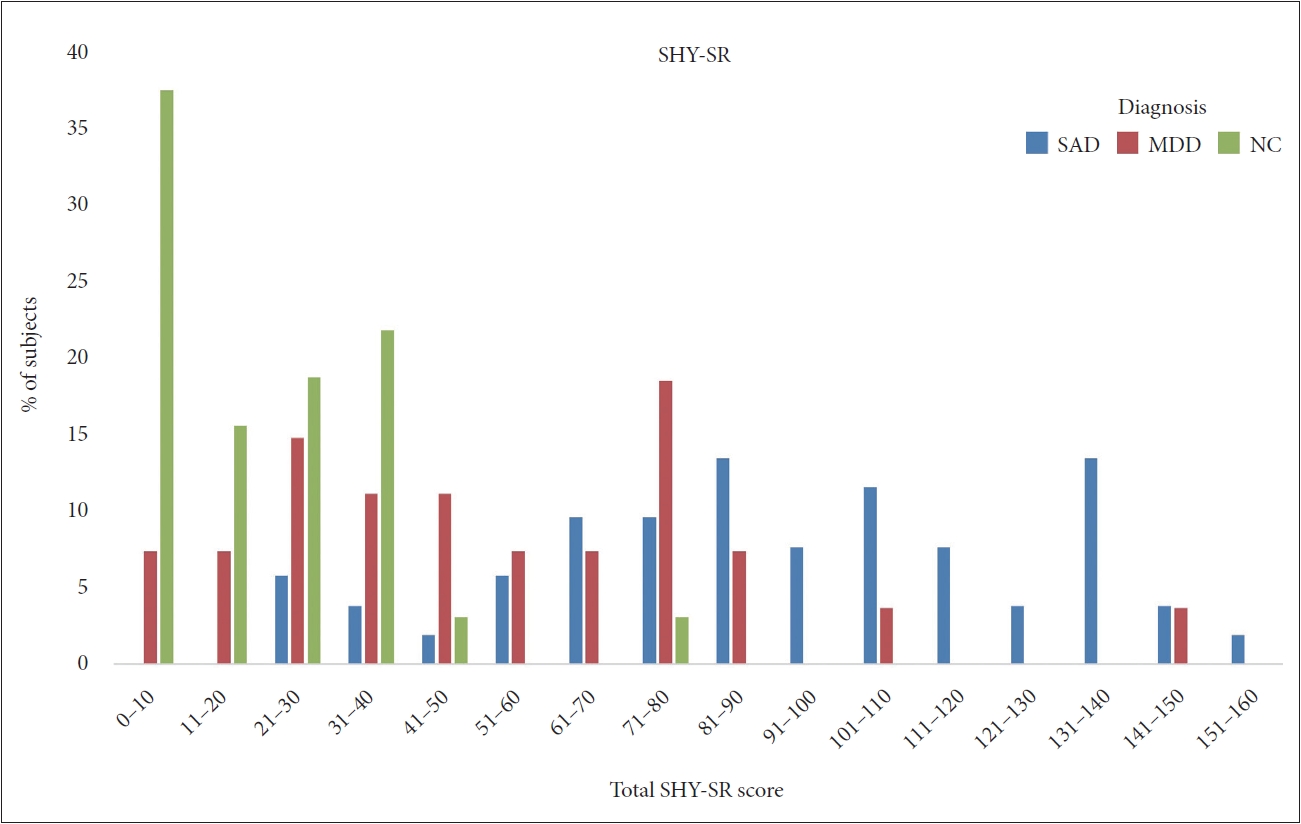
32. DellŌĆÖOsso L, Nardi B, Bonelli C, Gravina D, Benedetti F, Del Prete L, et al. Validation of the short version of the obsessive compulsive spectrum questionnaire. Front Psychol 2023;14:1157636


33. Berrocal C, Ruiz Moreno MA, Montero M, Rando MA, Rucci P, Cassano GB. Social anxiety and obsessive-compulsive spectra: validation of the SHY-SR and the OBS-SR among the Spanish population. Psychiatry Res 2006;142:241-251.