Validation of the Chinese Version of Penn Alcohol Craving Scale for Patients With Alcohol Use Disorder
Article information
Abstract
Objective
The Penn Alcohol Craving Scale (PACS) is a five-item, single-dimension questionnaire that is used to measure a patient’s alcohol craving. We sought to develop the Chinese version of the PACS (PACS-C) and assess its reliability and validity.
Methods
A total of 160 Taiwanese patients with alcohol use disorder were enrolled in this study. The internal consistency and concurrent validity of the PASC-C with the visual analogue scale (VAS) for craving, the Yale–Brown Obsessive Compulsive Scale for heavy drinking (YBOCS-hd), and the Severity of Alcohol Dependence Questionnaire (SADQ) were assessed. The test–retest reliability of the PASC-C was evaluated 1 day after the baseline measurements. Confirmatory factor analysis (CFA) was performed to examine the psychometric properties of the PACS-C.
Results
The PACS-C exhibited good internal consistency (Cronbach’s α=0.95) and test–retest reliability (r=0.97). This scale showed high correlations with the VAS (r=0.81) and YBOCS-hd (r=0.81 and 0.79 for the obsession and compulsion subscales, respectively), and moderate correlation with the SADQ-C (r=0.47). Furthermore, CFA results revealed that the PACS-C had good fit indices under various models.
Conclusion
The PACS-C appears to be a reliable and valid tool for assessing alcohol craving in patients with alcohol use disorder in Taiwan.
INTRODUCTION
The phenomenon of cravings has garnered considerable attention as a key feature associated with substance use disorders, including alcohol use disorder. The International Statistical Classification of Diseases and Related Health Problems, Tenth Revision includes craving as a feature of alcohol dependence, which is defined as a strong desire or sense of compulsion [1]. Furthermore, in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), craving is defined as an intense desire or urge for a substance and is recognized as a diagnostic criterion for alcohol use disorder [2]. Craving (i.e., preoccupation and anticipation) is considered the paramount predictor of relapse in addictive disorders [3]. Brain imaging studies have demonstrated that craving is associated with functional changes in specific brain circuits [4,5], and pharmacotherapies against craving have been in development [6]. The level of craving may help predict the risk of subsequent relapse in both inpatients and outpatients [7,8]. Therefore, measuring the level of alcohol craving is crucial for understanding how to treat alcohol use disorder.
Various definitions of craving had been proposed previously. The concept of craving was first introduced by the members of the World Health Organization Expert Committees on Mental Health and on Alcohol in 1954 as a characteristic of psychological dependence [9]. Later, operant conditioning [10] and the cognitive model [11] were introduced to explain the association between cues and craving. Recent neuroimaging studies have revealed that craving is associated with certain brain regions, including the ventral tegmental area, nucleus accumbens, and prefrontal cortex, and the symptomology of craving is also related to the neuropathology of these brain circuits [12].
The current scales used to measure alcohol craving can be of two types: single- and multi-item scales. Single-item scales, such as the visual analogue scale (VAS), Likert scale, and Penn Alcohol Craving Scale (PACS), are used to measure the intensity or frequency of craving and have the advantages of easy administration and reduced respondent burden and refusal risk [13]. However, information on obsessive thoughts and compulsive behaviors regarding drinking and the anticipation of a positive outcome or relief from negative affect, need to be obtained through multi-item scales, such as the Obsessive Compulsive Drinking Scale and the Yale–Brown Obsessive Compulsive Scale for heavy drinking (YBOCS-hd). The YBOCS-hd was translated into Chinese and validated in 2005; however, the requirement of trained raters limits its clinical application [14].
The PACS is a five-item, single-dimension, self-reported questionnaire. Its first three questions help assess the frequency, intensity, and duration of alcohol cravings. The last two questions help assess the ability to resist temptation and the patient’s craving level in the past week [15]. Users can rate each item on a scale of 0–6; the total score is 30 points. A PACS score of ≥15 indicates clinically significant alcohol craving [16].
The PACS is a reliable and validated scale [15] that can be used to predict the risk of relapse into alcohol dependence [17]. This tool can be used for both inpatients and outpatients with alcohol dependence. The scores are positively correlated with the severity of alcohol dependence and nonresponsiveness to treatment [18,19]. This scale has been translated into Korean [20], Portuguese [21], and Polish [22], with each version showing good reliability and validity. Moreover, it has been modified in different languages to measure drug craving [23,24].
In this study, we aimed to develop the Chinese version of the PACS (PACS-C) as a tool for measuring alcohol craving in patients with alcohol dependence who seek treatment. In addition, we assessed the reliability and validity of the PACS-C.
METHODS
Study participants and procedures
We consecutively recruited a total of 160 Taiwanese participants from the inpatient and outpatient departments of the Taipei City Psychiatric Center, Taipei City Hospital between 2020 and 2021. The inclusion criteria were as follows: 1) an age of 20–65 years, 2) a diagnosis of alcohol use disorder based on the DSM-5, as ascertained by two board-certified psychiatrists, and 3) the ability to understand the study and provide informed consent for participation. Patients with severe mental illnesses, such as schizophrenia, bipolar disorder, or major depressive disorder with psychotic features; neurocognitive disorders; or difficulty in understanding the study were excluded.
After providing informed consent, the participants completed the study questionnaire with the help of an assistant. The questionnaire included the PACS-C, YBOCS-hd, VAS for craving, Severity of Alcohol Dependence Questionnaire (SADQ), and questions on the sociodemographic and clinical characteristics of the participants. Clinical characteristics of alcohol use includes the age at which alcohol is first consumed, the age at which alcohol tolerance develops, and the amounts of drinks (equivalent to 10 gram of ethanol) consumed per drinking day. Tolerance is defined as requiring more alcohol to achieve the desired effect. The approximate time needed to complete the questionnaire was 15 min. Furthermore, a total of 40 inpatients completed the PACS-C again 1 day after their first assessment; this was necessary for us to assess the test–retest reliability. The study protocol was approved by the Research Ethics Committee of Taipei City Hospital (IRB protocol number=TCHIRB-10902006, and date of approval=May 15, 2020).
PACS-C
Approval to develop PACS-C was obtained from Mapi Research Trust, which officially distributes the PACS. Two board-certified psychiatrists (HMC and MCH) with expertise in treating alcohol dependence translated the PACS into Chinese. Back translation was then performed by a bilingual mental health professional. The board-certified psychiatrists, psychiatric residents, and a psychologist then reviewed the translated version to validate its meaning remained faithful to the original version. The final version of the PACS-C has five items; each item can be scored from 0 to 6. The items help measure the frequency, intensity, and duration of alcohol cravings; the ability to resist temptation; and the patient’s craving level in the past week.
The Chinese version of YBOCS-hd
The YBOCS-hd is a tool used to assess heavy drinking. This is the modified version of the YBOCS, with five items for assessing obsessive thoughts and another five items for assessing compulsive behavior regarding alcohol drinking [25,26]. Each item is scored on a five-point scale (0–4), and the total score is 40 points. The Chinese version of the YBOCS-hd (YBOCS-hd-C) was developed in 2005 with acceptable interrater reliability (intraclass correlation=0.89–0.96), internal consistency (Cronbach’s α=0.99), construct validity, and concurrent validity [14].
The VAS of craving for alcohol
The VAS uses a 100 mm straight line with two axes of “do not want to drink at all” and “want to drink very much” to measure the extent of a patient’s current desire to drink. Participants were requested to mark their current level of craving for alcohol on the straight line. The total score on the VAS was calculated on a scale of 0–100 in this study.
The Chinese version of SADQ
The SADQ is a widely used 20-item questionnaire with good reliability for measuring alcohol dependence. The SADQ has five sections, which assess physical withdrawal symptoms, emotional withdrawal symptoms, withdrawal relief from drinking, recovery from drinking, and symptoms after withdrawal. The SADQ can be self-administered by the patient or assessed by a trained rater. Each item is scored on a four-point scale (i.e., 0–3; possible score range, 0–60). A total score of ≥30 indicates severe alcohol dependence [27]. The SADQ was translated into Chinese (SADQ-C) in 2009 with acceptable internal consistency (Cronbach’s α=0.92) [28].
Statistical analysis
All statistical analyses were performed using SPSS 12.0 (SPSS Inc., Chicago, IL, USA). The reliability of the PACS-C was validated on the basis of internal consistency, which was calculated by determining the Cronbach’s α coefficient and item–total correlations. Test–retest reliability was validated using the Pearson correlation coefficient. The concurrent validity of the PACS-C was studied through correlation analysis of it with two other scales that help measure craving: the YBOCS-hd-C and VAS, and the scale that measure the severity of alcohol dependence, the SADQ-C.
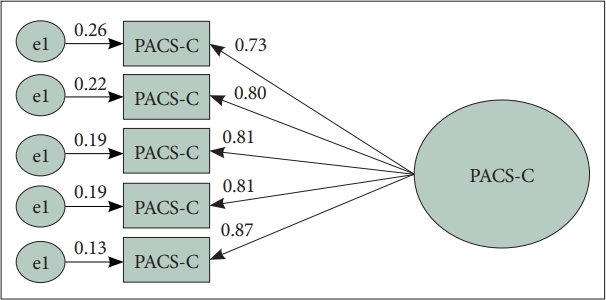
Confirmatory factor analysis (CFA) was performed to verify the construct validity of the original single-factor structure suggested by Flannery et al. [15] and to test the fit of individual items. We used a weighted least squares regression with the mean-and-variance-corrected estimation approach to evaluate the chi-square goodness-of-fit of CFA. Four other indices were selected to assess the model fit: root mean square error of approximation (RMSEA), comparative fit index (CFI), normed fit index (NFI), and nonnormed fit index (NNFI). RMSEA is associated with the residuals in a model. The RMSEA value ranges from 0 to 1, and a smaller RMSEA value indicates a better model fit. A good model fit is usually defined as an RMSEA value of ≤0.06 [29], but a value of ≤0.08 is often considered acceptable [30]. CFI is an incremental fit index [31] that helps evaluate the overall improvement in a proposed model over an independent model in which the observed variables are uncorrelated [32]. NFI and NNFI are two other indicators that are used commonly to determine model fit [33]. For CFI, NFI, and NNFI, larger values indicate better model fit and values of >0.90 are considered acceptable.
RESULTS
Sociodemographic and psychiatric characteristics
The sociodemographic and clinical characteristics of the study participants are presented in Table 1. A total of 160 participants (129 male and 31 female) having a mean age of 44.2 years were enrolled. Of these participants, 43.1% were married, 72.5% had completed senior high school education or higher (more than 12 years), and 73.8% were employed. Regarding drinking patterns, the mean age at first drink was 16.8 years, mean age at tolerance development was 28.2 years, and mean amount of alcohol consumed per drinking day was 13.4 units, of which one unit is equivalent to 10 grams of ethanol.
Reliability
The PACS-C exhibited high internal consistency, as evident from a Cronbach’s α of 0.95 for the five items (Table 2). The item–total correlations were satisfactory and ranged from 0.88 to 0.94 for each item; the lowest correlation was noted for item 1. The test–retest reliability was determined to be 0.97 (p<0.001) after comparing the patient’s baseline scores on the PACS-C with those after 1 day (Table 3).
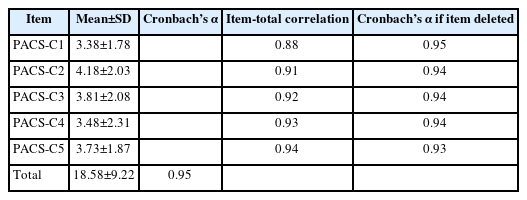
Item characteristics, Cronbach’s α, item-total correlations, and Cronbach’s α values if an item is deleted in PACS-C (N=160)
Validity
CFA results revealed a good fit under various models (Table 4). Under a single-factor structure, all five items exhibited satisfactory factor loadings (0.73–0.87) (Figure 1). The concurrent validities of the VAS and obsession and compulsion subscales of the YBOCS-hd-C were 0.81, 0.81, and 0.79, respectively. The SADQ-C (r=0.47) exhibited a moderate correlation with the PACS-C (Table 3).

Concurrent validity and test–retest reliability according to the correlation of PACS-C against VAS, SADQ-C, SADQ-C Severity, YBOCS-hd-C obsession subscales, and YBOCS-hd-C compulsion subscales (N=160)
DISCUSSION
This study demonstrated the PACS-C to have good internal consistency, with a Cronbach’s α similar to that of original version (Cronbach’s α=0.92) [15]. In addition, the test–retest results (performed at baseline and after 1 day) exhibited a high correlation, which implies that the PACS-C has good reliability. CFA results revealed a satisfactory model under the single-factor structure. Furthermore, the PACS-C showed good concurrent validity with other scales used to measure craving, such as the VAS and YBOCS-hd-C; however, it had only a moderate correlation with the SADQ-C, which is used to measure the severity of an individual’s dependence on alcohol. The moderate correlation between the PACS-C and the SADQ-C may result from their assessment of different dimensions of alcohol use disorder.
Alcohol use is a common but underestimated problem in Taiwan. The 2018 National Survey of Substance Use indicated that approximately 6% of the population aged 18–65 years in Taiwan exhibited a degree of alcohol use that is detrimental to health, which is defined as a score of ≥8 on the Alcohol Use Disorders Identification Test [34]. Furthermore, alcohol use is more common in inpatients than in general population. According to a survey conducted in a general hospital in Taiwan, approximately one-sixth of the patients admitted for reasons other than psychiatric problems had alcohol use disorder, but only one-quarter of them were identified by medical staff [35]. Recently, the Taiwanese government has started taking measures to reduce alcohol-related harm. One such strategy, for instance, is compelling drink-driving recidivists to receive treatment. Given the increasing recognition of the harm associated with alcohol use disorder, assessment tools must be developed to evaluate the symptoms associated with alcohol use disorder in Taiwan, particularly craving.
As a clinical tool for measuring craving, the PACS-C offers the following advantages. First, it is a single-dimension, multi-item tool for measuring alcohol craving and avoids vague definitions. Second, the PACS-C is a self-administered questionnaire. This reduces the risk of underreporting, which is common in patients with substance use disorder. Finally, the PACS-C has only five items, and each item is short; thus, the scale is less time-consuming and easy to complete.
The PACS can be used as a tool for predicting relapse. In a 9-month-long clinical trial, weekly assessments of alcohol craving using the PACS strongly predicted alcohol consumption in the subsequent week [17]. The PACS can also be used to classify inpatients with alcohol dependence and predict the time to relapse after discharge [19]. Follow-up studies are needed in Taiwan to validate whether the PACS-C can be used to predict relapse in patients with alcohol dependence.
This study has some limitations. First, test–retest reliability was measured in inpatients 1 day after the baseline measurements; however, craving level may vary on a daily basis. Nevertheless, this would more likely result in an underestimation rather than overestimation of the test–retest reliability. Second, the study participants were recruited from only one hospital and not the community. Because alcohol dependence severity and craving level vary widely across these patients, the PASC-C may be used for patients with varying degrees of dependence severity and craving. Finally, the possibility of underreporting cannot be disregarded, as it is common in similar studies centered on substance abuse. Nonetheless, the questionnaire used in the present study was self-administered and maintained user anonymity; thus, the risk of underreporting can reasonably be thought to have been low in this study. Past studies regarding alcohol consumption showed that the participants reported more often excessive drinking in the self-reported survey than in the face-to-face interviews, suggesting that alcohol drinking might be underreported in face-to-face interviews due to its social unacceptability [36].
In conclusion, the PACS-C appears to be a reliable and valid tool to measure alcohol craving in Taiwanese patients with alcohol use disorder. Further studies are warranted to validate the ability of the PACS-C to predict relapse in these patients.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Ming-Chyi Huang, Hu-Ming Chang. Data curation: Su-Chen Fang, Wei-Chien Huang, Hu-Ming Chang. Formal analysis: SuChen Fang. Funding acquisition: Hu-Ming Chang. Investigation: MingChyi Huang, Hu-Ming Chang. Methodology: Su-Chen Fang, Ming-Chyi Huang, Hu-Ming Chang. Project administration: Hu-Ming Chang. Resources: Ming-Chyi Huang, Hu-Ming Chang. Supervision: Hu-Ming Chang. Validation: Yu-Yu Ko, Hu-Ming Chang. Writing—original draft: Yu-Yu Ko. Writing—review & editing: Hu-Ming Chang.
Funding Statement
This research was supported by grants from Taipei City Government (TPECH 10901-62-037 and 11001-62-013 [Hu-Ming Chang]).