Development and Validation of the Korean Version of the Multidimensional Non-Suicidal Self-Injury Scar Scale
Article information
Abstract
Objective
Non-Suicidal Self-Injury (NSSI) scars are common in individuals with NSSI experiences. However, little is known about NSSI scars because related tools are limited. This study aimed to develop and validate the Korean version of the multidimensional Non-Suicidal Self-Injury Scar Scale (K-NSSI-ScarS), consisting of three components: NSSI scar measurement, NSSI scar cognition, and NSSI scar concealment.
Methods
A total of 333 Korean adults with at least one NSSI scar and history of NSSI within the last 5 years (age: 18 to 39 years) completed the online survey. We conducted exploratory (n=133) and confirmatory (n=200) factor analyses of NSSI scar cognition. To measure the internal consistency of each subfactor of the scar cognition and scar concealment components, we used Cronbach’s α. Kappa and intraclass correlation coefficients were used to measure the test-retest reliability of the entire scale. We also assessed the convergent and construct validity of the K-NSSI-ScarS.
Results
Factor analyses showed a 5-factor structure consisting of 23 items. Internal consistencies and test-retest reliability were excellent. The moderate correlation between the five subfactors of NSSI scar cognition and related concepts (e.g., acquired capability of suicide) confirmed the convergent validity. Lastly, moderate correlations were found between NSSI scar concealment, self-concealment, NSSI scar measurement information, and the five subfactors of NSSI scar cognition.
Conclusion
The results verify the psychometric properties and support the necessity of a multidimensional NSSI scar scale.
INTRODUCTION
Non-Suicidal Self-Injury (NSSI) is the act of directly and intentionally harming one’s bodily tissues without suicidal intent [1]. NSSI differs from other mental health problems because most cases leave distinct scars on the body [2]. Despite the growing academic interest in NSSI, surprisingly few studies have investigated NSSI scars [3-5]. More than half of individuals with a history of NSSI experience distress due to NSSI scars. NSSI scars are regarded as the result of unpleasant emotional experiences and are suggested to predict suicidal thoughts and suicide attempts [2]. Therefore, NSSI scars should be the focus of therapeutic interventions for NSSI, increasing the necessity for research. NSSI scars are often concealed due to stigmatization and prejudice from oneself and others [5]. Previous research linked the degree of NSSI scar concealment to negative scar-related cognitive experiences and revealed that NSSI scar concealment behaviors predicted future NSSI even after controlling for NSSI severity indices [3]. Therefore, a multidimensional approach should be taken when studying NSSI scars.
NSSI typically begins around the age of 12–14 and peaks at 16–24 [6]. Therefore, researchers and clinicians should pay attention to NSSI scars, as they can significantly impact one’s identity [7]. Moreover, because Koreans are typically conscious of how others evaluate them, they tend to care about how others see them much more than people in Western cultures do [8]. Therefore, interpretations of NSSI scars by oneself and others and their impact on one’s identity and social relationships could be important to NSSI interventions in Korea. However, NSSI scar-related scale is still limited.
Scar evaluation tools used in medical settings on patients with physical trauma provide limited information related to surgical intervention (e.g., scar width, and color) [9,10]. Moreover, no tool is available for measuring NSSI scar characteristics (e.g., location, time of occurrence, and subjective meaning). In addition, since NSSI scars may lead to negative cognitions (e.g., reminders of negative past experiences and shame) or positive cognitions (e.g., endurance in difficult times) [4], it is crucial to examine NSSI scar cognition. While Burke et al. [4] developed a tool to assess NSSI scar cognition, its psychometric properties have not been adequately established, nor has it been translated into Korean and subsequently validated. Furthermore, limited research has directly examined the effects of NSSI scar concealment [3], even though NSSI concealment behaviors make therapeutic intervention difficult. Therefore, if a tool to measure NSSI concealment behavior were to be developed, it would be possible to identify and intervene the problems faced by individuals who engage in NSSI. Therefore, a multidimensional psychological scale is needed to measure objective NSSI scar characteristics, related cognitive factors, and concealment behaviors.
The process of developing a multidimensional scale of NSSI scars includes constructing areas of evaluation and generating items based on a literature search and focus group interviews (FGIs). The Korean version of the multidimensional Non-Suicidal Self-Injury Scar Scale (K-NSSI-ScarS) consists of three sections: NSSI scar measurement, NSSI scar cognition, and NSSI scar concealment.
The first section measures objective NSSI scars and contains eight items assessing the presence, number, and locations of NSSI scars; information about the most meaningful scar (location, size, recency); the date when the last scar was created; and whether dermatologic surgery has been performed on the scars. Several studies have emphasized the need to explore the relationships between NSSI scars (e.g., size, number, location) and suicidal ideation, attempt, and scar-related negative experiences (e.g., shame) [4,7]. Therefore, we included items used in previous studies [3,4,11] and incorporated a figure of the human body. In addition, based on a literature review and interviews, items assessing the information related to a meaningful scar [11] and the date of the most recent scar occurrence were added.
The second section consists of 26 items regarding NSSI scar cognition. This component is a Korean-revised tool based on Burke et al.’s [4] Non-Suicidal Self-Injury Scar Cognition Scale (NSSI-SCS). The original scale suggests a 5-factor model with 23 items, comprising a social factor reflecting social stigma (e.g., “My scar(s) make me embarrassed in front of other people”), a reminder factor reflecting negative past experiences (e.g., “My scar(s) make me think about my failures and mistakes”), a suicide-related factor (e.g., “My scar(s) make me feel less afraid of dying”), a positive cognition factor (e.g., “My scar(s) make me feel tough, like I can get through anything”), and a weak cognition factor (e.g., “My scar(s) make me feel like I am weak”). We added two items for the social factor (“I think people judge me as having mental problems when they see my scars” and “I think my scars cause disadvantages in life”) and one item for the suicide factor (“My scars make me feel an urge to hurt myself”), which were developed based on FGIs.
The final section assesses NSSI scar concealment with 16 items. The first 5 items were developed based on literature reviews [3,4], checking for the prerequisites of scar concealment (e.g., noticeability of scars, desire to receive treatment for selfinjury scars, and degree of concealment intentions). The following 11 items measure behaviors performed to conceal selfinjury scars and were generated through the FGIs and literature reviews [12,13]. Identifying scar concealment methods is crucial as they hinder receiving timely and appropriate treatment. Considering the variations in concealment methods observed during the FGIs, influenced by participants’ NSSI characteristics (e.g., duration of NSSI, periods of cessation), we developed diverse items to enhance understanding and assessment of these methods. Examples of included methods are wearing band-aids, watches, bracelets, or other accessories; using cosmetics or wearing long-sleeved clothes; and avoiding certain activities or postures. All items are rated on a 5-point Likert scale (0=not at all, 4=very often).
The current study aimed to develop a K-NSSI-ScarS and confirmed its psychometric properties. First, using the NSSI scar measurement component, we sought to quantify participants’ NSSI scars by assigning them scores and determine whether these scores can serve as a meaningful objective index. In addition, we conducted exploratory and confirmatory factor analyses on the second section (NSSI scar cognition) to verify whether the original 5-factor model maintains and whether the original 23 items and the three newly developed items provide a stable, measurable value. We also examined correlation between K-NSSI-ScarS and related scales to establish its convergent validity. We predicted significant positive correlations between 1) the social factor and concerns about negative interpersonal evaluations or shame, 2) the suicide factor and acquired capability of suicide, 3) the reminder factor and event-related rumination, 4) the weak factor and shame, 5) the positive factor and positive changes in selfperception, and 6) NSSI scar concealment and self-concealment. Finally, we analyzed internal consistency and test-retest reliability to confirm whether the K-NSSI-ScarS provides reliable psychometric values. Through this study, we expect to provide a comprehensive measurement of NSSI scars and their utilization as significant indicators in clinical and therapeutic settings.
METHODS
Participants
Participants were recruited from advertisements posted in the online communities of 26 universities, snowball sampling and a bulletin board at the outpatient clinic of the department of psychiatry at Chung-Ang University Hospital from September to October 2022. The inclusion criteria were adults aged 18–39 with at least one NSSI mark or scar, no difficulty reading and answering the information and questions provided in this study, and their most recent NSSI experience within the last five years. Those with a history of suicide attempts or self-injuries causing serious physical damage requiring medical treatment (i.e., they were taken to the emergency room) in the past month, as well as those hospitalized due to the diagnosis of a mental disorder within the past month, were considered high-risk and were excluded from the study.
Among 428 participants who met the inclusion criteria, some respondents who gave inauthentic or duplicate responses (n=86) and outliers (n=9) were excluded. Thus, the data from 333 participants were included in the final analysis. Participants were randomly divided into two sample groups for the exploratory and confirmatory factor analyses. Sample 1 (n=133) contained 108 (81.2%) females and 25 (18.8%) males (Mage=22.13, standard deviation [SD]=2.99, range=18–33). Sample 2 (n=200) contained 172 (86%) females and 28 (14%) males (Mage=22.47, SD=3.41, range=18–34).
Measures
Korean version of the Multidimensional Non-Suicidal Self-Injury Scar Scale
The K-NSSI-ScarS is a self-report scale developed to measure the multidimensional psychological characteristics of NSSI scars. The K-NSSI-ScarS consists of 47 items and 3 components (8 items assessing NSSI scar measurement [Supplementary Figure 1 in the online-only Data Supplement], 23 items assessing NSSI scar cognition, and 16 items assessing NSSI scar concealment).
Korean version of the Event Related Rumination Inventory
The Korean version of the Event Related Rumination Inventory (K-ERRI) was developed by Cann et al. [14] and validated in Korean by Ahn et al. [15] It measures the rumination that arises after an individual experiences a stressful event. It consists of 10 items measuring intrusive rumination and 10 items measuring deliberate rumination on a 4-point Likert scale (1=not at all, 4=often). Intrusive rumination is associated with automatically emerging repetitive thoughts, iMages, and re-experiencing of events that induce emotional distress, while deliberate rumination is considered conscious thinking that focuses on the causes and meanings of events, thereby enhancing the potential for growth [16]. Therefore, we used only the 10 items measuring intrusive rumination by the Event Related Rumination Inventory-Intrusive (ERRI-I) subscale since the reminder factor of the K-NSSI-ScarS cognition section is considered negative cognition. The internal consistency of the ERRI-I was 0.96.
Post-Event Rumination Questionnaire
Kim’s Post-Event Rumination Questionnaire (PRQ) [17] is a self-report scale that measures post-event rumination that can occur in a social setting. It consists of three subscales (rumination on a failure of anxiety control, concerns about negative interpersonal evaluations, reviews of the past situation) comprising 26 items rated on an 8-point scale (0=not at all, 7=very much). We only utilized the 9 items from the Post-Event Rumination Questionnaire-concerns about negative interpersonal evaluations (PRQ-EVA) subscale because the social factor of the K-NSSI-ScarS cognition section represents stigma in a social context. The internal consistency of the PRQ-EVA was 0.95.
Internalized Shame Scale
The Internalized Shame Scale (ISS) was developed by Cook and Coccimiglio [18] and translated into Korean and validated by Lee and Choi [19]. The 30 items of this scale are rated on a 5-point Likert scale (0=never, 4=almost always). 24 items measure internalized shame, and 6 items from Rosenberg’s Self-Esteem Scale counteract the respondent’s tendency to answer in one direction. The internal consistency was 0.97 in this study.
Korean version of the Posttraumatic Growth Inventory
We measured the degree of positive change in self after experiencing an adverse event using the Korean version of the Posttraumatic Growth Inventory (K-PTGI), originally developed by Tedeschi and Calhoun20 and validated in Korean by Song et al. [21] This scale consists of four subscales (changed perception of self, the increase of interpersonal depth, finding new possibilities, the increase of spiritual interest) and 16 items rated on a 6-point Likert scale (0=did not experience this change, 5=experienced this change to a very great degree). In the current study, only the six items from the Posttraumatic Growth Inventory-changed perception of self (PTGI-CPS) subscale were used, as the positive factor of the K-NSSI-ScarS cognition section also emphasizes the terms “I” and “me.” The internal consistency of the PTGI-CPS was 0.91.
Acquired Capability for Suicide Scale
We used a Korean version of the Acquired Capability for Suicide Scale (ACSS), developed by Van Orden et al. [22] and translated by Jo [23]. It includes 20 items and measures the reduction of fear of death and tolerance for physical pain using a 5-point Likert scale (0=not at all like me, 4=very much like me). The internal consistency was 0.86 in the present study.
Hospital Anxiety and Depression Scale
We used a Korean version of Hospital Anxiety and Depression Scale (HADS), developed by Zigmond and Snaith24 and translated into Korean and validated by Oh et al. [25], which measures anxiety and depression based on a 4-point Likert scale. The HADS contains 14 items: Odd-numbered items measure Hospital Anxiety and Depression Scale-Anxiety (HADS-A), and even-numbered items measure Hospital Anxiety and Depression Scale-Depression (HADS-D). The internal consistencies of HADS-A and HADS-D reported in this study were 0.90 and 0.76.
Self-Concealment Scale
The Self-Concealment Scale (SCS) was developed and validated by Park and Lee [26]. It consists of 15 items and measures tendencies for concealment, possession of secrets, and fear of disclosure. All items are measured on a 5-point Likert scale, and the internal consistency was 0.91 in the present study.
Self-Injurious Thoughts and Behaviors Interview-Korean version-Short Form
The Self-Injurious Thoughts and Behaviors Interview-Korean version-Short Form (SITBI-K-SF) was developed by Nock et al. [27] and validated in Korean by Lee et al. [28] We used the short form, which can be conducted as a self-report questionnaire. Of the 5 types of modules that measure suicide/NSSIrelated thoughts and behaviors, we exclusively employed the NSSI module to ascertain whether participants had engaged in NSSI behaviors more than once within the past 5 years.
Procedure
First, we translated the items of the original NSSI-SCS into Korean. We received permission to translate and validate the NSSI-SCS from Burke et al. [4], the leading developer of the scale. An expert clinical psychologist with 12 years of experience, a doctor in clinical psychology, and a master’s student in clinical psychology performed forward translations. The items were then back-translated by an individual fluent in both languages with a master’s degree in clinical psychology. The back-translated items were compared with the original items and finalized.
In the second procedure, we conducted FGIs with eight individuals who met the inclusion criteria. Semi-structured interviews were conducted to gather insights on NSSI scars in the Korean sociocultural context. Four interviews were held, each lasting around 1.5 hours, with 1–3 participants per interview. Based on the interviews, 3 items were generated and added to the 23 original items.
Next, we completed the development of K-NSSI-ScarS, which consists of three components, and administered the online survey. Participants who fully completed the survey were compensated with a 10,000 KRW (approximately 8 dollars) gift card. Lastly, we checked the psychometric properties of the K-NSSI-ScarS according to the item types for each component by following data analysis steps. The procedures were approved by the Chung-Ang University Institutional Review Board (IRB No. 1041078-202205-HR-132) and all participants provided informed consent.
Data analysis
We utilized SPSS 26.0 (IBM Corp., Armonk, NY, USA) to calculate descriptive statistics and conduct exploratory factor analysis (EFA), reliability analysis, and correlation analysis. To examine the factor structure of the NSSI scar cognition (section 2), we conducted an EFA on Sample 1 (n=133). Factors were extracted using principal axis factoring. Promax rotation assuming a correlation between factors was employed. We examined the suitability of items by considering factor loading values of at least 0.40 or higher [29], and ensuring that the differences between factor loading coefficients on other factors were at least 0.10, thus avoiding cross-loading [30].
Next, we employed AMOS 26.0 (SPSS Inc., Chicago, IL, USA) to perform a confirmatory factor analysis (CFA) on Sample 2 (n=200). The sample size for CFA is determined based on the consideration that it is appropriate if it exceeds 150 [31,32]. To assess the model fit, we utilized relative fit indices, including the comparative fit index (CFI) and Tucker-Lewis index (TLI), as well as absolute fit indices, such as standardized root mean square residual (SRMR), and root mean square error of approximation (RMSEA). Generally, a model is considered reasonable if CFI and TLI are above 0.90, and SRMR and RMSEA are below 0.08 [33,34].
Cronbach’s α assessed internal consistency; values of at least 0.70 indicated acceptable reliability. To measure test-retest reliability, we used Kappa (κ) for categorical items and intraclass correlation coefficients (ICCs) for Likert-type items. Lastly, we used Pearson’s correlations to examine the convergent validity of scar cognition subfactors and the construct validity of K-NSSI-ScarS.
RESULTS
Characteristics of NSSI and NSSI scars
Among 333 participants, 28 (8.4%) engaged in NSSI only once in their lifetime, 109 (32.7%) engaged in NSSI 2–5 times, 103 (30.9%) performed NSSI 6–20 times, 42 (12.6%) performed NSSI 21–50 times, and 51 (15.3%) engaged in NSSI 51 times or more. Moreover, 89 participants (26.7%) had engaged in NSSI for less than one year, 138 (41.4%) had engaged in NSSI for 2–5 years, and 106 (31.9%) had engaged in NSSI for five or more years. Furthermore, 64 participants (19.2%) had only one NSSI scar, 149 (44.7%) had 2–5 scars, 68 (20.4%) had 6–20 scars, 33 (9.9%) had 21–50 scars, and 19 (5.7%) had 51 or more scars. In addition, participants reported having one or more scars on various parts of the body (e.g., wrist, thigh, and neck).
EFA
EFA was conducted on Sample 1 (n=133) for the 26 items regarding NSSI scar cognition. The Kaiser-Meyer-Olkin index was acceptable (0.85), and Bartlett’s sphericity test was significant (χ2=1,800.893, df=325, p<0.001), indicating that the data were suitable for factor analysis. The initial EFA revealed 6-factors with eigenvalues above 1.0. However, fewer than two items were loaded onto a factor, thus ruling out the 6-factor structure. Because the original scale suggested using five factors—and considering the point where the slope levels off in the scree plot (Supplementary Figure 2 in the onlineonly Data Supplement)—using at least four or five factors was deemed appropriate [35].
Therefore, to determine the appropriate number of factors, we set the number of factors to five, following the original study by Burke et al. [4], and re-analyzed the data. Twenty-five of the 26 items showed appropriate factor loadings (i.e., greater than 0.40). For 2 items, the difference between factor loadings on other factors was less than 0.10, weakening item discrimination. Thus, these 2 items were deleted, leaving 23 items to be finalized.
The final factor loadings ranged from 0.432–0.957. The first factor is the social factor, comprising 6 items related to social stigma or shame. The second factor is the positive factor, comprising 6 items related to hope and strength. The third factor is the weak factor, comprising 4 items from the original scale: two items from the weak factor, one from the reminder factor (item 6), and one from the social factor (item 8). The fourth factor is the reminder factor, comprising 3 items from the reminder factor and one from the weak factor (item 7) from the original scale. This factor reflects that NSSI scars remind people of negative experiences from the past (e.g., mistakes or failures, unwanted memories of the past, and stress). The fifth factor is the suicide factor, consisting of 4 items.
In summary, the EFA revealed 23 items in the cognition component with the same 5-factor structure as the original scale (social, positive, weak, reminder, and suicide). However, some different items comprised each factor. The final items and the EFA results are presented in Supplementary Table 1 (in the online-only Data Supplement).
CFA
We conducted CFA using AMOS 26.0 on Sample 2 (n=200) to confirm the 5-factor model of the NSSI scar cognition component. The results showed an overall acceptable model fit (χ2=509.052, df=220, p<0.001, Chi-squared fit statistic/Degrees of freedom [CMIN/DF]=2.314<3, SRMR=0.076) [36]. However, for the other model fit indices of the 5-factor structure, CFI=0.881, TLI=0.863, and RMSEA=0.081, which did not indicate a good model fit. Accordingly, modification indices (MI) were reviewed, showing that the covariance MI for the item pairs (1, 20), (3, 9), and (6, 8) exceeded 10, indicating a connection between the covariances of each pair of error terms [37]. As a result, the values for the modified 5-factor structure changed to χ2=433.497, df=217, p<0.001, CMIN/DF=1.998, and SRMR=0.069. Meanwhile, both fit indices increased to CFI=0.911, TLI=0.896, and RMSEA=0.071, indicating a good and acceptable model fit. Thus, the modified 5-factor structure was selected.
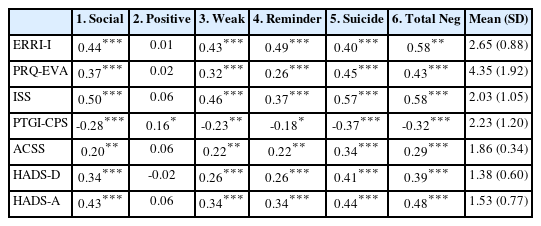
The factor structure of the finalized Korean version of the NSSI Scar Cognition Scale K-NSSI-SCS) and standardized coefficient estimations are presented in Supplementary Figure 3 (in the online-only Data Supplement). The means, SDs, and correlations between factors are presented in Table 1.
Reliability analysis
The Cronbach’s α values for all five factors of the K-NSSISCS (social, positive, weak, reminder, and suicide) indicated good internal consistencies (0.89, 0.81, 0.87, 0.79, and 0.82, respectively). Cronbach’s α for the scar concealment component was also good (0.82).
To measure the test-restest reliability of the K-NSSI-ScarS, we analyzed data from 51 respondents out of the 85 individuals who agreed to participate in additional research after a 6–8 week interval. The test-retest reliability was acceptable for the overall score (ICC=0.863, p<0.001), social factor (ICC=0.905, p<0.001), positive factor (ICC=0.754, p<0.001), weak factor (ICC=0.844, p<0.001), reminder factor (ICC=0.822, p<0.001), and suicide factor (ICC=0.844, p<0.001). The test-retest reliability of the categorical items in the scar measurement component, calculated using κ, showed strong consistency (κ=0.941). The test-retest reliability of Likert-scale items was calculated using ICC, which showed appropriate consistency for the number of scars (ICC=0.842, p<0.001). Finally, the test-retest reliability for the scar concealment component was calculated using ICC, demonstrating appropriate consistency (ICC=0.855, p<0.001).
Convergent validity
Correlations between subfactors of NSSI scar cognition and related scales
To confirm the convergent validity of the section 2, we examined the correlations between each subfactor and other related psychological scales (Table 2). Following Cohen’s criteria [38], correlation value of 0.1 is small, 0.3 is medium, and 0.5 is classified as large. Consistent with hypotheses, 1) the social factor was significantly positively correlated with PRQEVA (r=0.37, p<0.001) and displayed the highest correlation with ISS (r=0.50, p<0.001). Also, 2) the positive factor exhibited significant positive correlation solely with PTGI-CPS (r=0.16, p<0.05). Furthermore, the correlation analyses showed significant positive correlations of 3) the weak factor with ISS (r=0.46, p<0.001), 4) the reminder factor with ERRII (r=0.49, p<0.001, respectively), and 5) the suicide factor with ACSS (r=0.34, p<0.001). In addition, HADS, which measures depression and anxiety, showed significant positive correlations with all factors except the positive factor. These results imply satisfactory convergent validity for the K-NSSI-ScarS section 2 and suggest that the subfactors effectively measure distinct relevant domains.
Correlations between NSSI scar concealment and other variables
To confirm the construct validity of the NSSI scar concealment scale, we investigated the relationship between NSSI scar measurements (number of scars, size of the most meaningful scar, and time since the most recent scar), NSSI scar cognition, and the SCS. NSSI scar concealment intentions and behaviors were positively correlated with SCS, number of scars, and scar size, and negatively correlated with time since the last scar. In addition, concealment intention and concealment behavior showed significant positive correlations with all factors except the positive factor, confirming that greater scar concealment intentions and behaviors are linked to a higher degree of negative cognition regarding the scars. Detailed results are presented in Table 3.
DISCUSSION
This study aimed to develop and validate a tool to investigate the multidimensional psychological characteristics of NSSI scars in a Korean context. First, we unified clinically used items into a single NSSI scar measurement scale. We used a body figure to effectively identify scar location and examine the subjective meaning of the scar or treatment history, enhancing the suitability and usefulness of NSSI scar evaluations. Next, for the NSSI scar cognition component, new items were added to Burke et al.’s4 scale to align with Korean culture and then validated. The EFA and CFA confirmed a 5-factor structure (social, positive, weak, reminder, and suicide) for K-NSSI-SCS. Reliability analyses revealed appropriate internal consistencies and test-retest reliabilities, indicating that the items consistently and reliably measure the characteristics reflecting NSSI scar cognition.
K-NSSI-SCS retained the original scale’s 5-factor structure, albeit with three original items omitted and three items added through FGIs, totaling 23 items. Specifically, an original item from the suicide factor (“My scar(s) make me feel hopeless”) was deleted due to low factor loading. Furthermore, factor loadings of “My scar(s) make me feel like I can’t change anything, like I’m stuck” cross-loaded on suicide and weak factors, and “My scar(s) make me feel less afraid of dying” overlapped with suicide and positive factors; thus, these items were removed. For suicide cognition, rather than expressions indirectly related to death (e.g., “hopeless”), the inclusion of direct expressions such as “suicide” or “urge to hurt myself” was suggested to provide a sensitive measurement. Moreover, participants occasionally interpreted the meaning of “feel less afraid of dying.” positively. Despite the efforts to provide a sophisticated translation, the items originally developed in Korean appear to be more sensitive for measurement than the translated items.
In addition, item 8 (“My scar(s) make me feel shame”), originally assigned to the social factor, loaded on the weak factor. This is because, while shame is experienced in interpersonal relationships and social settings, it is a negative experience about oneself. Item 20 (“I think my scar(s) make me unique”) in the original scale, contrary to the authors’ expectation, was categorized under the suicide factor instead of the positive factor [4]. However, in this study, it was found to align with the intended positive factor as anticipated. Furthermore, the newly added items in the social factor concerning social stigma and social disadvantages had high factor loadings. Compared to Burke et al.’s study [4], this study showed higher scores for negative cognition factors and a lower score for the positive cognition factor. This suggests that the Korean sample may experience more negative cognitions related to NSSI scars, which could contribute to emotional and clinical difficulties.
Next, to confirm the convergent validity of the K-NSSISCS, we calculated the correlations between its subfactors and related scales. As expected, 1) the social factor was positively correlated with internalized shame and concerns about negative interpersonal evaluations. This finding is consistent with previous research showing that self-stigmatization and stigmatization from others are related to NSSI scars [3,39]. While 2) the positive factor showed a significant positive correlation with positive changes of self after a traumatic experience, the r value was slightly small. This outcome might be affected by the low score of the positive factor. Additionally, significant positive correlations were also found for 3) the weak factor with internalized shame, 4) the reminder factor with invasive rumination occurring after a stressful event, and 5) the suicide factor with acquired capability for suicide. These findings demonstrate the association between NSSI scars and ongoing suicidal thoughts, supporting previous research that highlights a strong connection between increased rumination about negative emotions and suicidal thoughts in individuals who engage in self-injury [2].
Finally, the scar concealment component was developed to measure the concealment intentions, methods, and degree. The findings provide strong evidence for the validity of the NSSI scar concealment component. Notably, there were significant positive correlations between NSSI scar concealment intention and methods with SCS. Additionally, significant positive relationships were found between NSSI scar con-cealment and subfactors of NSSI scar cognition, except for the positive factor. Particularly, strong correlations were observed with the social and suicide factors. Furthermore, the correlations between scar concealment and psychological characteristics were stronger than those with physical characteristics (e.g., the size or number of scars). Such findings support previous research that indicates the fear of stigma as a reason for concealing NSSI scars, the tendency to perform NSSI on easily hidden areas, and the use of band-aids and tattoos to cover scars [40].
The results provide several important implications. First, this is the first Korean study to specifically focus on NSSI scars and develop a multidimensional measurement tool that is reliable and valid. A key contribution of this study is the revision of the NSSI scar cognition component, aligning with the Korean cultural context. Unlike Burke et al. [4], we conducted CFA to assess the fit of the 5-factor structure, further enhancing the scale’s validity. Furthermore, the temporal stability of the scale was established through test-retest, increasing its psychometric validity and reliability.
Second, the K-NSSI-ScarS includes NSSI scar cognition, measurement, and concealment components. While the scar cognition component was named “cognition” in the original scale, it is more appropriately viewed as a tool that measures psychological attitudes towards scars. Therefore, the K-NSSIScarS is expected to provide a new avenue for NSSI evaluation and intervention. NSSI scars are associated with negative psychological attitudes, which may lead to concealment behaviors that exacerbate or prolong the problem. The K-NSSI-ScarS may enable clinicians to identify patients’ internalized psychological attitudes and concealment behaviors and provide proper intervention opportunities. Furthermore, ceasing NSSI is just one facet of recovery [41]. Previous research has shown that even after discontinuing NSSI, the emotional, behavioral, psychosocial problems, and vulnerabilities that accompanied NSSI tend to persist in the long term [42]. Therefore, the cessation of NSSI does not necessarily indicate the end of clinical risks and the need for NSSI-related treatment. As NSSI behaviors leave permanent scars on the body, therapeutic interventions should prioritize addressing psychological attitudes towards scars, mitigating their adverse effects, and, if necessary, considering dermatologic or plastic surgical inteventions [43].
Limitations and conclusion
The limitations of this study and suggestions for future studies are as follows. First, the insufficient EFA sample size were due to participants characteristics (recent NSSI experiences and resulting scars), but consistent 5-factor results from both EFA and CFA were achieved. Also, there are suggested criteria to consider item-to-participant ratios (e.g., 1:2 or 1:5) for determining the appropriate number of participants in EFA [31,44]. Second, this study recruited participants from various sources to include individuals who are comparable to clinical and subclinical populations. As a result, many participants represented a clinical (30%; at least 5 NSSI experiences in the past year) or a subclinical group (27%; 1–4 NSSI experiences in the past year). However, most participants were female university students, limiting the generalizability of the K-NSSI-ScarS. Therefore, future studies should aim to recruit participants from diverse age groups and consider validating the factor structure in a male sample. Furthermore, among the participants recruited from both hospital outpatients and university communities, there were individuals who were undergoing hospital follow-ups. However, this study did not consider the presence of comorbid conditions. Therefore, future research should examine comorbidities in individuals engaging in self-harm behaviors. Lastly, this study measured cognition and concealment behaviors of NSSI scars cross-sectionally and performed correlation analyses. Thus, causal relationships or sequential outcomes could not be determined. A longitudinal study is needed to investigate whether NSSI scar cognition leads to scar concealment behaviors, NSSI repetition, suicidal urges and exacerbation of emotional symptoms.
Despite the limitations mentioned, this study successfully developed and validated the K-NSSI-ScarS, establishing its psychometric properties. This lays the groundwork for future research on NSSI scars and offers insights for therapeutic interventions. We expect this study will inspire further investigations on NSSI scars in the Korean context and contribute to the implementation of effective therapeutic approaches.
Supplementary Materials
The online-only Data Supplement is available with this article at https://doi.org/10.30773/pi.2023.0193.
Exploratory factor analysis results of the K-NSSI-SCS
Korean version of the multidimensional Non-Suicidal Self-Injury Scar Scale (K-NSSI-ScarS): Non-Suicidal Self-Injury (NSSI) scar measurement section.
Scree plot of exploratory factor analysis for Korean version of the Non-Suicidal Self-Injury Scar Cognition Scale (K-NSSI-SCS). The scree plot indicates 4–5 factor solutions.
A 5-factor structural model of the Korean version of the Non-Suicidal Self-Injury Scar Cognition Scale (K-NSSI-SCS). Estimates represent stadardized factor loadings and correlations among the factors of the K-NSSI-SCS. Arrows between e10 and e11, e13 and e16, e17 and e19 indicate the addition of error paths based on modification indices (MI) tests.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Seo Jeong Lee. Data curation: Jinwoo Myung, Young-Sil Kwon. Formal analysis: Jinwoo Myung. Funding acquisition: Seo Jeong Lee, Jinwoo Myung. Investigation: Jinwoo Myung, Myoung-Ho Hyun. Methodology: Seo Jeong Lee. Software: Jinwoo Myung. Validation: Young-Sil Kwon, Myoung-Ho Hyun, Jinwoo Myung. Writing—original draft: Seo Jeong Lee, Jinwoo Myung. Writing—review & editing: Seo Jeong Lee, Myoung-Ho Hyun, Young-Sil Kwon.
Funding Statement
This work was supported by the Ministry of Education of the Republic of Korea and the National Research Foundation of Korea (NRF-2022S1A5A8053321). In addition, this research was supported by the Chung-Ang University Graduate Research Scholarship Grants in 2022.