 |
 |
- Search
| Psychiatry Investig > Volume 20(8); 2023 > Article |
|
Abstract
Objective
Methods
Results
Notes
Availability of Data and Material
The data from this study cannot be made publicly available to protect participants’ information. Inquiries about the data can be referred to the corresponding author [HY, LEE, hylee@catholic.ac.kr].
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Seongju Kim, Mi-Sun Lee, Hooyeon Lee. Formal Analysis: Seongju Kim, Mi-Sun Lee, Hooyeon Lee. Investigation: all authors. Methodology: Seongju Kim, Hooyeon Lee. Project administration: Hooyeon Lee. Data curation: Seongju Kim, Dong Jun Kim. Supervision: Hooyeon Lee. Validation: Seongju Kim, Hooyeon Lee. Visualization: Seongju Kim, Dong Jun Kim. Writing—original draft: Seongju Kim. Writing—review & editing: Mi-Sun Lee, Hooyeon Lee.
Funding Statement
This study was supported by the National R&D Program for Cancer Control through the National Cancer Center (NCC) funded by the Ministry of Health & Welfare, Republic of Korea (Grant number: HA21C0225) and the Catholic Medical Center Research Foundation made in the program year of 2022 (Grant number: 5-2022-B0001-00207).
Figure 1.
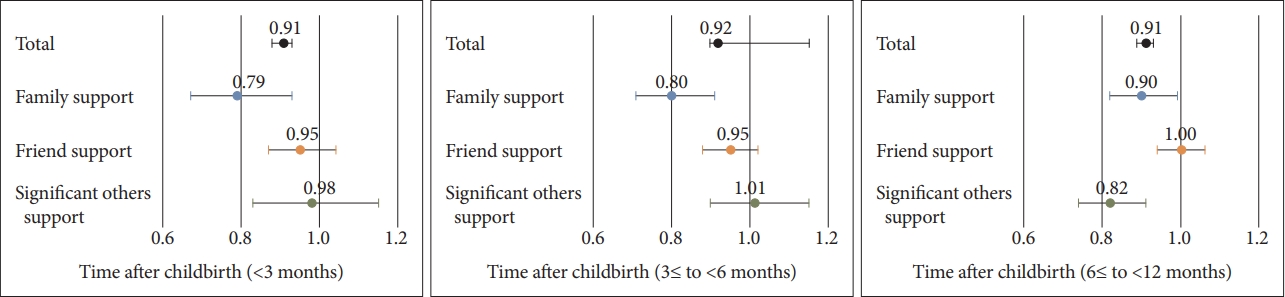
Table 1.
Table 2.
| Variables | aOR* | 95% CI | p |
|---|---|---|---|
| Social support | 0.91 | 0.90-0.93 | <0.001 |
| Age | |||
| 20-29 yr | 1 | ||
| 30-39 yr | 0.89 | 0.64-1.23 | 0.551 |
| 40-49 yr | 0.65 | 0.37-1.15 | 0.158 |
| Current employment status | |||
| Unemployed | 1 | ||
| Employed, full or part time | 1.30 | 0.82-2.04 | 0.381 |
| Employed, maternity leave | 1.13 | 0.86-1.48 | 0.948 |
| Education level | |||
| ≤High school | 1 | ||
| ≥College | 0.90 | 0.64-1.24 | 0.495 |
| Household monthly income | |||
| <3,000,000 KRW | 1 | ||
| 3,000,000-5,000,000 KRW | 0.95 | 0.72-1.25 | 0.687 |
| ≥5,000,000 KRW | 0.82 | 0.57-1.18 | 0.282 |
| Quality of sleep | |||
| High | 1 | ||
| Moderate | 1.62 | 1.12-2.33 | 0.588 |
| Low | 3.02 | 2.11-4.33 | <0.001 |
| Past depressive disorder | |||
| No | 1 | ||
| Yes | 2.22 | 1.40-3.53 | 0.001 |
| Parity | |||
| 1 | 1 | ||
| ≥2 | 0.99 | 0.77-1.28 | 0.957 |
| Time after childbirth | |||
| <3 mo | 1 | ||
| 3≤ to <6 mo | 0.98 | 0.72-1.34 | 0.371 |
| 6≤ to <12 mo | 1.23 | 0.92-1.64 | 0.371 |
| Type of pregnancy | |||
| Spontaneous | 1 | ||
| Used Fertility | 1.35 | 0.86-2.09 | 0.190 |
| Type of delivery | |||
| Vaginal | 1 | ||
| Cesarean section | 0.95 | 0.75-1.22 | 0.709 |
| Planned pregnancy | |||
| Yes | 1 | ||
| No | 1.40 | 1.08-1.81 | 0.011 |
Table 3.
|
Variable |
Crude OR | 95% CI | aOR* | 95% CI | |
|---|---|---|---|---|---|
| Time after childbirth | Social support | ||||
| <3 mo | Total | 0.90 | 0.88-0.93 | 0.91 | 0.88-0.93 |
| Family | 0.74 | 0.69-0.80 | 0.79 | 0.67-0.93 | |
| Friends | 0.83 | 0.78-0.88 | 0.95 | 0.87-1.04 | |
| Significant others | 0.77 | 0.71-0.82 | 0.98 | 0.83-1.15 | |
| 3≤ to <6 mo | Total | 0.91 | 0.89-0.93 | 0.92 | 0.90-0.94 |
| Family | 0.76 | 0.71-0.82 | 0.80 | 0.71-0.91 | |
| Friends | 0.84 | 0.80-0.89 | 0.95 | 0.88-1.02 | |
| Significant others | 0.80 | 0.75-0.85 | 1.01 | 0.90-1.15 | |
| 6≤ to <12 mo | Total | 0.90 | 0.88-0.92 | 0.91 | 0.89-0.93 |
| Family | 0.76 | 0.72-0.81 | 0.90 | 0.82-0.99 | |
| Friends | 0.86 | 0.82-0.90 | 1.00 | 0.94-1.06 | |
| Significant others | 0.74 | 0.70-0.79 | 0.82 | 0.74-0.91 | |
* adjusted by age, current employment status, education level, household income, quality of sleep, past depressive disorder, parity, time after childbirth, type of pregnancy, type of delivery, and planned pregnancy. PPD, postpartum depression; OR, odds ratio; CI, confidence interval; aOR, adjusted odds ratio
REFERENCES
-
METRICS

-
- 0 Crossref
- 1 Scopus
- 1,973 View
- 55 Download






