Social Stigma and Discrimination Toward People With Drug Addiction: A National Survey in Korea
Article information
Abstract
Objective
This study aims to understand the attitudes, stigma, and discrimination of the general adult population toward drug addiction.
Methods
We conducted a cross-sectional nationwide survey with 1,020 Korean adults using an Internet web-based panel. Self-reported data were collected on demographics, experience with substance abuse, perceptions of narcotic analgesic use, beliefs about the legalization of cannabis use, coping with substance abuse and addiction, and perceptions of drug risks. All statistical analysis in this study utilized the IBM SPSS Statistics 26 program.
Results
In this study, 1.6% of the participants reported abuse of opioid analgesics, 88.0% reported negative perceptions of drug addiction, and 76.9% reported agreeing to unfair treatment of drug addicts. Logistic regression analysis found that perceived stigma was more prevalent among women (odd ratio [OR]=2.087, p<0.01), old adults (OR=1.939, p<0.01), those with no personal experience of opioid misuse (OR=8.172, p<0.05), and those who were non-smoking (OR=2.011, p<0.01). In addition, the discriminatory attitude was more prevalent among participants with higher income (OR=1.989, p<0.001) and those who are non-smoking (OR=1.608, p<0.05).
Conclusion
This study provides information and guidelines for public intervention in drug addiction by identifying factors influencing social stigma and discriminatory behaviors toward drug addiction. The findings suggest that education on drug addiction prevention for the general adult population is necessary, and this education should include knowledge on coping with drug addiction and reducing stigma and discrimination toward drug addicts.
INTRODUCTION
Drug addiction is a global problem that requires complex efforts to solve [1]. In the Korean data reported in September 2021, the number of drug offenders increased by 327.8% and the number of narcotic drug abuse cases also increased by 10.3%, compared to that of the previous year (2020) [2]. In the UK, around 1% Britons of the total population are dependent on narcotic drugs [3], and around 730,000 people are receiving opiate replacement therapy across the EU [4], while the mortality rate from opioid overdose continues to rise [5]. Although the results of these country-specific drug addiction surveys indicate that there is evidence of the increasing severity of drug addiction, factors should be considered when preparing measures to treat addiction.
In particular, the stigmatization and discrimination of individuals with substance use disorder (SUD) serve as an important barrier for them to seek and continue treatment for drug addiction. In previous studies, in the UK’s attitudes toward substance dependence and treatment strategies study, only 35% agreed to pay for medical services for drug addiction treatment [6]. The Polish study explains that the “common good” view of drug dependence as a social and medical problem requiring medical support is collapsing [7]. A more recent Scottish survey of adults found public opinion against the use of vast government budgets and available resources to treat drug addicts [8]. The need for further investigation has been noted as the stigma of drug addiction and related discrimination can have a negative effect on solving drug addiction problems [9]. The results of some supporting follow-up studies stated that people have a basic aversion to narcotic drug users, with an attitude that it is unnecessary for them to receive treatment, and that socially trying to treat them is necessary to maintain a social balance. It has also been suggested that increasing people’s knowledge about drugs is associated with more positive attitudes toward individuals with drug addiction [10]. Evidence is also emerging that there is a strong link between the stigma and difficulties faced when treating narcotic drug addicts [11,12]. However, limited research has explored how the public views drug addiction, whether attitudes toward addicts influence the amount of resources the public has to pay to solve the problem of drug addiction, and the method of intervention [13,14].
What is observed in the literature is that social stigma and discrimination are barriers that keep addicts from accessing professional services. Individuals with SUD are afraid of attending medical institutions or therapeutic programs and of being labeled as a problematic person in the community in which they work. This indicates that people who are afraid of stigma and discrimination may be induced to move away from the community, where they can easily get help from family, relatives, and friends, and seek treatment facilities or shelters in remote places [15]. Even people who became addicted to drugs after using opioids are thought to be dependents involved in drug-related crimes. The negative views of these people contribute to social exclusion of the drug addicts and prevent them from trying to improve their lives or access health care services. They feel ignored and shamed by people’s stigma and discrimination, are unable to seek help when needed, or have difficulty completing therapeutic interventions [16,17].
Moreover, it is not just the average person who has a negative attitude toward drug addiction. The negative attitudes healthcare professionals have toward them also have a detrimental effect on the individual’s access to medical care in pharmacies and treatment institutions [18]. It has been found that when healthcare professionals develop negative attitudes toward drug-abusing individuals, they can also increase inaccuracy in making medical diagnoses [18]. In caring for patients with substance abuse, the healthcare professionals feel that the individuals are responsible for their illegal drug use, which leads to a decrease in sympathy and respect for the patients, and hence results in the loss of focus when caring for the patients [19].
As such, the existing literature mainly focuses on the negative relationship between stigma and discrimination for drug addiction, but studies on the individual characteristics that influence stigma and discrimination are lacking. Although some studies suggest that the majority of the general public support policies designed to help with drug addiction, discriminatory attitudes are found toward drug addiction in their actual behavior [20,21]. It seems to suggest that there is a difference in attitudes toward drug addiction and relationships with people suffering from drug addiction [20]. Stigma and discrimination for drug addiction can vary widely across countries and cultures, but because of their conservative cultural characteristics, Koreans tend to have poor understanding in mental illness and poor acceptance for the need of treatment [21], with little research being conducted on drug addicts in Korea.
This suggests that factors influencing undeserving behavior and discrimination based on the stigma associated with a reputation for drug addiction can be distinguished, and policies can be developed to reduce stigma and discrimination as our understanding of these factors increases and action is taken. Therefore, this study aims to investigate the relationship between the personal characteristics of the general adult population and their perceptions and attitudes toward drug addiction, and the effect of personal characteristics on discriminatory behavior that imposes a negative reputation and discomfort on drug addicts. A cross-sectional nationwide survey was conducted with 1,020 Korean adults, and self-reported data were collected on demographics, experience with substance abuse, perceptions of narcotic analgesic use, beliefs about the legalization of cannabis use, coping with substance abuse and addiction, and perceptions of drug risks.
METHODS
Participants and procedure
This study was conducted in Korea from May 20, 2020 to June 1, 2020, and data were collected from adults, including men and women, aged 19 years or older, nationwide through a web-based national survey titled “Public Awareness Survey on Drug Misuse and Abuse.” The questionnaire used in this study was empirically produced and reviewed through sufficient discussion involving an advisory committee composed of addiction psychiatrists from the Health Promotion Center and Tertiary Teaching Hospital. The national population was categorized by region and by gender and age (in 10-year units), and a sample was extracted using a stratified random sampling method from an access panel owned by Hankook Research (https://www.hrc.co.kr/) composed of voluntary participants. An email with an online link to the survey was sent to 1,252 sampled participants. Among these, 232 dropped out due to incomplete information. The final 1,020 participants who responded to the survey received a $7.5 electronic gift card for completing the survey. Voluntary participants filled out the questionnaire online, and they understood the right to refuse the survey and that there was no penalty for discontinuation. In addition, a detailed explanation of the survey contents and compensation was given in advance, and the participants provided written consent, and the researcher provided a written guarantee of anonymity and confidentiality.
The study design was approved by Hallym University Chuncheon Sacred Heart Hospital Institution Review Board (IRB: 2020-08-008-003).
Measures
The items for stigma and discrimination were extracted from the questions used in previous studies on stigma and stereotypes of drug addicts and people with mental illness [14,22-25]. First, the questions for stigma consisted of two items: “If someone in your family were to marry a drug addict (dependent), how much would you agree with this situation? (deny as family)” and “If a person who is addicted to drugs (dependent) starts working by your side at work, how much would you agree with this situation? (deny as colleague).” Responses were measured on a 5-point Likert scale, with 1 representing “strongly disagree” and 5 representing “strongly agree.” All of the questions for stigma were inversely scored. A higher average score indicates more stigma toward drug addicts.
The questions for discrimination consisted of two items: “What is your opinion on ‘the landlord has the right to refuse a person who is addicted to drugs (dependent) as a tenant’? (deny for housing)” and “What is your opinion on ‘employers have the right not to hire people with drug addiction (dependence) as employees’? (deny for employment).” The items were measured on a 5-point Likert scale, with 1 representing “strongly disagree” and 5 representing “strongly agree.” A higher average score indicates more severe discrimination toward drug addicts.
The clinical characteristics of the participants included narcotic analgesic misuse (yes vs. no), drinking in the past one year (yes vs. no), and smoking status at present (yes vs. no). In addition, it collected information about participants’ demographic characteristics, the items were measured on a 5-point Likert scale, perceptions of the effectiveness of drug addiction treatment (“Do you agree that many symptoms of drug addiction can be sufficiently improved through appropriate treatment?”), coping with substance abuse and addiction (“Do you agree to seek medical treatment in a hospital if suffering from narcotics and substance abuse and addiction symptoms?”), the government’s role in and support for substance abuse and addiction (“Do you agree that government should increase support and investment spending to develop and operate treatment programs for drug addiction?”), and perceptions of the causes of substance abuse and addiction (“What do you think of addiction/dependence?”).
Data analysis
All statistical analysis in this study utilized the IBM SPSS Statistics 26 program (IBM Corp., Armonk, NY, USA). Descriptive statistics were used to analyze participants’ responses and demographics; analysis of variance was used to examine differences between groups; Pearson’s correlation analysis was used to analyze the correlation of different traits with stigma and discrimination; and multiple regression analysis was used to confirm the influence of latent variables on the two dependent variables: stigma and discrimination. All statistical significance was analyzed based on α=0.05.
RESULTS
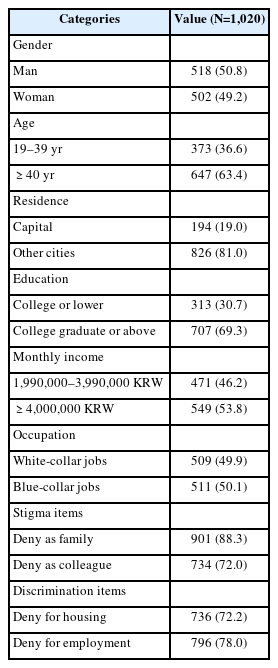
A vast majority of study participants agreed with stigma and discrimination toward drug addiction. We identified a very high level of desire to exclude drug addicts in both the questions of stigma and discrimination. A large percentage of participants were reluctant to allow drug addicts (dependents) to marry into their own families (deny as family; 901, 88.3%) or work with them at work (deny as colleague; 734, 72.0%). Participants agreed that it was justifiable for landlords to reject drug addicts as tenants (deny for housing; 736, 72.2%) or for employers to deny them employment (deny for employment; 796, 78.0%) (Table 1).
Table 1 presents the demographic characteristics of the participants. Among the 1,020 participants, there were 518 men (50.8%) and 502 women (49.2%). Most of them lived in regions other than the capital (826, 81.0%) and had a college degree or higher (707, 69.3%). About half reported that their monthly household income was over 4 million KRW (549, 53.8%) and that they worked in white-collar occupations (509, 49.9%).
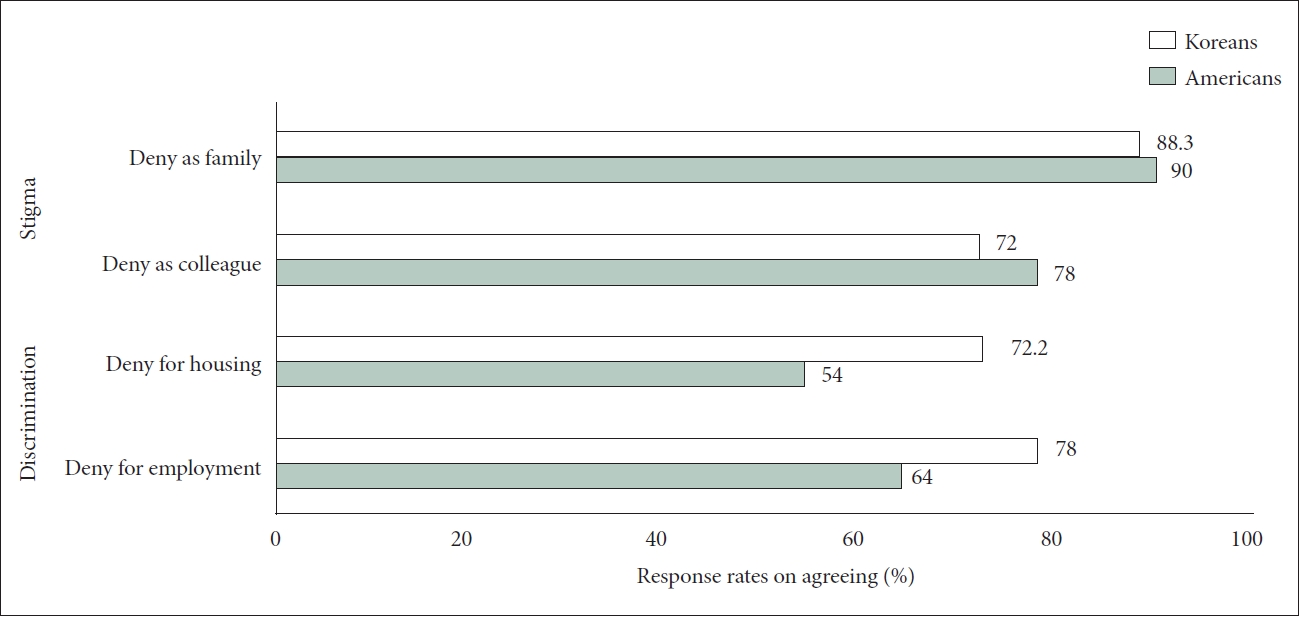
Figure 1 presents a comparison of response rates on agreeing to stigma and discrimination toward drug addiction between the results of the current study and that of the previous study. Compared to the study of Barry et al. [22] on Americans, the results of the current study with Koreans were slightly lower in the stigma item, and higher on a tendency to agree on discriminatory behavior toward drug addiction in the discrimination items.
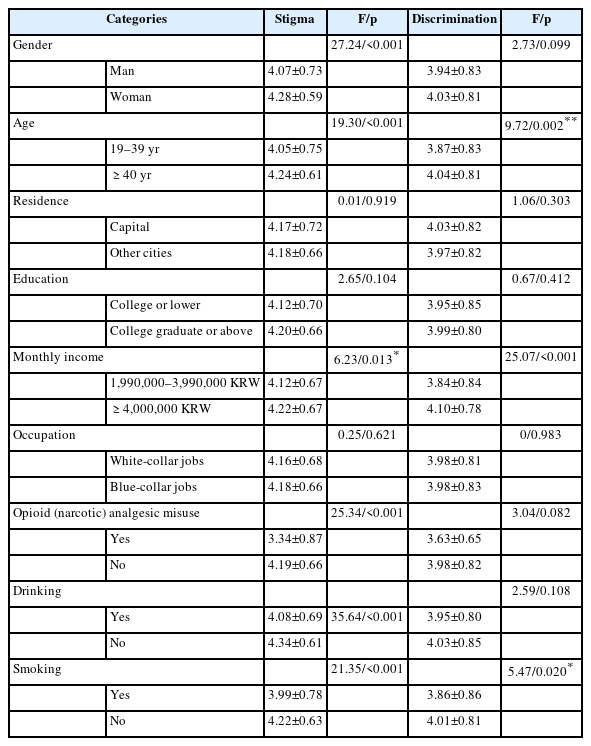
Table 2 shows the mean difference between stigma and discrimination according to the characteristics of the entire sample. The overall means and standard deviations of the items for stigma and discrimination were 4.17±0.67 and 3.97±0.82, respectively, with higher values indicating greater agreement on stigma and discrimination. Gender, age, and income level are significantly related to responses to stigma and discrimination. Women reported higher level of agreement on stigma than men, and participants in the ≥40 years age group agreed more strongly with stigma and discrimination than did participants aged 19–39 years. The high-income group (≥4,000,000 KRW) agreed more strongly with stigma and discrimination toward drug addiction than the lower-income participants (1,990,000–3,990,000 KRW).
In terms of clinical characteristics, most substance experiences are significantly related to stigma and discrimination. People with “no history of opioid pain analgesics misuse” were more likely to agree with the stigma of drug addiction. People who “do not consume alcohol” were more likely to agree with the stigma as well. “Non-smokers” agreed more strongly with both stigma and discrimination toward drug addiction than smokers. Although no significant difference was found, non-drinkers was more likely to agree with the stigma (p=0.06).
Table 3 shows the correlation coefficients of all variables measured in this study. The relative power of other variables on stigma and discrimination showed a significant difference. Participants who were woman, with higher age, and with higher monthly income were more positively correlated with the stigma. In addition, participants with experience of opioid (narcotic) analgesics, drinking alcohol, and smoking showed significant negative correlations with stigma. Conversely, age and monthly income showed a significant positive correlation with discrimination, and smoking was the only variable showing a negative correlation, implying that there are differences between stigma and discrimination.
Logistic regression analysis showed that being woman (odd ratio [OR]=2.087, p<0.01), old age (≥40 years; OR=1.939, p<0.01), non-experience of opioids (narcotic) analgesics misuse (OR=8.172, p<0.01), and non-smoking (OR=2.011, p<0.01) had significant effects on stigma. High monthly income (≥4,000,000 KRW; OR=1.989, p<0.001) and non-smoking (OR=1.608, p<0.05) were found to have significant effects on discrimination. Participants who agreed to seek medical treatment in a hospital if suffering from narcotics and substance abuse and addiction symptoms (medical treatment; OR=1.998, p<0.01), and those disagreed that the government should increase support and investment spending to develop and operate treatment programs for drug addiction (government support; OR=8.251, p<0.05) were found to have a high probability of agreeing to stigmatization. Additionally, participants’ views on what they perceived as causes of addiction—personal character, will, and bad habits and mental illness, loss of brain control—had no significant effect on the probability of agreeing to stigma and discrimination (Table 4).
DISCUSSION
This study investigated stigma and discriminatory behavior toward drug addiction in a national sample of adults in Korea. We also explored factors related to demographic characteristics that may influence stigma and discriminatory behavior toward drug addicts. In this study, 88.3% (deny as family) and 72.0% (deny as colleague) of all participants reported that they agreed with the stigma toward drug addiction. Factors related to stigma included gender, age, household average monthly income, opioid analgesics misuse experience, alcohol consumption, and smoking. The factors that were found to have significant influences on stigma included gender, age, opioid analgesics misuse experience, smoking, agreement to medical treatment toward drug addiction, and disagreement to increase government support. However, factors related to discrimination appeared to be age, monthly income, and smoking, and only monthly income and smoking were identified as significant influencing factors.
Compared to the results of the studies on stigma and discrimination targeting American adults (USA: stigma 78%–90%, discrimination 54%–64%) [22], this study showed that the stigma score for Korea was lower than that of the United States, and the discrimination score was higher for Korean adults (KOR: stigma 72.0%–88.3%, discrimination 72.2%–78.0%). The general public’s attitude toward drug addiction is related to their demographic and social characteristics [26]. Since this study showed a high consent rate for discriminatory behavior, further research on “discrimination” is needed. In a previous study, 83% of participants reported experiencing some form of discrimination [27]. Discrimination can cause individuals to be isolated from their families, rejected by their coworkers, and excluded from the society [28]. The discrimination is positively correlated with suicide attempts among transgender people, and that intimidation from others has a greater impact on their social isolation [29]. As such, there are a few studies on discrimination, but studies comparing it with stigma are lacking. In this sense, it suggests that more research on discrimination is needed.
We identified several factors associated with stigma and discriminatory behavior toward drug addiction. Adults who had not abused opioids were more likely to stigmatize drug addiction in thoughts and behaviors. In addition, we found that participants who had no smoking history were more likely to form stigma and discrimination toward drug addiction. This phenomenon can be explained by the familiarity hypothesis [30]. We can expect that people who have experienced substance abuse will be able to increase their understanding of the addict’s situation and reduce stigma and discriminatory behavior through personal and secondhand experiences with drugs [14]. However, more research is needed to understand the role of familiarity on stigma and discrimination toward drug addiction. In a study with a large Asian American population, which includes Korean Americans, Asian Americans had the lowest rates of service use and help-seeking attempts for psychiatric problems among other racial groups in the United States; moreover, Asian Americans tend to delay seeking hospital care until their psychiatric symptoms become chronic and severe [21].
This study found that participants’ drug experiences were associated with stigma and discrimination toward drug addiction. This suggests that positive attitudes toward drug addicts can be regarded as having feelings of compassion for them, while negative attitudes have been associated with devaluation of the groups [19]. As data on stigma and discrimination can be expressed in various ways in different social situations and therapeutic settings, and these influences can also affect the treatment services patients receive [22], investigation on stigma and discrimination in the general public and the data from this study can help reduce bias in therapeutic interventions and health care.
There appears to be heterogeneity in stigma and discriminatory attitudes toward drug addicts. In this study, there were more factors affecting stigma than discrimination. Researchers have yet to come to any clear conclusions about how to measure and analyze stigma and discrimination separately and objectively [31,32]. Previous studies [33,34] conceptualized stigma as internalized, perceived, anticipated, or enacted stigma, and some studies [35-37] defined enacted stigma as discrimination. Stigma is sometimes classified as an internalized form, and discrimination also refers to unfair treatment based on one’s status, which is one aspect of stigma [38,39]. As defined in our study, stigma is defined as the perception of belonging to a group and the internalized aversion to and rejection of belonging to that same group, while discrimination is a conceptualization of an externalized attitude toward the expected poor and unfair treatment and consequences for the target.
One of the findings was that older people had greater stigma. Young people may have less experience of the harmful effects of drug addiction, while older generations, through direct and indirect experiences, already have negative views about drug addiction and hence support more discriminatory treatment [40]. Regarding the demographic data, gender had significant effects on stigma as well. Women had more negative thoughts about drug addiction than men. These results were consistent with previous studies reporting the effects of heightened vigilance due to women’s vulnerability to drug problems [41]; women disabled by drug use are physically more vulnerable than men and are more likely to be targeted when exposed to crime [42]; woman drug addicts are exposed to an exploitative environment [43], and the effects of drugs can affect women’s defensive behavior to protect themselves and their ability to actively express themselves [44].
In this study, it was found that those who thought that they should receive active counseling or hospital treatment when suffering from opioids and drug abuse were more likely to agree to stigmatization than those who tried to solve it personally. Moreover, people who are reluctant to see governments increasing support and investment toward drug addiction are more likely to agree to stigmatization. According to previous studies, experts have pointed out the stigma and discriminatory medical services toward drug addiction. Efforts to explain drug addiction as a brain disease can potentially increase the negative stigma effect in the perspective and perception toward drug addiction and show that it can lower expectations about people’s chances of recovery [45]. Stigma and discrimination toward drug addiction has side effects such as denying and blaming of individuals with drug addiction, and exempting government from their responsibility in drug addiction [46-48].
As a study confirming this negative effect of stigma and discrimination, previous studies conducted on HIV patients found that stigma reduced clinical intervention for individuals suffering from depression [49]. In a questionnaire among Indian HIV clinicians, 62% of participants were neutral or agreed with the statement that “depression is a sign of personal weakness,” and 53% of participants felt it was difficult to work with someone who was depressed [50]. Other studies have shown that specialized approaches, subject to stigma and discrimination, impede the exercise of the rights of drug addicts and hinder their access to health care services [51,52]. Many people choose not to seek help from treatment services as a way to deal with stigma and discrimination and to avoid being “labeled” owing to possible negative consequences. Not having access to treatment services can actually exacerbate substance abuse problems, which can create a false perception that drug addiction treatment services are unnecessary, resulting in the devaluation of treatment services [53].
Economic status was one of the characteristic factors related to discrimination. In this study, people with middle or higher economic status agreed more to discriminatory behavior. In line with these results, there is a study that suggests stigma and discriminatory behavior increase with socioeconomic status [40]. In contrast, a study reported that the probability of wealthy people having a discriminatory attitude is lower than that of the very poor people because wealthy people have free access to various communications such as mass media and social media, and may obtain knowledge and information on drug addiction easily [26]. However, in these studies, the concepts of stigma and discrimination are used interchangeably. Regarding these differences, this study distinguished the concepts of stigma and discrimination more clearly, and in particular, the items for discrimination were contents that related to “economic loss.” Therefore, it seems that wealthy people honestly expressed their conservative position in protecting their property rights as “landlords” and “employees.”
In this sense, as a way to prevent stigma and successfully reduce discrimination, it is suggested that experts who treat drug addiction and the institutions in charge of their education should include appropriate evidence-based materials in the educational curriculum [18,54]. It suggests that these efforts should be made with the general public to help change their attitude toward drug addicts in a more positive way. It is also worth mentioning that there is a lack of information about the impact of stigma and discrimination on drug addiction and the factors that impede appropriate medical intervention. In developing future addiction prevention policies and plans, it is also important to consider how this information will be used in future data-driven planning, through assessing stigma and discriminatory attitudes toward addicts and obtaining feedback from patients.
Our study had some limitations. Although it is common to use cross-sectional analysis in public views toward drug addiction, it is difficult to derive cause-and-effect relationships from the present findings. We used a few simple questions when evaluating stigma and discrimination to be consistent with Barry et al. [22]; however, questions were not specific about the types of drugs (e.g., alcohol, smoking, or opioids) or standardized like the Devaluation-Discrimination Scale [55]. Therefore, this study cannot address differences in stigma or discrimination toward those addicted to alcohol versus those addicted to opioids. We also took cognizance of the limitation that the concepts of stigma and discrimination were not fully captured in the items used in present study. So it is unclear how clearly the participants understood and answered substance abuse, stigma, and discrimination.
Despite these limitations, this study went further than previous research and conducted a nationwide survey to understand the factors that affect stigma and discrimination in the general public in Korea. We suggested a better understanding of how individual and clinical characteristics may influence stigma and discrimination toward drug addiction, and emphasize the need to expand research to reduce stigma and discrimination. Further research is needed to better differentiate and address stigma and discrimination, especially as the need to explore factors that may directly or indirectly affect stigma as well as discrimination grows.
In conclusion, these findings suggest that a vast majority of Korean adults hold moderate levels of stigma and discrimination toward drug addiction. People who are women; over 40 years of age; with no history of opioid analgesic misuse; nonsmoking; agree to hospital treatment for addicts; and disagree to increase government support were more likely to stigmatize drug addicts. Meanwhile, those with higher incomes and are non-smoking were more likely to agree to discriminatory treatment for drug addicts. This study provides insight into factors influencing stigma and discrimination, hence it is essential to introduce drug addicts are guided to seek appropriate medical services and treatment institutions under positive social awareness and are encouraged to regain their health.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Ki Won Jang, Hae Kook Lee, Byung Joo Park, HoonChul Kang, Sang-Kyu Lee, Chan-Hyung Kim, Daeyoung Roh. Formal analysis: Hae Kook Lee. Methodology: Ki Won Jang, Hae Kook Lee. Project administration: Daeyoung Roh. Resources: Byung Joo Park, Hoon-Chul Kang, Sang-Kyu Lee, Chan-Hyung Kim. Software: Sang Kyu Nam. Supervision: Byung Joo Park, Hoon-Chul Kang, Chan-Hyung Kim, Daeyoung Roh. Validation: Sang-Kyu Lee. Visualization: Sang Kyu Nam. Writing—original draft: Ki Won Jang, Hae Kook Lee. Writing—review & editing: Ki Won Jang, Hae Kook Lee, Daeyoung Roh.
Funding Statement
This work was supported by the National Academy of Medicine of Korea, KYOBO Life, Life Insurance Social Contribution Committee (2020), a National Research Foundation of Korea (NRF) grant funded by the Korean government (NRF-2022R1A2C1005797), and R&D Program for Forest Science Technology (Project No. 2021390A00-2123-0105) provided by Korea Forest Service (Korea Forestry Promotion Institute).