|
 |
- Search
| Psychiatry Investig > Volume 20(7); 2023 > Article |
|
Abstract
Notes
Availability of Data and Material
Data sharing not applicable to this article as no datasets were generated or analyzed during the study.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Houman Sotoudeh. Data curation: all authors. Investigation: all authors. Methodology: all authors. Project administration: Mohammadreza Alizadeh. Supervision: Houman Sotoudeh. Validation: Houman Sotoudeh. Visualization: Houman Sotoudeh. Writing—original draft: all authors. Writing—review & editing: all authors.
Funding Statement
None
Figure 1.

Figure 2.
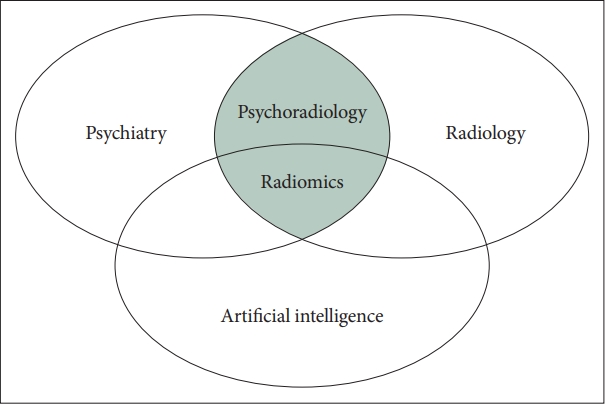
Table 1.
| Study | Target | Modality | No. of cases | Brain region segmented | No. of extracted features | Feature selection technique | No. of selected features | Machine learning models | Findings |
|---|---|---|---|---|---|---|---|---|---|
| Ma et al. [19] | Differentiation between major depression disorder (MDD) and subthreshold depression (STD) | T1 weighted MRI and DTI | 142 (43 MDD, 49 STD, 50 HC), only adolescent patients | 124 regions (38 cortical and subcortical regions and 24 sulci per hemisphere) | 3,030 | RF | 25 | RF | Accuracy 86% and AUC of 0.93 for MDD vs. HC |
| Accuracy 70.5%, AUC of 0.69 for STD vs. HC | |||||||||
| Accuracy of 59%, AUC of 0.66 for MDD vs. STD | |||||||||
| Zhang et al. [20] | Differentiate between isolated Parkinson’s disease (PD) from Parkinson’s disease with depression (PDP) versus healthy volunteers (HC) | Resting state fMRI | 21 DPD, 49 PD, 50 HC | 16 gyri | 6,557 | LASSO, RF, SVM | 19 features for PDP vs. HC, 34 features for PD vs. HC, 17 features for PD vs. PDP | LASSO, RF, SVM | LASSO had highest performance. |
| Accuracy of 95 for PDP vs. HC, 96% for PD vs. HC, and 85% for PD vs. PDP | |||||||||
| Lu et al. [21] | Differentiation between Schizophrenia (SZ) vs. HC | T1 MRI, [11c]ABP-688 PET | 17 SZ, 17 HC | 5 regions: frontal cortex, posterior cingulate, temporal cortex, primary auditory cortex, and thalamus | 48 | Relief Algorithm | Between 7 to 43 for different brain regions | SVM, Bagged Trees, KNN, NB | AUC of 0.89 for T1 sequence and 0.82 for PET to differentiate SZ vs. HC |
| Xi et al. [24] | Prediction of treatment response after ECT in SZ | T1 weighted MRI | 28 responsive and 29 non-responsive patients | 19 regions | 15 first order features | t-test | 13 | Logistic regression (LR), SVM | Accuracy above 90% for LR and SVM to predict treatment response |
| Park et al. [25] | Differentiation between SZ vs. HC | T1 weighted MRI | 86 SZ, 66 HC | Bilateral hippocampi | 642 | Mutual Formation | 30 | LR, Extra-trees, AdaBoost, XGBoost, SVM | LR had highest performance: Accuracy of 82% |
| SZ patients were on treatment | |||||||||
| Cui et al. [26] | Treatment (medical treatment, ECT, and rTMS) response prediction in SZ [treatment was heterogeneous, not all cases received the same treatment] | T1 weighted MRI and resting-state fMRI | 85 responsive and 63 non-responsive patients | 91 cortical and 15 subcortical regions | 408 | LASSO | 12 | SVM | Accuracy of 80% for fMRI, 69% for T1 and 85% for the combination of T1+fMRI |
| Latha and Kavitha [27] | Differentiation between SZ vs. Schizoaffective disorder (SA) vs. HC | T1 weighted MRI | 84 HC, 81 SZ, 31 SA | Ventricle, cerebellum, and whole brain | 104 feature for ventricles, 60 features for brain, 56 for cerebellum | No feature selection | Binary Particle Swarm Optimization, Fuzzy SVM | Features of cerebellum were more accurate with accuracy of 90% | |
| Wang et al. [28] | Differentiation between bipolar disorder II (BD II) vs. HC | Resting state fMRI | 90 BD (only BD II), 117 HC | 116 regions of brain | 7,018 | Mann-Whitney U-test and LASSO | 65 | SVM | Accuracy above 80% for HC vs. BD |
| Sun et al. [32] | Differentiation of ADHD from HC subjects, and Differentiation ADHD inattentive (ADHD-I) and combined inattentive and hyperactive subtypes (ADHD-C) | T1 weighted MRI and DTI | 83 (40 with ADHD-I and 43 with ADHD-C), and 87 HC | 31 cortical regions, 7 subcortical regions per hemisphere, 24 sulci per hemisphere, 48 white matter regions | 3,106 | Forest-based | 8 feature for ADHD vs. HC and 4 features for ADHS-I vs. ADHD-C | RF | Accuracy of 73% for ADHD vs. HC, 80% for ADHD-I vs. ADHD-C |
| Kim et al. [34] | Predicting the social anxiety | Resting state fMRI | 116 | 14 regions of brain | 56 | Shapley Additive Explanation | Features of orbitofrontal cortex | Xboost, SVM, RF, and multi-layer perceptron | Xboost with highest performance; accuracy of 77% |
| Bang et al. [38] | Differentiation of panic disorder vs. HC | T1 weighted MRI | 93 patients, 120 HC | Amygdala, insula, and anterior cingulate | 1,498 | LASSO | 179 | XGBoost, RF | AUC of 0.81 for differentiation panic patients vs. HC |
| Han et al. [39] | Differentiation between Internet gaming disorder (IGD) vs. HC | 3D Fast spoiled Gradient Recalled sequence, and DTI | 59 cases, 69 HC | 101 regions of brain | 2,084 | RF | 179 | RF | Accuracy of 73% to differentiate HC vs. IGD |
| Chaddad et al. [42] | Autism spectrum disorder (ASD) vs. development control | T1 | 34 cases, 30 HC | Hippocampi and amygdala | 15 | 11 features in hippocampi and 4 features for amygdala | SVM, RF | Accuracy of 76% to differentiate autism vs. HC |
MRI, magnetic resonance imaging; DTI, diffusion tensor imaging; AUC, area under the curve; fMRI, functional MRI; LASSO, least absolute shrinkage and selection operator; RF, random forest; SVM, support vector machine; PET, positron emission tomography; KNN, k-nearest neighbors algorithm; NB, Naive Bayes algorithm; rTMS, repetitive transcranial magnetic stimulation; ADHD, attention deficit hyperactivity disorder
REFERENCES