 |
 |
- Search
| Psychiatry Investig > Volume 19(5); 2022 > Article |
|
Abstract
Objective
Methods
Results
Notes
Availability of Data and Material
Data sharing not applicable to this article as no datasets were generated or analyzed during the study.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Se-Hoon Shim, Ji Sun Kim. Data curation: Ji Sun Kim. Formal analysis: Min Jin Jin. Funding acquisition: Se-Hoon Shim. Investigation: Ji Sun Kim. Methodology: Min Jin Jin. Project administration: Se-Hoon Shim, Ji Sun Kim. Resources: Se-Hoon Shim, Ji Sun Kim. Software: Ji Sun Kim, Min Jin Jin. Supervision: Se-Hoon Shim, Young Joon Kwon, Dongwook Lee, Ho Sung Lee. Validation: Se-Hoon Shim, Young Joon Kwon, Dongwook Lee, Ho Sung Lee, Ji Sun Kim, Min Jin Jin. Visualization: Min Jin Jin. Writing—original draft: Se-Hoon Shim. Writing—review & editing: Ji Sun Kim, Min Jin Jin.
Funding Statement
This work was supported by Jisan Cultural Psychiatry Research Fund and a grant (2020R1I1A3A04036435) awarded by the Basic Science Research Program through the National Research Foundation of Korea (NRF) and funded by the Ministry of Education. This study was also supported by Soonchunhyang University.
Figure 1.
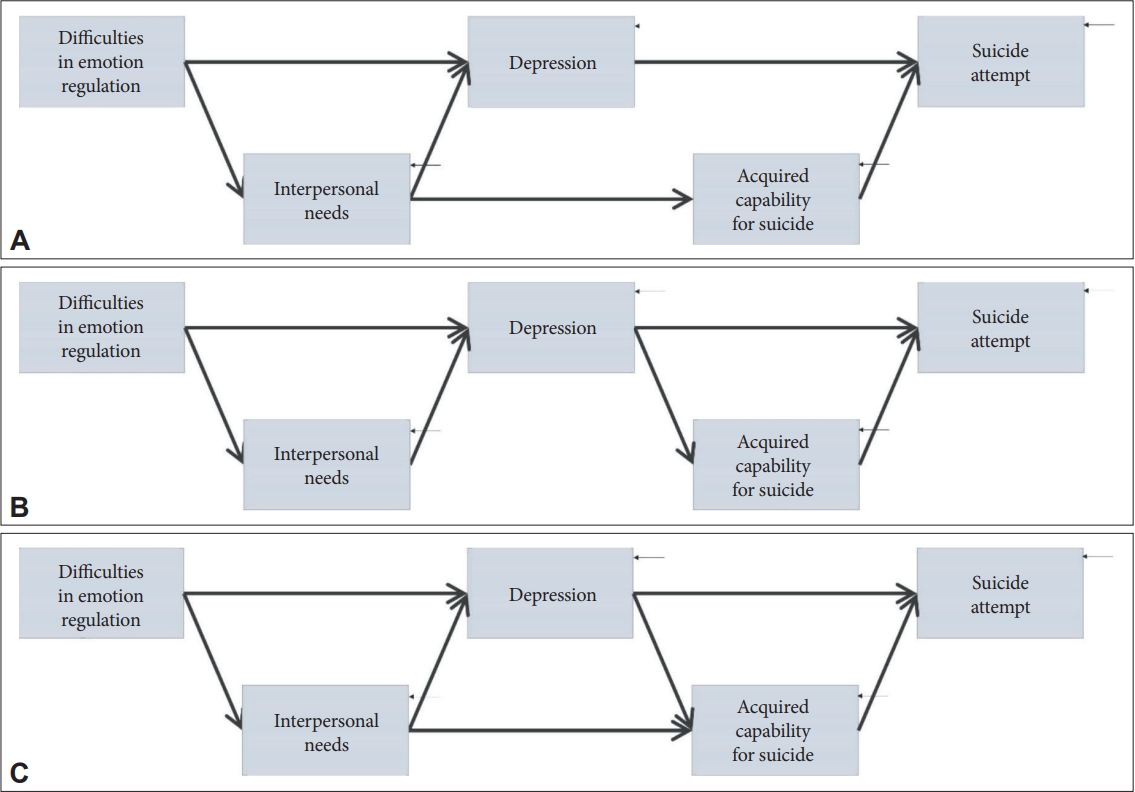
Figure 2.
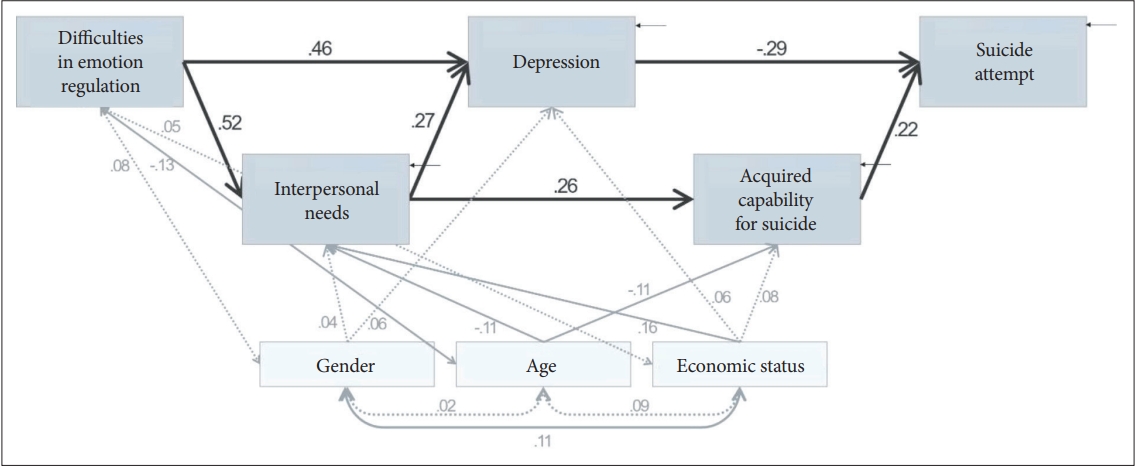
Figure 3.
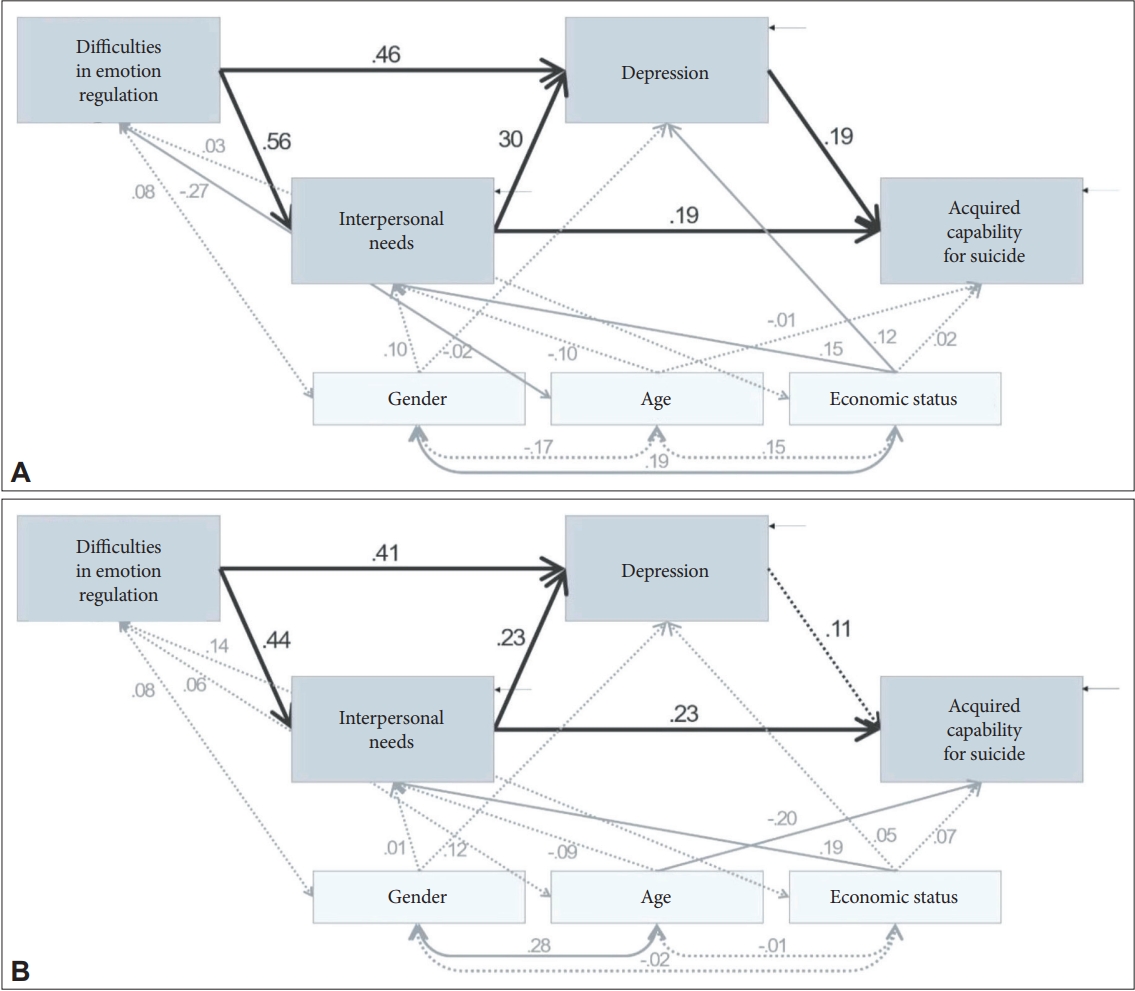
Table 1.
| Characteristic | Suicide attempters (N=197) | Suicide ideators (N=141) | Total (N=338) | t or χ2 |
|---|---|---|---|---|
| Age (yr) | 38.97±14.56 | 39.82±15.01 | 39.33±14.73 | -0.521 |
| Gender | ||||
| Men | 82 (41.6) | 56 (39.7) | 138 (40.8) | 0.124 |
| Women | 115 (58.4) | 85 (60.3) | 200 (59.2) | |
| Education (yr) | 12.62±9.34 | 12.19±3.52 | -0.524 | |
| Economic status | 6.191* | |||
| High | 5 (2.5) | 2 (1.4) | 7 (2.1) | |
| Middle | 126 (64.0) | 108 (76.6) | 234 (69.2) | |
| Low | 66 (33.5) | 31 (22.0) | 97 (28.7) | |
| Difficulties in Emotion Regulation Scale | 108.01±26.34 | 115.89±24.08 | 111.29±25.68 | -2.811† |
| Interpersonal Needs Questionnaire | 56.59±23.58 | 60.90±21.88 | 58.39±22.95 | -1.706 |
| Zung Self-Rating Depression Scale | 46.07±10.78 | 51.11±8.62 | 48.17±10.23 | -4.764‡ |
| Acquired Capability for Suicide Scale | 62.95±13.03 | 58.61±14.13 | 61.14±13.65 | 2.914† |
Table 2.
| Measures |
r |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
| 1. Gender | - | ||||||||
| 2. Age | 0.023 | - | |||||||
| 3. Education | -0.099 | -0.037 | - | ||||||
| 4. Economic status | 0.108* | 0.089 | -0.071 | - | |||||
| 5. Difficulties in Emotion Regulation Scale | 0.079 | -0.127* | -0.037 | 0.052 | - | ||||
| 6. Interpersonal Needs Questionnaire | 0.118* | -0.165† | 0.018 | 0.187† | 0.551‡ | - | |||
| 7. Zung Self-Rating Depression Scale | -0.061 | -0.146† | 0.028 | 0.122* | 0.199‡ | 0.290‡ | - | ||
| 8. Acquired Capability for Suicide Scale | 0.118* | -0.089 | -0.016 | 0.142† | 0.614‡ | 0.538‡ | 0.219‡ | - | |
| 9. Suicide attempt or ideation | -0.019 | -0.028 | 0.055 | 0.105 | -0.152† | -0.089 | 0.157† | -0.243‡ | - |
Table 3.
| Model | χ2 | df | p | CFI | NFI | TLI | RMSEA | AIC |
|---|---|---|---|---|---|---|---|---|
| Hypothesized model | 12.557 | 9 | 0.184 | 0.991 | 0.971 | 0.973 | 0.034 | 66.557 |
| Alternative model 1 | 21.952 | 9 | 0.009 | 0.969 | 0.950 | 0.902 | 0.065 | 75.952 |
Table 4.
| Variable | Standardized regression weights | SE | CR |
|---|---|---|---|
| DERS → INQ | 0.523‡ | 0.040 | 11.698 |
| DERS → SDS | 0.460‡ | 0.019 | 9.394 |
| INQ → SDS | 0.268‡ | 0.022 | 5.376 |
| INQ → ACSS | 0.256‡ | 0.032 | 4.783 |
| SDS → Suicide attempt or ideation | -0.290‡ | 0.003 | -5.585 |
| ACSS → Suicide attempt or ideation | 0.220‡ | 0.002 | 4.233 |
| Gender → INQ | 0.062 | 2.075 | 1.388 |
| Gender → SDS | 0.043 | 0.856 | 1.052 |
| Age → INQ | -0.115* | 0.070 | -2.563 |
| Age → ACSS | -0.112* | 0.049 | -2.118 |
| Economic status → INQ | 0.164‡ | 2.100 | 6.667 |
| Economic status → SDS | 0.063 | 0.876 | 1.514 |
| Economic status → ACSS | 0.084 | 1.484 | 1.594 |
| Gender ↔ Age | 0.023 | 0.394 | 0.430 |
| Gender ↔ Economic status | 0.108* | 0.013 | 1.974 |
| Gender ↔ DERS | 0.079 | 0.689 | 1.450 |
| Age ↔ Economic status | 0.089 | 0.391 | 1.621 |
| Age ↔ DERS | -0.127* | 20.711 | -2.311 |
| Economic status ↔ DERS | 0.052 | 0.681 | 0.955 |
Table 5.
| Variable |
Suicide attempts |
Suicide ideators |
||||
|---|---|---|---|---|---|---|
| Standardized regression weights | SE | CR | Standardized regression weights | SE | CR | |
| DERS → INQ | 0.558‡ | 0.051 | 9.701 | 0.439‡ | 0.067 | 5.933 |
| DERS → SDS | 0.461‡ | 0.026 | 7.226 | 0.409‡ | 0.028 | 5.270 |
| INQ → SDS | 0.298‡ | 0.030 | 4.560 | 0.231† | 0.031 | 2.917 |
| INQ → ACSS | 0.192* | 0.047 | 2.267 | 0.232† | 0.057 | 2.620 |
| SDS → ACSS | 0.189* | 0.101 | 2.260 | 0.114 | 0.142 | 1.310 |
| Gender → INQ | 0.105 | 2.742 | 1.820 | -0.004 | 3.392 | -0.050 |
| Gender → SDS | -0.016 | 1.148 | -0.296 | 0.118 | 1.209 | 1.708 |
| Age → INQ | -0.100 | 0.096 | -1.692 | -0.085 | 0.111 | -1.232 |
| Age → ACSS | -0.013 | 0.063 | -0.190 | -0.198* | 0.074 | -2.532 |
| Economic status → INQ | 0.147* | 2.627 | 2.553 | 0.194† | 3.677 | 2.628 |
| Economic status → SDS | 0.120* | 1.098 | 2.283 | 0.046 | 1.393 | 0.646 |
| Economic status → ACSS | 0.015 | 1.765 | 0.217 | 0.074 | 2.598 | 0.916 |
| Gender ↔ Age | -0.167* | 0.518 | -2.312 | 0.283† | 0.643 | 3.222 |
| Gender ↔ Economic status | 0.188* | 0.018 | 2.587 | -0.016 | 0.018 | -0.189 |
| Gender ↔ DERS | 0.078 | 0.928 | 1.091 | 0.076 | 0.995 | 0.895 |
| Age ↔ Economic status | 0.155* | 0.540 | 2.140 | -0.006 | 0.554 | -0.075 |
| Age ↔ DERS | -0.265‡ | 28.184 | -3.590 | 0.063 | 30.396 | 0.748 |
| Economic status ↔ DERS | 0.028 | 0.965 | 0.393 | 0.143 | 0.897 | 1.678 |
REFERENCES







