The Severity of Sleep Disordered Breathing Induces Different Decrease in the Oxygen Saturation During Rapid Eye Movement and Non-Rapid Eye Movement Sleep
Article information
Abstract
Objective
To investigate how differences in oxygen saturation between non-REM (NREM) and REM sleep in patients according to the severity of sleep apnea.
Methods
We studied 396 male patients diagnosed with simple snoring or obstructive sleep apnea syndrome (OSAS) on nocturnal polysomnography. Patients were divided into groups by the OSAS severity. We compared the average oxygen saturation between REM and NREM sleep in each group.
Results
In the simple snoring group, average oxygen saturation was significantly greater during REM than during NREM sleep. In the severe OSA group alone, average oxygen saturation was greater in NREM than in REM sleep. The difference of NREM-REM average oxygen saturation correlated significantly with AHI in the severe OSA group.
Conclusion
More severe hypoxemia was seen in REM than NREM sleep in the severe OSAS group. The differential oxygen decrease between REM and NREM sleep is likely due to the differentially occurring sleep breathing events in each sleep stage according to the SDB severity. The more AHI increases in the severe OSAS patients, the more prominent the hypoxemia of REM sleep compared with NREM sleep is likely to appear. This suggests that the pressure of continuous positive airway pressure should be increased to control the hypoxemia of REM sleep in extremely severe OSAS.
INTRODUCTION
There is a difference between the breathing pattern while awake and asleep. While awake, intentional breathing control takes priority over automatic breathing; in contrast, this changes after falling asleep. When sleeping, breathing changes in accordance with the stage of sleep.1 The fact that patients with obstructive sleep apnea have apnea and patients with chronic pulmonary disease have hypoxia is related to these changes. That is, while awake, the system that controls breathing operates effectively. In contrast, during sleep, the breathing control system becomes relatively unstable, and interacts with collapsing forces that affect characteristic anatomic structures, such as the pharyngeal airway, weakened reactions of the muscles of the upper airway, and arousal threshold. This leads to, and affects the severity of, sleep apnea.2
Sleeping is categorized into two main phases: rapid eye movement (REM) and non-rapid eye movement (NREM) sleep. During REM sleep, breathing is irregular, with shallow amplitude, and low frequency. Hypoxemia, often due to hypoventilation, is often observed in comparison with NREM sleep. That is, during REM sleep, the oxygen saturation is generally lower than that during NREM sleep. In comparison with being awake, during REM sleep, arterial oxygen saturation is lowered; when hypoventilation occurs, arterial oxygen saturation decreases further.34
The mechanism of this phenomenon has not yet been revealed, but it may be due to the fact that during REM sleep the tension of muscles that expand the thoracic cavity is relatively decreased, but the resistance of the upper airway is increased, weakening ventilation.5
During REM sleep, there is a decrease in the muscular strength of the intercostal and other breathing-related muscles, except for the diaphragm. During NREM sleep, sound pressure reflections gradually decreases, and further decrease during REM sleep.16 Hypoxia, due to apnea during REM sleep, may be closely related to the aftereffects and dysfunctions of sleep apnea such as daytime sedation and cognitive impairment. In this regard, it is of particular clinical importance.7
It is known that when the ventilatory response to hypoxemia decreases during sleep, it differs by sex.8 In the case of both men and women, the ventilatory response to hypoxemia decreases more during REM than NREM sleep, during which there is no significant difference between sexes.9 However, in a study which examined only male patients, the ventilatory response decreases more during NREM sleep in comparison with the awakened state. In another study, which examined female patients only, the level of ventilatory response during NREM sleep was similar to that of being awake.10
As such, it is widely known that, in the case of normal adults, the ventilatory response to hypoxemia is weakened during sleep, and is closely related to several clinical sequelae of Obstructive Sleep Apnea (OSA). However, the relationship between oxygen saturation and the severity of sleep apnea during REM and NREM sleep has not yet been clarified. Hence, this study investigated how oxygen saturation differs during REM and NREM sleep, in accordance with the severity of sleep apnea, as well as related main factors such as age, body mass index, and hypertension.
METHODS
Subjects
We recruited 396 untreated male patients with simple snoring or obstructive sleep apnea syndrome (OSAS), who had undergone nocturnal polysomnography. Mean±SD age was 40.8±12.0 years and average body mass index (BMI) was 26.7±3.5 kg/m2. Subjects were categorized into four groups, simple snoring (n=37), mild OSAS (n=92), moderate OSAS (n=103), and severe OSAS (n=164).
Mild OSAS was defined as apnea-hypopnea index (AHI) greater than or equal to 5 but less than 15, moderate OSAS was defined as AHI greater than 15 and less than or equal to 30, and severe OSAS as AHI greater than 30. All subjects met the following inclusion criteria: 1) male, 2) REM sleep time greater than thirty minutes, total sleep time greater than one hundred and eighty minutes, 3) normal electrocardiogram at wakefulness, 4) apnea-hypopnea index (AHI) greater than 5 in OSAS subjects, and 5) no medication except antihypertensive medication.
Exclusion criteria included previous or current cardiovascular disease, pulmonary disorder, diabetes mellitus, substance abuse, history of taking alcohol or other drugs up to 7 days before polysomnographic study, previous diagnosis of sleep disorder except for simple snoring or OSAS, disorders of the autonomic nervous system or endocrine system that can change blood pressure, and a history of surgery or continuous positive airway pressure (CPAP) treatment for OSAS. Informed consent was obtained prior to the study. The protocol was approved by the institutional review board.
Methods
Nocturnal polysomnography
Polysomnographic recordings were performed with the Embla N7000 system (Medcare-Embla, Reykjavik, Iceland) using Somnologica version 3.3.1 software (Medcare-Embla, Reykjavik, Iceland) during the time when the subjects were in bed from light-off to light-on. Electroencephalography was monitored using two pairs of C3/A2 and C4/A1 leads and O1/A2 and O2/A1 leads. Two pairs of electro-oculographic leads were also used. Electromyographic leads were placed on the submentalis and tibialis anterior muscles. Airflow was continuously measured by a thermistor and a nasal pressure cannula. Respiratory movements were monitored using respiratory inductive plethysmographic belts around the chest and abdomen. Oxygen saturation was measured using a pulse oximeter that was put on the left second finger. Average oxygen saturation (%), lowest oxygen saturation (%), time of oxygen saturation <90% (min), time of oxygen saturation <80% (min), and time of oxygen saturation <70% (min) were measured. Many variables related to sleep structure, such as time in bed (TIB), total sleep time (TST), sleep period time (SPT), sleep latency (SL), sleep efficiency (SE), stage 1 sleep (S1), stage 2 sleep (S2), slow wave sleep (SWS), REM sleep, wake, slow wave sleep fraction and arousal index, were calculated. The oxygen desaturation event index (ODI) was defined as the number of events per hour in which oxygen saturation decreased by 4% or more. Hypopnea was defined as a reduction of airflow by 50–80% for at least 10 sec associated with either oxygen desaturation of at least 4% or arousal. Apnea was defined as an air flow reduction of 90% or more for at least 10 sec. AHI was calculated by dividing the total number of apneas and hypopneas by the number of hours of sleep. The evaluation of sleep stages and events was based on the American Academy of Sleep Medicine (AASM) manual.11
Statistical analysis
This study utilized SPSS (SPSS Windows, 17.0, SPSS Inc., Chicago, IL, USA) to analyze data. In order to investigate whether the average oxygen saturation differed in accordance with the severity of sleep apnea, the subjects were categorized into four groups: simple snoring, and mild, moderate, and severe obstructive sleep apnea. The independent samples t-test was conducted for each group. We analyzed the correlations between the difference of average oxygen saturation during NREM and REM sleep, and demographic variables, AHI, antihypertensive medication therapy, and other variables related to sleep and oxygen saturation. Statistical significance was set as p<0.05. In addition, subjects with severe sleep apnea were categorized into two groups: a group showing higher average oxygen saturation during REM than during NREM sleep, and another group showing higher average oxygen saturation during NREM sleep, for which the independent samples t-test was conducted.
RESULTS
Demographic and sleep parameter data
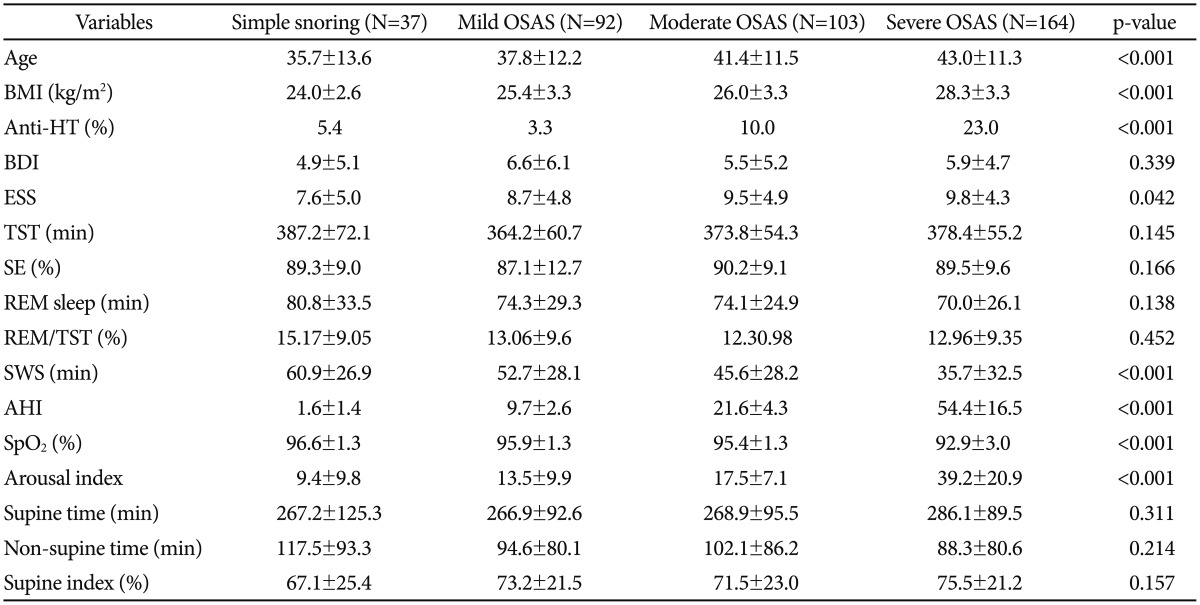
The subjects were categorized into simple snoring (n=37, 35.7±13.6 years), mild OSAS (n=92, 37.8±12.2 years), moderate OSAS (n=103, 41.4±11.5 years), and severe OSAS (n=164, 43.0±11.3 years). When the groups were compared in terms of demographic variables and sleep related indicators based upon polysomnography results, there were significant differences in age, BMI, whether taking antihypertensive medication, oxygen saturation, and arousal index (p<0.001). There were no differences in other demographic variables and the sleep related indicators based on polysomnography (Table 1).
Average oxygen saturation in REM and NREM sleep
By group, the average oxygen saturation of the simple snoring group was statistically significantly higher during REM than NREM sleep (REM vs. NREM; 96.91±0.20 vs. 95.55±0.22; p<0.001). Patients with mild and moderate sleep apnea showed no significant difference in oxygen saturation between REM and NREM sleep. The oxygen saturation of patients with severe sleep apnea was higher during NREM than REM sleep(REM vs. NREM; 91.79±0.37 vs. 93.15±0.22; p<0.001) (Table 2).
Correlation between oxygen saturation difference during NREM-REM and other variables in patients with severe sleep apnea
In patients with severe sleep apnea, in order to find potential correlates with the difference in average oxygen saturation between NREM and REM sleep, correlation with age, body mass index, sleep apnea-hypopnea index (AHI), mean oxygen saturation, and lowest oxygen saturation was analyzed. Consequently, there was significant positive correlation with BMI (r=0.312; p<0.001), AHI (r=0.322; p<0.001), mean oxygen saturation (r=0.452; p<0.001), and number of awakenings (r=0.349; p<0.001). It showed significant negative correlation with the lowest oxygen saturation (r=-0.668; p<0.001) and mean oxygen saturation (r=-0.552; p<0.001).
In particular, severe sleep apnea was strongly associated with BMI, so when it was controlled for, partial correlation analysis showed that the difference between the average oxygen saturations of NREM and REM sleep appeared to have a positive correlation with the degree of arousal (rp=0.286, p<0.001), supine index (rp=0.200; p<0.05) and AHI (rp=0.229; p<0.001) (Table 3). In patients with severe sleep apnea, when BMI was controlled for, there was a significant correlation between the difference in oxygen saturation between NREM and REM sleep, and the AHI indices (Figure 1).
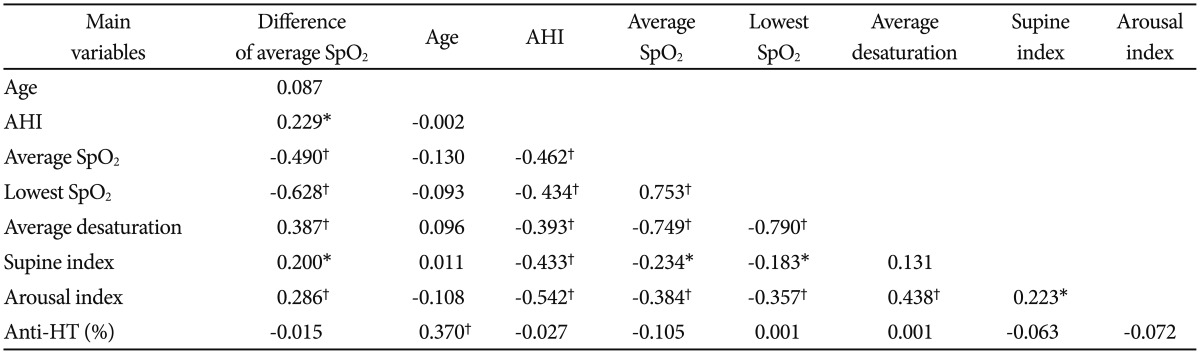
The difference of NREM-REM average oxygen saturation correlation with AHI, supine position time, and oxygen variables adjusted by BMI in severe obstructive sleep apnea syndrome group

The correlation between apnea-hypopnea index and the difference in the average oxygen saturations during rapid eye movement and non-rapid eye movement sleep, when controlled for body mass index, in the severe obstructive sleep apnea group (rp=0.229, p<0.05). N-REM: non-rapid eye movement, REM: rapid eye movement.
Comparison based on differences in oxygen saturation of patients with severe obstructive sleep apnea
We categorized 164 patients with severe obstructive sleep apnea into two groups, and then compared the groups. In Group A (n=108, 44.39±10.84 years), the average oxygen saturation, which was lower during REM than NREM sleep, was compared with Group B (n=56, 39.96±11.65 years) average oxygen saturation, which was lower during NREM than REM sleep. As a result, age (44.39±10.84 vs. 39.96±11.65, p=0.018) and AHI (57.34±16.99 vs. 49.97±15.29, p=0.004) were significantly higher in Group A. Group A's average oxygen saturation (92.21±3.38 vs. 93.98±1.81, p<0.001) and lowest oxygen saturation (72.76±8.34 vs.79.63±5.47, p<0.001) were significantly lower. In terms of the duration of oxygen saturation less than or equal to 90% (81.20±77.20 vs. 41.88±40.85, p<0.001), and oxygen saturation was less than or equal to 80% (16.52±36.44 vs. 3.11±9.51, p=0.001), it was significantly longer in Group A (Table 4). In Group A, after controlling for BMI, there was an interdependence between AHI indices and differences in oxygen saturation during NREM and REM sleep (rp=0.336, p<0.001). In Group B, there was no interdependence (rp=-0.241, p=0.074) (Figure 2).

Comparison of subgroups according to average oxygen saturation in the severe obstructive sleep apnea syndrome group
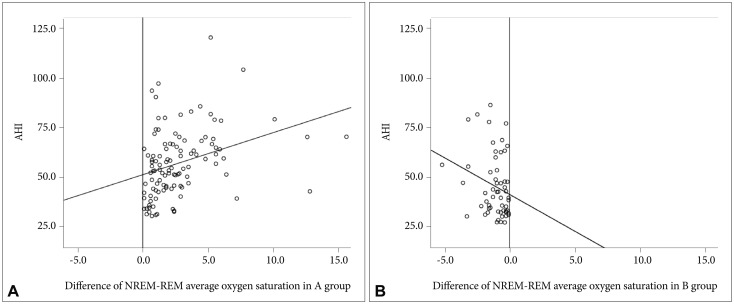
A: The correlation between apnea-hypopnea index and the difference of non-rapid eye movement-rapid eye movement average oxygen saturation controlling for age and body mass index is shown by a positive correlation (rp=0.336, p<0.001) in patients with severe obstructive sleep apnea syndrome in group A. B: The correlation between apnea-hypopnea index and the difference of non-rapid eye movement-rapid eye movement average oxygen saturation controlling for age and body mass index is not shown by a significant correlation (rp=-0.241, p=0.074) in patients with severe obstructive sleep apnea syndrome in group B. A group: average saturation (%) of NREM >average saturation (%) of REM, B group: average saturation (%) of REM >average saturation (%) of REM. REM: rapid eye movement.
DISCUSSION
In this study, it was confirmed that selective difference in average oxygen saturation during NREM and REM sleep occurred according to the severity of sleep breathing disorder (SBD). In the case of simple snoring, the average oxygen saturation during REM was statistically significantly higher. Patients with mild and moderate OSAS showed no significant difference in oxygen saturation during REM and NREM sleep. In the case of patients with severe OSAS, the average oxygen saturation was lower during REM than NREM sleep. Previous studies reported that apnea or hypopnea can be further exacerbated during REM sleep, as compared to NREM sleep1213 and that average oxygen saturation was lower during REM sleep, as compared to NREM sleep.14 However, because these previous studies were conducted on patients with REM-dependent obstructive sleep apnea with relatively lower AHI and milder severity of apnea than patients with non-REM-dependent obstructive sleep apnea, the results are expected to be inconsistent with the finding in this study, which examined patients with various severities of SBD.1516
To our knowledge, there have not been any studies that investigated the reason why average oxygen saturation differs during REM and NREM sleep in accordance with SBD. We hypothesized that the distribution of events of sleep apnea may differ in accordance with the severity of SBD. In the case of simple snoring, sleep apnea or snoring are more likely to happen during NREM than REM sleep. In cases of mild and moderate obstructive sleep apnea, they happen regardless of REM and NREM sleep, and in cases of severe obstructive sleep apnea, sleep apnea happens more intensely during REM than NREM sleep.
It has been reported that there is no correlation between the severity of obstructive sleep apnea and sleep stage,17 but there have been reported results where AHI-NREM was far higher than AHI-REM in the cases of patients with severe obstructive sleep apnea.121518 However, some have argued that AHI during REM sleep can be relatively undervalued, considering the fact that the ratio of REM sleep to total sleeping time is decreased when sleep apnea is more severe.19 In this regard, further comparative study is required, measuring AHIs in REM and NREM sleep and compensating for total sleeping time.
As a result of the analysis of the correlation between the difference in average oxygen saturation between NREM and REM sleep, and age, supine figure, the non-supine Index, and variables related to oxygen, it was found that there was no statistically significant correlation between the difference in oxygen saturation, and age or hypertension. However, AHI did demonstrate a significant correlation with the difference in average oxygen saturation. The fact that in cases of severe obstructive sleep apnea, the difference in average oxygen saturation between NREM and REM sleep correlated with AHI, may partially explain why Continuous Positive Airway Pressure (CPAP) is increased, which is due to the high possibility of severe hypoxia during REM sleep.20
It is known that patients with positional obstructive sleep apnea with sleeping time longer than or equal to 15 minutes and AHI higher than or equal to 5, supine AHI is at least twice non-supine AHI and have lower rates of obesity than patients with non-positional obstructive sleep apnea. They are also known to have mild and moderate symptoms of obstructive sleep apnea.21 Previous research showed that non-supine position has no clear correlation with severity of obstructive sleep apnea.22 However, this study showed that in the case of patients with severe sleep apnea, AHI and supine index showed correlation (rp=0.433, p<0.001).
When the patients with severe OSA are compared, having been categorized into a group with low average oxygen saturation during REM sleep and another group with low average oxygen saturation during NREM sleep, the group with low oxygen saturation during REM sleep showed higher AHI, age, and BMI than its counterparts. Its average oxygen saturation and lowest oxygen saturation was lower, and the duration of oxygen saturation less than or equal to 90% or 80% was relatively longer. Like previous research, in this study, the apnea period was estimated to be longer during REM than NREM sleep.2324 This is because the degree of arousal is lower during REM than NREM sleep.25 Accordingly, it could be deduced that the hypoxic period can lengthen when the sleep apnea index is higher, which makes sleep apnea more severe during REM sleep. In this regard, the cases of patients whose oxygen saturation is obviously lower during REM sleep required more proactive treatment.
This study has a limitation that the AHI of REM and NREM sleep were not separately analyzed. In night polysomnography, normally sleep apnea is evenly observed throughout REM and NREM sleep. However, in the case of certain patients, apnea occurs more during REM sleep. In particular, when sleep apnea happens more during REM sleep, AHI during REM sleep is typically at least twice that during NREM sleep, and is referred to as REM Sleep-Dependent Obstructive Sleep Apnea, which was not analyzed in this study. However, it is known that patients with REM Sleep-Dependent Obstructive Sleep Apnea tend to be relatively young female patients with mild OSA.2627 In order to resolve this limitation, this study examined only male subjects, but for more precise evaluation, in further studies that separate REM and NREM sleep, the AHI for each phase needs to be analyzed.
This study, for the first time, suggests that oxygen saturation of REM and NREM sleep can differ in accordance with the severity of sleep disordered breathing. This study also suggests that, in the case of patients whose hypoxia becomes severe during REM sleep, continuous positive airway pressure (CPAP) needs to be more actively controlled to resolve hypoxia, as well as oxygen saturation during NREM and REM sleep.
Acknowledgments
This paper was supported financially by Konkuk University (Seoul, Korea) in 2015. The financial sponsors played no role in the design, execution, analysis and interpretation of data or writing of the study.