Borderline Personality Pathology in Major Depressive Disorder, Bipolar I and II Disorder, and Its Relationship With Childhood Trauma
Article information
Abstract
Objective
Mood disorder and borderline personality pathology (BPP) are frequently comorbid and relate to childhood trauma. We investigated the relationship between childhood trauma and BPP features in mood disorder patients versus controls.
Methods
A total of 488 mood disorder patients, particularly major depressive disorder (MDD), bipolar I disorder (BD I), and bipolar II disorder (BD II), and 734 controls were included. We examined between-group BPP-related differences and correlated between BPP and childhood trauma using the Childhood Trauma Questionnaire-Short Form (CTQ) and the Personality Assessment Inventory–Borderline Features Scale.
Results
BD II patients showed significantly higher BPP. Emotional abuse and neglect were prominently associated with BPP, while affective instability and negative relationships exhibited a stronger association with childhood trauma. We also found a positive relationship between childhood trauma and BPP in MDD, BD I, and BD II patients.
Conclusion
The findings of the present study imply that BPP features are more likely to be found in patients with BD II than BD I or MDD. Mood disorder patients with severe childhood trauma may have higher BPP features. Thus, further study of the relationship between childhood trauma and BPP features could improve the therapeutic approaches and help understand patients with mood disorders.
INTRODUCTION
Mood disorders are common mental diseases affecting the general population [1]. Patients with mood disorders frequently have high rates of borderline personality pathology (BPP) [2-6]. Mood disorder patients with BPP demonstrate a high risk for treatment resistance, self-harm, and suicide attempts [7-9]. These findings suggest that the consideration of borderline personality features in mood disorders is clinically important.
BPP is a characteristic that accounts for borderline personality disorder [10]. BPP comprises four critical features [11,12]: 1) affective instability: extreme emotional response, quick and severe mood fluctuation, and uncontrolled anger; 2) identity problem: losing a sense of purpose, emptiness, boringness, and unsatisfied feelings about one’s life; 3) negative interpersonal relationships: feelings of hostility or betrayal by close friends and experiencing unstable or intense emotions in relationships; and 4) self-harm: an impulsive tendency leading to negative effects on one’s person. The features of BPP and bipolar disorder (BD) found similar characteristics [13], leading misdiagnosing to as mood disorders or personality disorders [14]. Another study showed that mood disorder patients, MDD and BD, with features of BPP increased suicide risk [15]. These findings suggest that studying BPP in the context of various mood disorders (e.g., MDD, bipolar I disorder [BD I], and bipolar II disorder [BD II]) is worthwhile.
Childhood trauma is defined as any abuse or neglect that leads to emotional, sexual, and physical harm to a child [16]; it affects the development of emotion, behavior, social life, physical development, and cognition [17-19] during childhood and throughout life [20]. Various studies [21-23] revealed that negative experiences from childhood maltreatment are closely related to BPP, particularly physical or sexual abuse and neglect [24]. Physical and sexual abuse were significantly related to the increased risk for mood disorder [25]; thus, it is necessary to examine childhood trauma correlating to mood disorder subtypes. Previous studies showed that childhood trauma could significantly impact the clinical course of mood disorders, even though each diagnosis has different associations. Emotional trauma, for example, predicted psychotic symptoms in patients with BD [26] and was associated with somatization in MDD [27]. There have been limited studies on the relationship between childhood trauma and BPP in mood disorder patients. These findings imply that investigating this relationship is important.
In the present study, we investigated the relationship between various types of childhood trauma and features of BPP in patients with diagnosed mood disorders (MDD, BD I, or BD II) in comparison to control groups. We hypothesized that: 1) features of BPP would differ between groups (MDD, BD I, BD II, and comparison group); 2) childhood trauma would be significantly associated with BPP, and its association would vary depending on the features of BPP and on the type of childhood trauma.
METHODS
Participants
The present study is cross-sectional research at the Seoul National University Bundang Hospital (SNUBH) from September 2019 to February 2021. All patients were diagnosed with a mood disorder, particularly MDD, BD I, and BD II, based on the Diagnostic Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) [28] criteria and received treatment at the mood disorder clinic of the SNUBH. The diagnoses were confirmed by board-certified psychiatrists (T.H.H and W.M) based on a structured diagnostic interview (Mini-International Neuropsychiatric Interview [M.I.N.I]) [29] or review of case records. All information related to patients, including sex, education, job, marital status, smoking, drinking, psychiatric family history, and hospitalization history, was gathered. The Participants as the comparison group were recruited anonymously and excluded by self-reported a history of psychiatry disorder. 488 patients with mood disorders (MDD [n=130], BD I [n=79], and BD II [n=279]) and 734 individuals from the general population were analyzed in the study. As all patient data were collected from medical chart review and comparison data were collected through anonymous surveys without direct access to personal information from the researchers, informed consent was waived. The present study protocol was approved by the Institutional Review Board of Seoul National University Bundang Hospital (B-2104-679-103).
Clinical instruments
Personality Assessment Inventory–Borderline Features Scale
The Personality Assessment Inventory–Borderline Features Scale (PAI-BOR) [12] is a self-report scale that clinically assesses borderline personality features in 24 items. The items are classified into four subscales: affective instability, identity problems, negative relationships, and self-harm. The scale is rated on a four-point Likert-type scale and ranges from 0 to 3 (0=false/not at all true, 1=slightly true, 2=mainly true, and 3=very true). A total raw score of ≥38 indicates the existence of BPD features, and a score of ≥60 demonstrates conventional borderline personality functioning.
Childhood Trauma Questionnaire-Short Form
The Childhood Trauma Questionnaire-Short Form (CTQ) [30] is a retrospective self-reporting scale that asks questions about childhood and adolescence experiences (under the age of 18) through 28 items rated on a five-point Likert scale with scores ranging from 1 to 5 (1=never true, 2=rarely true, 3=sometimes true, 4=often true, and 5=very often true). These items are divided into five trauma subtypes: Emotional abuse, physical abuse, sexual abuse, emotional neglect, and physical neglect. We used a modified CTQ score for this study after excluding minimization/denial scores (items 10, 16, 22), with scores ranging from 25–125, and each subscale having potential scores ranging from 5–25.
Statistical analysis
Differences between groups regarding demographic and clinical variables were analyzed via the independent samples t-test for continuous variables, such as age. Categorical variables were compared using the chi-square test. Analysis of covariance (ANCOVA) was conducted to compare the patient and comparison group PAI-BOR and CTQ scores, followed by post-hoc testing with Bonferroni correction to ascertain the direction of differences. A partial correlation coefficient was obtained from the residuals of multiple regression to examine the correlation between PAI-BOR and CTQ scores, controlling for potential confounding factors (age, sex, education, employment, marital status, psychiatric first-degree family history, alcohol use status, and smoking status). All statistical analyses were two-tailed, with the statistical significance level set at p<0.05. Bonferroni’s correction was applied to correct for type I errors from multiple tests, multiplying the unadjusted p-value by the total number of tests. All analyses were performed using R, version 4.0.5 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
Clinical and demographic characteristics
Data from 488 psychiatric patients (MDD [n=130], BD I [n=79], and BD II [n=279]) and 734 individuals from the general population were analyzed in the study. Clinical and demographic characteristics are presented in Table 1. Participants were aged 16–67 years, with a mean age of 36.60 (standard deviation [SD]=11.64). There were 503 males (41.2%) and 719 females (58.8%) participants in total, with 158 males (32.4%) and 330 females (67.4%) in the patient group, and 345 males (47.0%) and 389 females (53.0%) in the comparison group. There were statistical differences between the patient and comparison group regarding age (t=6.43, p<0.001), sex (χ2(1)=25.89, p<0.001), education (χ2(1)=72.92, p<0.001), employment status (χ2(1)=129.75, p<0.001), marital status (χ2(1)=37.14, p<0.001), psychiatric family history (χ2(1)=63.50, p<0.001), and alcohol use status (χ2(1)=66.64, p<0.001).
Scores of Personality Assessment Inventory–Borderline Features Scale and Childhood Trauma Questionnaire-Short Form according to groups
There were significant group differences regarding PAI-BOR total score (F3,1218=43.07, p<0.001) (Figure 1 and Supplementary Table 1 in the online-only Data Supplement). BD II patients in particular, had significantly higher PAI-BOR total scores (mean±SD, 35.38±12.58) compared to those of the comparison group (23.06±10.28, p<0.001), MDD (26.71±10.40, p<0.001) and BD I patients (27.91±13.60, p<0.001). Among the subscales, the scores for affective instability and identity problems in BD II patients were significantly higher than those from all other groups. BD II patients also had significantly higher scores for negative relationships and self-harm compared to the MDD and comparison groups (all corrected p<0.001). MDD patients had significantly higher scores than those of the comparison group regarding total score (p<0.01) and affective instability (p<0.001). BD I patients had a significantly higher score than those of the comparison group for self-harm (p<0.01). We also found multiple differences in CTQ total scores and subscales in the ANCOVA with Bonferroni post-hoc comparisons (Supplementary Table 1 in the online-only Data Supplement).
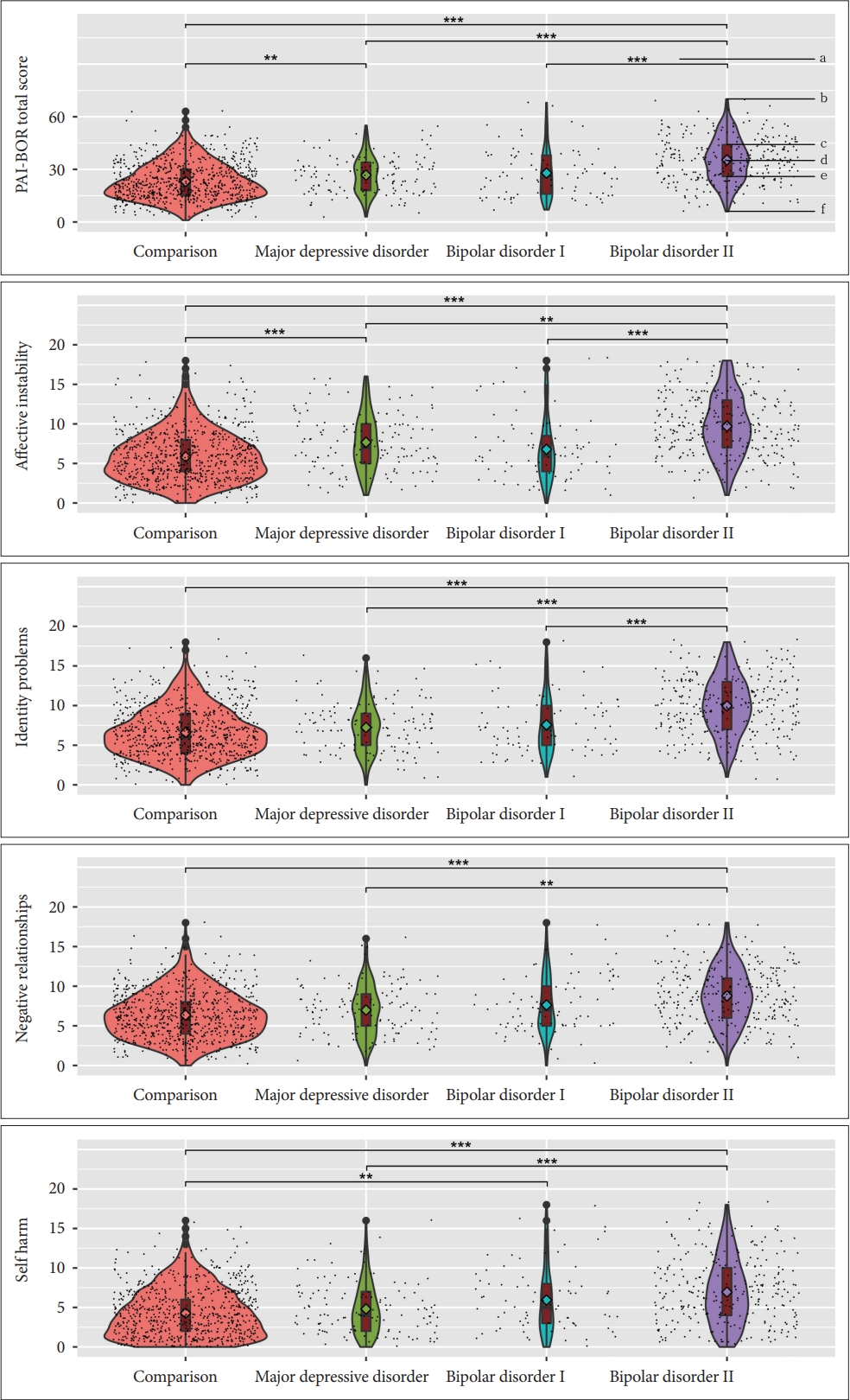
Violin plots for distribution of borderline personality disorder scale (PAI-BOR), according to the groups. a: p-value of Kruskal–Wallis analysis. b: Upper adjacent value. c: Third quartile (75%ile). d: Median. e: First quartile (25%ile). f: Lower adjacent value. **p<0.01; ***p<0.001. PAI-BOR, Personality Assessment Inventory–Borderline Features Scale.
Relationship between Childhood Trauma and Borderline Personality Features
Partial correlation analyses showed that CTQ total score was positively correlated with PAI-BOR total score (r=0.406, p<0.001 in all participants; r=0.419, corrected p<0.001 in the comparison group; r=0.335, corrected p<0.001 in all patients) (Figure 2A-C, Supplementary Tables 2-4 in the online-only Data Supplement) These findings showed that individuals with high scores for childhood trauma showed high levels of BPP.
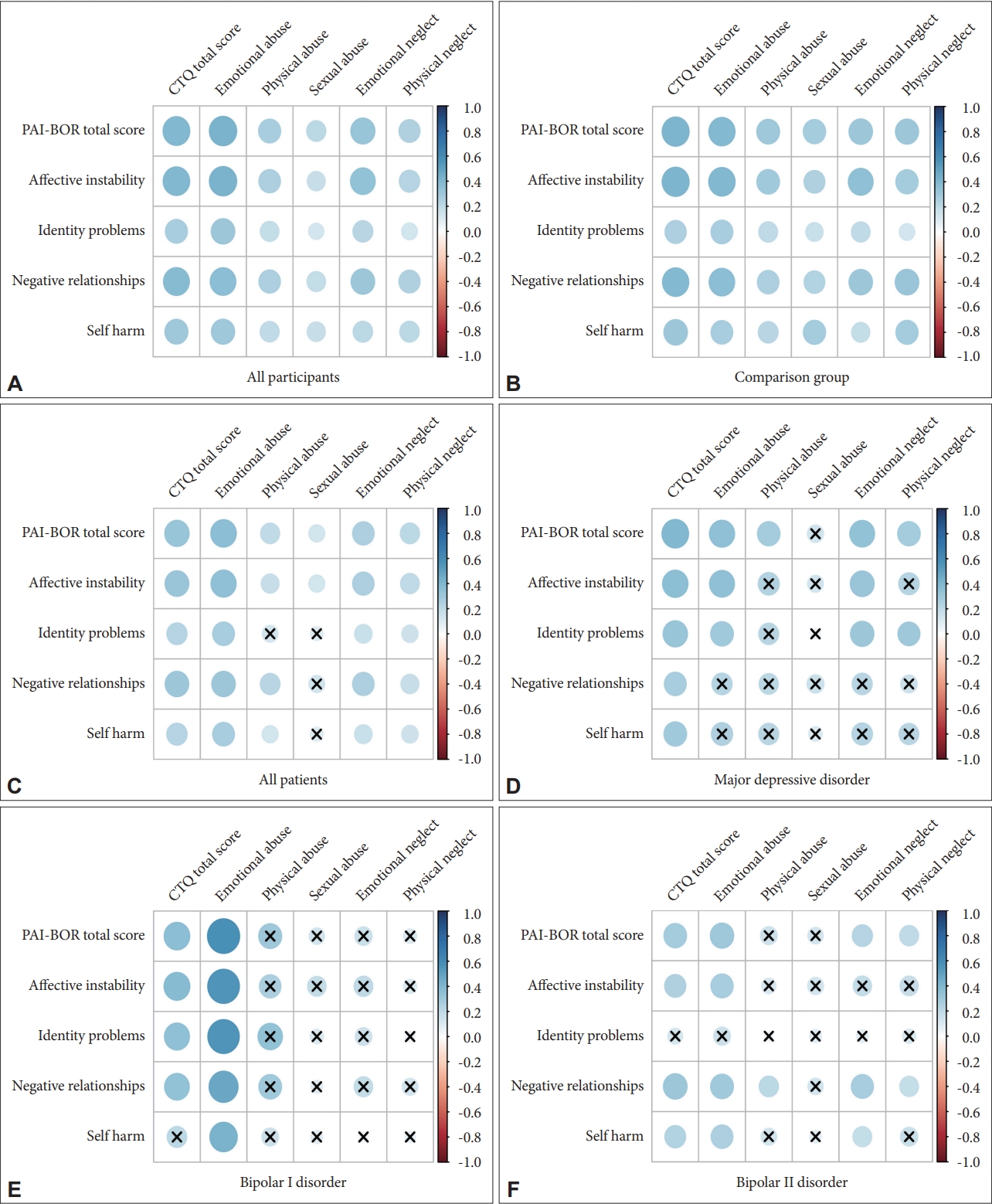
Partial correlation plot between Childhood Trauma Questionnaire (CTQ) scores and Borderline Personality Disorder Scale (PAIBOR) scores. Partial correlation coefficients (p<0.05) are shown in the figure and Partial correlation coefficients (p>0.05) are marked as X. Positive correlations are shown in blue color and negative correlations in red color. Color intensity is proportional to the partial correlation coefficients. A: All participants (N=1,222). B: Comparison group (N=734). C: All patients (N=488). D: Major depressive disorder (N=130). E: Bipolar I disorder (N=79). F: Bipolar II disorder (N=279). PAI-BOR, Personality Assessment Inventory–Borderline Features Scale; CTQ, Childhood Trauma Questionnaire-Short Form.
At the subscale level for CTQ, emotional abuse and emotional neglect were the factors most positively correlated with PAI-BOR total score (for emotional abuse: r=0.424 corrected p<0.001 in all participants; r=0.396, corrected p<0.001 in comparison group; r=0.370, corrected p<0.001 in all patients and for emotional neglect: r=0.330, corrected p<0.001 in all participants; r=0.319, corrected p<0.001 in comparison group; r=0.265, corrected p<0.001 in all patients) (Figure 2A-C, Supplementary Tables 2-4 in the online-only Data Supplement). When examined at the subscale level for PAI-BOR, affective instability and negative relationships were the factors most positively correlated with the total score for childhood trauma (for affective instability: r=0.400, corrected p<0.001 in all participants; r=0.419, corrected p<0.001 in the comparison group; r=0.321, corrected p<0.001 in all patients and for negative relationship: r=0.381, corrected p<0.001 in all participants; r=0.399, corrected p<0.001 in comparison group; r=0.316, corrected p<0.001 in all patients) (Figure 2A-C, Supplementary Tables 2-4 in the online-only Data Supplement).
In three patient groups (MDD, BD I, and BD II), CTQ total score was significantly correlated with PAI-BOR total score (r=0.400, corrected p<0.001 in MDD; r=0.372, corrected p<0.01 in BD I; r=0.289, corrected p<0.001 in BD II, Figure 2D-F and Supplementary Tables 5-7 in the online-only Data Supplement). In the subgroup analysis, emotional abuse was robustly correlated with PAI-BOR total score among the CTQ subscales, and two subscales of PAI-BOR (affective instability and negative relationships) were consistently associated with CTQ total score. In the analysis between subscales, physical or sexual abuse in CTQ and identity problems in PAI-BOR did not show robust correlation (Figure 2D-F, Supplementary Tables 5-7 in the online-only Data Supplement).
Regarding sex difference, we found that CTQ total score was positively correlated with PAI-BOR total score (r=0.454, corrected p<0.001 in all male participants; r=0.335, corrected p<0.001 in all female participants) (Supplementary Figures 1 and 2, Supplementary Table 8 in the online-only Data Supplement). At the subscale level for CTQ, emotional abuse and emotional neglect were the subtypes most positively correlated with PAI-BOR total score, in both sexes (r=0.456, corrected p<0.001, r=0.330, corrected p<0.001 in all male participants; r=0.339, corrected p<0.001, r=0.266, corrected p<0.001 in all female participants). At the subscale level for PAI-BOR, affective instability and negative relationships were the subtypes most positively correlated with CTQ total score in both sexes (r=0.449, corrected p<0.001, r=0.416, corrected p<0.001 in all male participants; r=0.329, corrected p<0.001, r=0.328, corrected p<0.001 in all female participants). We also conducted residual correlation analysis based on sex in all patients and in the comparison group (Supplementary Figures 3-6, Supplementary Tables 9 and 10 in the online-only Data Supplement).
DISCUSSION
The present study investigated the relationship between BPP and childhood trauma and compared BPP in patients with a diagnosed mood disorder versus a comparison group. We observed significant group differences regarding BPP in patients with MDD, BD I, and BD II, versus the comparison group. Patients with BD II had a higher level of BPP across the various features of BPP, including affective instability and identity problems. In addition, we found a significant positive association between BPP and childhood trauma after adjusting for potential confounding factors. Two childhood trauma subtypes, emotional abuse, and emotional neglect were most significantly associated with higher levels of BPP. Among the borderline features, affective instability and negative relationship were most positively correlated with childhood trauma. The correlation between the total score of childhood trauma and BPP score was robust for all mood disorders studied, including MDD, BD I, and BD II. However, some types of childhood trauma, such as physical abuse or sexual abuse, and some features of borderline pathology, including identity problems, lost their association during the subgroup analysis.
BD II scored significantly high regarding total BPP score compared to other mood disorders. A previous study [31] suggested that hypomanic symptoms lead to an overlapping of BD II and BPP; and that affective instability, a feature of BPP, could influence this vulnerability towards hypomanic symptoms. In line with this previous study, we also observed that affective instability reflected a higher score in patients with BD II. The association between BPP and BD has been widely studied. A few studies have directly compared the two disorders, though the diverse features of BPP were not examined between mood disorders [32,33]. Even though we did not statistically investigate the difference in BPP within each group, our findings provide additional evidence for the relationship between BPP and mood disorder and would assist clinicians in making differential diagnoses and treatment decisions.
During partial correlation analysis, BPP was found to be positively associated with childhood trauma both overall and in the comparison group. When compared with each subtype of childhood trauma, emotional abuse and emotional neglect were most correlated to BPP. In addition, affective instability, among all subscales of BPP, was mainly correlated to childhood trauma. Our findings are in accordance with previous studies. An earlier study in a general population [34] found that the participants with BPP report more childhood trauma experience than participants without BPP. Another study in patients with mood disorders [35] also revealed a significant relationship between BPP and childhood trauma. However, the present study not only discerned a relationship between BPP and childhood trauma in patients with mood disorders and the general population but also observed the relationship of childhood trauma subtypes on BPP and the features of BPP. These results could be helpful to find individuals predisposed to psychological risks as a result of specific childhood trauma.
One of the possible mechanisms for this association between childhood trauma and BPP is epigenetic changes [36]. Changes in DNA methylation have been studied and correlated with stressful early life events [37,38]. For instance, associations between NR3C1 methylation and early life stresses in patients with BPD were found, suggesting that changes in NR3C1 methylation can occur from early life stress experiences, and that persistence of these stress conditions can enhance vulnerability to developing BPD [37]. Moreover, methylation of other genes has been revealed as an important mediating factor influencing childhood trauma on BPP development [38-41]. Further studies on biological mechanisms between BPP and childhood trauma in relation to mood disorder status, specific features of BPP, and type of childhood trauma are warranted.
A previous study found that children who experienced emotional abuse were three times more likely to exhibit BPP than those without traumatic experiences [42]. Our findings were consistent with this study in that emotional abuse was the most significantly correlated subtype with BPP. Moreover, we observed in more detail that emotional abuse was significantly associated with affective instability and that emotional neglect also showed a significant association with the total score for borderline pathology in all participants. This finding of an association between emotional neglect and BPP is in line with previous results showing that emotional neglect in childhood was a predictive factor for BPP 10 years later [43].
A previous study [44] suggested that sexual abuse was the most important type of trauma that influences BPP. In our analysis, sexual abuse was correlated with the total score for BPP in the comparison group, all-patients group, and the male/female subgroups. However, in subgroup analysis in MDD, BD I, and BD II patients, sexual abuse was not associated with the total score for BPP. Possible underreporting of sexual trauma, the relatively small sample size of the subgroup analysis for each mood disorder, and multiple test corrections could have affected these results.
In the present study, affective instability and negative relationships were highly associated with childhood trauma in patients with MDD, BP I, and BP II, and in the comparison group. These findings are in line with previous studies. In a neuromagnetic brain activity study [45], participants who failed regarding emotional regulation reported childhood trauma experiences. Goodman et al. [46] also revealed an association between affective measurements, including lability and intensity, and childhood trauma among patients with borderline personality disorder. In addition, children who had more childhood trauma experiences reported a higher level of negative relationships than those without childhood trauma [47].
The present research had several limitations. The main limitation was that our results made it difficult to draw any causal relationship between childhood trauma and BPP. We conducted a cross-sectional study that did not establish a temporal relationship between exposure and result [48]. Moreover, CTQ, used as a clinical instrument in our study, is a self-report assessment. False-negative reports occur when participants refuse to report distressing memories or when older participants are unable to recall past episodic memories from childhood. We also did not ask for family information during childhood as a variable. Our participants were mostly adults, with their average age being >30 years. Although we statistically controlled for various variables, such as marital status and psychiatric family history, we did not control childhood family information, which has been mentioned as a crucial factor in a previous study [49].
The present study had the following strengths: Several previous studies on childhood trauma or BPP did not include a comparison group [24,50] nor did they conduct subgroup analysis for mood disorder [51,52]. In addition, few studies investigated the relationship between the type of childhood trauma and developed borderline features [53,54]. Contrarily, our study investigated the association in various subgroups, including patients with MDD, BD I, and BD II, and a comparison group. We also evaluated the correlation between childhood trauma and BPP for each subscale. Therefore, we were able to elucidate comprehensive pictures for the association between BPP, childhood trauma, and various mood disorders.
In conclusion, the present study showed the relationship between BPP features and mood disorder patients, including MDD, BD I, and BD II, and a history of childhood trauma. Patients with BD II are more likely associated with BPP features than BD I or MDD. Mood disorder patients with a severe history of childhood trauma, especially emotional trauma, may have higher BPP features. Also, affective instability might be more related to childhood trauma. These results could improve the recognition of features of BPP in mood disorder patients and stress the importance of the childhood environment in relation to the later development of both.
Supplementary Materials
The online-only Data Supplement is available with this article at https://doi.org/10.30773/pi.2022.0114.
Total and subscale scores of the Borderline Personality Disorder Scale (PAI-BOR) and Childhood Trauma Questionnaire (CTQ) according to groups
Partial correlation coefficient between Childhood Trauma Questionnaire (CTQ) scores and Borderline Personality Disorder Scale (PAI-BOR) scores in all participants (N=1,222)
Partial correlation coefficient between Childhood Trauma Questionnaire (CTQ) scores and Borderline Personality Disorder Scale (PAI-BOR) scores in comparison group (N=734)
Partial correlation coefficient between Childhood Trauma Questionnaire (CTQ) scores and Borderline Personality Disorder Scale (PAI-BOR) scores in all patients (N=488)
Partial correlation coefficient between Childhood Trauma Questionnaire (CTQ) scores and Borderline Personality Disorder Scale (PAI-BOR) scores in major depressive disorder (N=130)
Partial correlation coefficient between Childhood Trauma Questionnaire (CTQ) scores and Borderline Personality Disorder Scale (PAI-BOR) scores in bipolar I disorder (N=79)
Partial correlation coefficient between Childhood Trauma Questionnaire (CTQ) scores and Borderline Personality Disorder Scale (PAI-BOR) scores in bipolar II disorder (N=279)
Pearson correlation coefficient between Childhood Trauma Questionnaire (CTQ) scores and Borderline Personality Disorder Scale (PAI-BOR) according to sex in all participants (N=1,222)
Pearson correlation coefficient between Childhood Trauma Questionnaire (CTQ) scores and Borderline Personality Disorder Scale (PAI-BOR) according to sex in all patients (N=488)
Pearson correlation coefficient between Childhood Trauma Questionnaire (CTQ) scores and Borderline Personality Disorder Scale (PAI-BOR) according to sex in comparison group (N=734)
Partial correlation coefficients (p<0.05) are shown in the figure and Partial correlation coefficients (p>0.05) are marked as X. Positive correlations are shown in blue color and negative correlations in red color. Color intensity is proportional to the partial correlation coefficients. Partial correlation plot between Childhood Trauma Questionnaire (CTQ) scores and Borderline Personality Disorder Scale (PAI-BOR) scores in all male participants (N=503).
Partial correlation coefficients (p<0.05) are shown in the figure and Partial correlation coefficients (p>0.05) are marked as X. Positive correlations are shown in blue color and negative correlations in red color. Color intensity is proportional to the partial correlation coefficients. Partial correlation plot between Childhood Trauma Questionnaire (CTQ) scores and Borderline Personality Disorder Scale (PAI-BOR) scores in all female participants (N=719).
Partial correlation coefficients (p<0.05) are shown in the figure and Partial correlation coefficients (p>0.05) are marked as X. Positive correlations are shown in blue color and negative correlations in red color. Color intensity is proportional to the partial correlation coefficients. Partial correlation plot between Childhood Trauma Questionnaire (CTQ) scores and Borderline Personality Disorder Scale (PAI-BOR) scores in all male patients (N=158).
Partial correlation coefficients (p<0.05) are shown in the figure and Partial correlation coefficients (p>0.05) are marked as X. Positive correlations are shown in blue color and negative correlations in red color. Color intensity is proportional to the partial correlation coefficients. Partial correlation plot between Childhood Trauma Questionnaire (CTQ) scores and Borderline Personality Disorder Scale (PAI-BOR) scores in all female patients (N=330).
Partial correlation coefficients (p<0.05) are shown in the figure and Partial correlation coefficients (p>0.05) are marked as X. Positive correlations are shown in blue color and negative correlations in red color. Color intensity is proportional to the partial correlation coefficients. Partial correlation plot between Childhood Trauma Questionnaire (CTQ) scores and Borderline Personality Disorder Scale (PAI-BOR) scores in all male comparison group participants (N=345).
Partial correlation coefficients (p<0.05) are shown in the figure and Partial correlation coefficients (p>0.05) are marked as X. Positive correlations are shown in blue color and negative correlations in red color. Color intensity is proportional to the partial correlation coefficients. Partial correlation plot between Childhood Trauma Questionnaire (CTQ) scores and Borderline Personality Disorder Scale (PAI-BOR) scores in all female comparison group participants (N=389).
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Ji Seon You, Chan Woo Lee, Tae Hyon Ha, Woojae Myung. Data curation: Chan Woo Lee, Yoonjeong Jang, Hyeona Yu, Joohyun Yoon, Sunghee Oh, Yun Seong Park, Hyun A Ryoo, Nayoung Cho, Jong Hun Lee. Funding acquisition: Woojae Myung. Investigation: Ji Seon You, Chan Woo Lee, Yoonjeong Jang, Hyeona Yu, Joohyun Yoon, Sunghee Oh, Yun Seong Park, Hyun A Ryoo, Hong Kyu Ihm, Nayoung Cho, Jong Hun Lee. Methodology: Ji Yoon Park, Chan Woo Lee, Yeong Chan Lee, Hong-Hee Won, Hyo Shin Kang, Tae Hyon Ha, Woojae Myung. Supervision: Hong-Hee Won, Hyo Shin Kang, Tae Hyon Ha, Woojae Myung. Writing—original draft: Ji Yoon Park, Chan Woo Lee, Yoonjeong Jang, Hyeona Yu, Joohyun Yoon. Writing—review & editing: all authors.
Funding Statement
This work was supported by the SNUBH Research Fund (grant no. 09- 2020-003; WM). This work was also supported by a National Research Foundation (NRF) of Korea Grant, funded by the Korean government (NRF-2021R1A2C4001779; WM). This research was additionally supported by the Korea Medical Device Development Fund grant, funded by the Korean government (the Ministry of Science and ICT; the Ministry of Trade, Industry, and Energy; the Ministry of Health & Welfare; the Ministry of Food and Drug Safety) (Project Number NTIS 9991006915, KMDF_ PR_20200901_0250). The funding body had no role in the study design, data collection, data analysis, data interpretation, or writing of this report. The corresponding author had full access to all the data in this study and had final responsibility for the decision to submit for publication.

