Hospital-Based Case Management for Suicide High-Risk Group Using Delphi Survey
Article information
Abstract
Objective
As of 2019, suicide is serious problem in Korea, with the highest suicide rate among OECD countries. To reduce suicide rates Emergency Department Based Post-Suicide Attempt Case Management carried out with government funding in South Korea, but it is insufficient to address the issue. Aim of this study is to prevent suicide attempts through continuous provision of mental health services even after discharge from acute care.
Methods
We selected 15 mental health specialists who are multidisciplinary experts in Suicide Prevention. Two-round Delphi survey was conducted on them to reach an agreement for hospital-based case management.
Results
The first Delphi survey consisted of 8 areas and 39 questions. Among them, 30 questions draw agreement above the reference value. The second Delphi survey, consisted of 37 questions, resulted in 32 above-standard questions.
Conclusion
Consensus was reached in most category of the Hospital Based Case Management for Suicide High-Risk Group. Core of the developed plan was to provide services to patients who visited the hospital, pursue the stability and universalization of services through a medical insurance fee system. In the future, hospital-based case management service will be implemented as a new model contributing to the reduction of suicide rates in Korea.
INTRODUCTION
Suicide accounts for 4.6% of all deaths in Korea [1]. According to a Korean psychological autopsy report, 84.5% of suicides had mental health problems, but active management of mental disorders was insufficient, leading to a high suicide rate in Korea [2]. Since suicide attempts are known to have many reattempts within 24 months after the initial effort, suicide attempters are a high-risk group that requires active intervention [3-5]. However, in the pilot project conducted by the Mental Health and Welfare Center in Seoul and emergency departments at five hospitals, the patient’s consent rate was meager, at only 12%. In 2009, Professor Seongho Min’s team at Wonju Severance Christian Hospital assigned a case manager of the Mental Health Welfare Center to the emergency room for the first time for follow-up management for suicide attempters in the emergency room. The follow-up showed remarkable results where the consent rate for case management was 65% or more. The Ministry of Health and Welfare’s pilot project began in 2011 at Wonju Severance Christian Hospital, Catholic University Hospital, and Kyunghee University Hospital. Since 2013, Emergency Department Based Post-Suicide Attempt Case Management has been implemented nationwide through the Korea Suicide Prevention Center [6,7]. As of 2019, 63 medical institutions carry out Emergency Department Based Post-Suicide Attempt Case Management. However, the number is still insufficient, considering the current status of emergency rooms in Korea at around 500 [8,9].
On the other hand, the need to include not only suicide attempters, but also patients discharged from the Department of Psychiatry to the suicide high-risk group was raised. The rate of suicide death within 90 days after discharge was nearly 20 times higher in patients hospitalized for mental illness than those hospitalized for non-psychiatric diseases [10]. The suicide rate was highest during the first 3 months after discharge and did not until several years later [11]. Some studies have shown that the suicide rate with a history of hospitalization in the Department of Psychiatry is 50–70 times higher than that of general adolescents [12].
According to previous studies, intensive case management such as face-to-face counseling, phone counseling, home visits, and emergency room accompaniment for those at high risk of suicide effectively assisted suicide prevention [13-15]. A Swedish study demonstrated showed that phone counseling improved overall function and suicidal thoughts in 216 suicide attempters [16]. In an Australian survey of 772 patients admitted to university hospitals for poisoning, the number of suicide reattempts reduced by 50% in the group to which postcards were sent [17,18]. Additionally, when face-to-face counseling once a week and phone counseling twice a week were conducted for 12 months to 30 patients who received inpatient treatment from the Department of Psychiatry for suicide attempts in Australia; depression, suicidal thoughts, and quality of life significantly improved in the case management group [19]. Accordingly, in Japan, the follow-up care of suicide attempters in the emergency room has been included in health insurance since 2016 for effective case management, based on ACTION-J and the Assertive Community Treatment (ACT) program using insurance funds is being implemented in New York State in the United States [20].
Meanwhile, as a limitation to existing management of persons at high risk of suicide, the dropout rate when the care was linked to the community was high [21]. Treatment compliance was low, and there was a tendency to refuse mental health services [22,23]. Therefore, the patients discharged from the Department of Psychiatry had difficulty in receiving case management and community care despite being at a high risk of suicide. However, until now, no policy project on hospital-based case management has been carried out in South Korea. To overcome this problem and effectively treat the suicide high-risk group, devising interventions for suicide attempters and patients discharged from the Department of Psychiatry will effectively reduce suicide deaths [24]. In other words, the goal of this study is to develop a hospital-based case management model that continuously provides mental health services even after the patient discharged from the hospital upon acute treatment.
METHODS
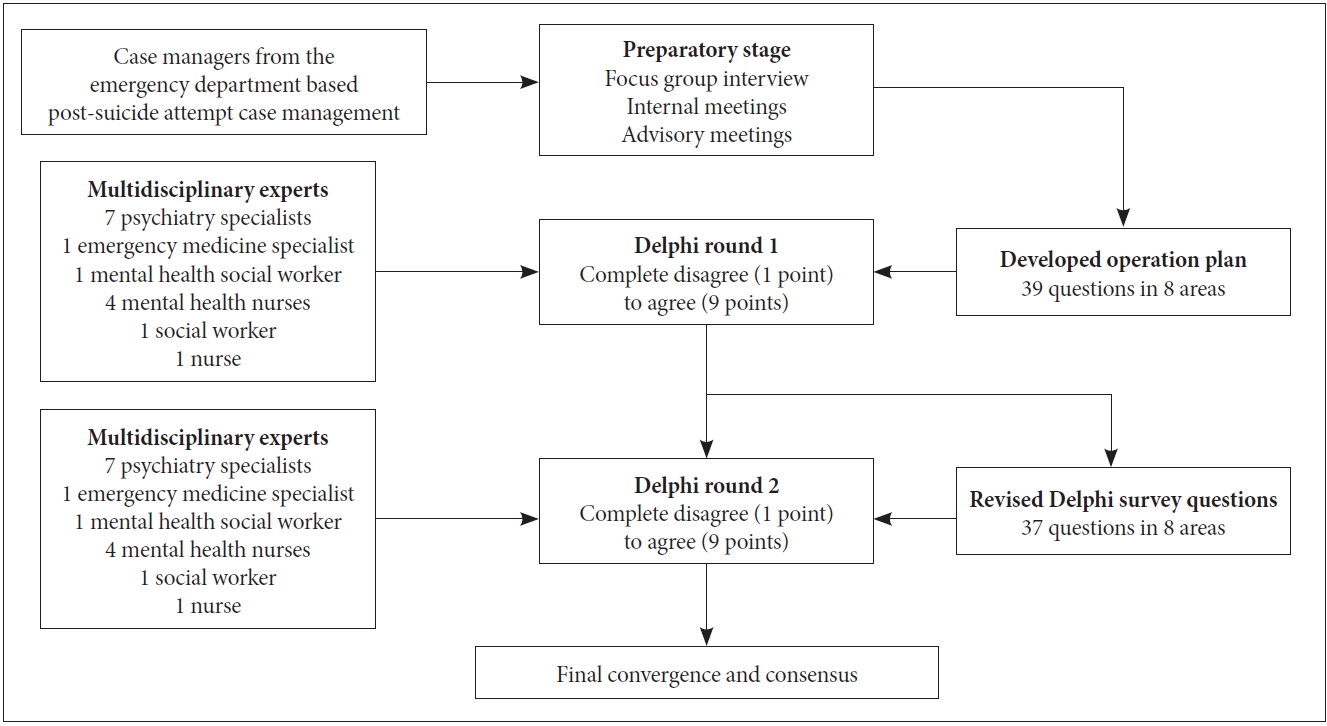
Delphi survey
In this study, through focus group interviews, internal meetings, and advisory meetings targeting the case managers from the Emergency Department Based Post-Suicide Attempt Case Management, we developed an operational plan for hospitalbased case management services for inpatients in the department of psychiatry (Figure 1). A Delphi survey on the developed plan was conducted for multidisciplinary experts, and the consensus was reached on the qualification requirements, working guidelines, adequate workforce, and the medical insurance cost. The Delphi survey was conducted twice between May and June 2019. For the first Delphi survey, a focus group interview was conducted with case managers from the Emergency Department Based Post-Suicide Attempt Case Management. Afterward, opinions were collected from the expert panel, and the first survey was composed of 39 questions in 8 areas. Each question was evaluated on a 10-point Likert scale, from completely disagree (1 point) to agree (9 points), and participants gave their opinions for each area.
The second Delphi survey consisted of 37 questions in 8 areas upon reflecting the questions that did not meet the first survey criteria, and the questions participants wanted to be revised. Further, the results from the first survey were presented so that participants could compare their responses and respond again.
Analysis of the Delphi survey results
Following the previous studies, the mean and standard deviation, convergence rate, content validity, and consensus were analyzed [25]. Convergence was the number of respondents who responded with agree (7 points) or higher than the respondents’ total number for each question. Each item was judged to have content validity when the score was 0.49 or higher, based on the Content Validity Ratio (CVR) [26]. The consensus was measured by the coefficient variation (CV), obtained by dividing the standard deviation by the arithmetic mean. The result was interpreted as stable when the CV was 0.5 or less [27].
This research was corresponded to IRB review exemption (KHUH-2018-02-004) from Kyung Hee University Hospital Institutional Review Board, and was conducted in accordance with research protocol.
RESULTS
Characteristics of research participants
The Delphi process derives results by relying on expert judgment; thus, appropriate participant selection is essential [26]. In this survey, 15 people, including doctors in hospital-based suicide prevention projects, the director of Emergency Department Based Post-Suicide Attempt Case Management, and mental health specialists of the Mental Health and Welfare Center, were selected. The participants were eight males (53.3%) and seven females (46.7%), with nine in their 40s (60%), three in their 30s (20%), and three in their 50s (20%). There were eight doctors (53.3%), five mental health specialists (four mental health nurses and one mental health social worker, 33.3%), and two staff members (one nurse and one social worker, 13.4%). The response rate for both the first and the second Delphi surveys was 100%.
Delphi survey results
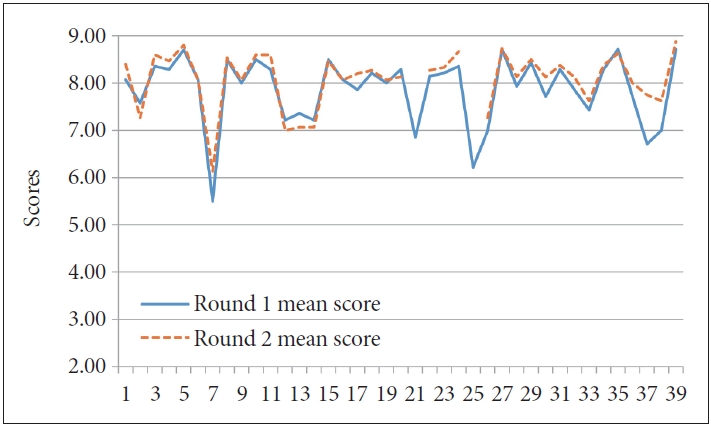
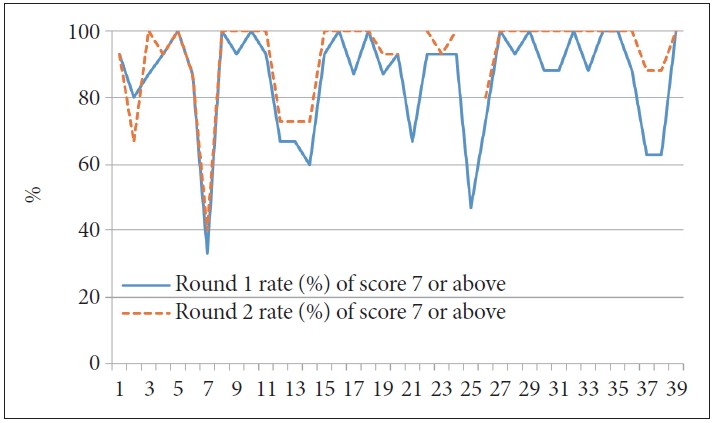
Delphi survey area and questions, mean score, convergence, content validity, and consensus for each survey are shown in Tables 1–4. Moreover, Figures 2 and 3 represent the mean score and convergence for each question in the first and second surveys.

Delphi results for the relationship with current case managements and hospital based case management
Items for case management subjects included 1) “patients that attempted suicide within one year while being treated for diseases such as schizophrenia, bipolar disorder, depression, and alcohol use disorder,” 2) “outpatients or patients under collaborative care at high risk of suicide,” 3) “suicide attempters that have been hospitalized and those who are considering discharge of suicide high-risk group,” and 4) “suicide attempters and persons at high risk of suicide that visited the hospital through emergency rooms.” In the first survey, the convergence rate for each item was 85% or more, the consensus was high with 0.15 or less, and content validity was high with CVR of 0.60 or higher. However, in the second survey, the convergence rate for the item “outpatients or patients under collaborative care at high risk of suicide” decreased from 0.80 to 0.67.
The items for the composition and qualification requirements of the multidisciplinary team were 1) “psychiatrists,” 2) “case managers (mental health specialists or person with more than three years of working experience at the Department of Psychiatry),” and 3) “emergency medicine specialists and doctors from other departments.” As a result of the two rounds of surveys, “psychiatrists” and “case managers” met the convergence rate standards and consensus, but “emergency medicine specialists and doctors from other departments” did not. The revised item for the second survey still did not meet the criteria.
In the case management method and period, seven items about management method, standards, and period for inpatients and outpatients were surveyed. The convergence rate for case management criteria and period was 60%–67% in the first round, and CVR was 0.20–0.33, which did not meet the criteria. However, in the second round, the convergence rate and the CVR of the above items increased to 73% and 0.47, respectively.
In regards to case management, eight items were surveyed: 1) “initial and regular evaluation of suicide risk,” 2) “suicide risk-related education,” 3) “provision of treatment-related information (drugs, symptom management, etc.),” 4) “hospital visits or home visits,” 5) “family intervention,” 6) “comprehensive evaluation of the subjects’ needs and circumstances and connection with the welfare resources,” 7) “other physical care,” and 8) “establishment of emergency response system in case of suicide reattempts.” In the first round, all items except for “other physical care” (convergence rate 0.67, CVR 0.33) met the criteria (convergence rate 0.87–1.00, CVR 0.73–1.00). Therefore, “other physical care” was removed from the second round, and the criteria were met in all items (convergence rate 0.93–1.00, CVR 0.87–1.00).
In cooperation with existing case management services and the establishment of a connection system, two items were surveyed: 1) “provision of service based on the need for connection of services for the subjects” and 2) “establishment of a suicide prevention network for local communities and hospitals in relevant areas and preparation and utilization of a list of related organizations for connection.” In this area, convergence rate and consensus criteria were met in both the first round (convergence rate 0.93, CVR 0.87) and the second round (convergence rate 0.93–1.00, CVR 0.87–1.00).
In “relationship with the existing Emergency Department Based Post-Suicide Attempt Case Management,” 2 items were surveyed: 1) “requests can be made after providing a service equivalent to the manual for suicide attempters in emergency rooms” and 2) “the provision of services to suicide high-risk groups that are not registered as suicide attempters in the emergency room is restricted until the change in service provision criteria is approved. It is recommended that the hospital hires a separate workforce for hospital-based case management services”. In the first round, the item “requests can be made after providing a service equivalent to the manual for suicide attempters in emergency rooms” did not meet the criteria with a convergence rate of 47% and CVR of -0.07; thus, it was removed from the second round. For the item, “the provision of services to suicide high-risk groups that are not registered as suicide attempters in the emergency room is restricted until the change in service provision criteria is approved. It is recommended that the hospital hires a separate workforce for hospital-based case management services,” the convergence rate was 73% and CVR 0.47 in the first round. However, it increased in the second round to an 80% convergence rate and 0.60 CVR.
In “recordkeeping and evaluations,” two items were surveyed: 1) “All of Hospital Based Case Management for Suicide in High-Risk Group are medical records and kept under the relevant law” and 2) “A separate report is prepared through annual self-evaluation of key indicators such as consent rate to case management, service provision rate, and suicide reattempt rate etc.” Results from both the first round (convergence rate 0.93–1.00, CVR 0.87–1.00) and the second round (convergence rate 0.87–1.00, CVR 1.00) met the criteria.
As for health insurance fee for case management, a survey was conducted for eight psychiatrists that are related to the medical insurance fee: 1) “general outpatient fee at the department of psychiatry,” 2) “psychiatric outpatient assessment report preparation fee,” 3) “psychiatric outpatient drug administration fee, education fee for the medication, and long-term injection fee,” 4) “multidisciplinary self-injury • suicide evaluation fee,” 5) “Emergency administrative support fee,” 6) “self-injury • suicide status evaluation fee,” 7) “emergency intervention fee for the acute phase of suicide,” 8) “fee for social work against suicide,’’ 9) “continuing support fee against suicide,” 10) “suicide follow-up monitoring fee,” and 11) “additional fees for the psychiatric emergency response team,” and a standing member of the Health Insurance Review and Assessment Service and a director of insurance at the Korean Neuropsychiatric Association participated in this process. In the first round, “continuing support fee against suicide” and “suicide follow-up monitoring fee” did not meet the convergence rate and CVR criteria with 63% and 0.25, respectively. Nonetheless, in the second round, convergence rate and CVR were over 88% and 0.75, respectively, in all items.
DISCUSSION
In developing hospital-based case management services for suicide high-risk groups, this study conducted two Delphi surveys with experts in suicide prevention in Korea. A survey of experts is a structured communication technique and is one of the methods used when specific policy decisions need to be made in situations where existing data is insufficient [28]. In Delphi surveys, the initial questions’ design is important [29]. Nevertheless, previous studies in hospital-based case management using Delphi processes were inadequate. Therefore, this study conducted focus group interviews to reflect expert panels’ opinions on related tasks in academia and clinical settings. Based on this, the initial items consisting of 39 questions in 8 areas were developed. Afterward, the average score, convergence, CVR, and consensus were measured to evaluate experts’ convergence and consensus.
When the Delphi survey results were categorized by area, there was no disagreement in providing services for inpatients and emergency room patients in case management. However, there was a low level of convergence for targeting outpatients or patients under collaborative care. Furthermore, a need for a more clear definition of the ‘suicide high-risk group’ was raised. If necessary, active hospitalization is recommended for the outpatients at high risk of suicide to ensure safety. Thus, it is often difficult to continue outpatient-based treatment. Hospital-based case management can be considered at the time of discharge.
Meanwhile, as a result of the Emergency Department Based Post-Suicide Attempt Case Management, the rate of refusal to go through case management was high when there was no history of treatment in the department of psychiatry, the patient did not recognize the suicide attempt, and when the patient refused to respond to the initial survey [30]. Additionally, prejudice and lack of insight about the psychiatry department were pointed out as the reasons for suicide attempters in the emergency room refusing treatment in the psychiatric department [21]. Moreover, considering the treatment compliance and understandings of patients and caregivers who do not have a medical history in psychiatry, it seems that the rate of consensus on targeting suicide high-risk persons among the patients under collaborative care was not high. Consequently, in future Hospital Based Case Management for Suicide in High-Risk Group, prioritizing inpatients and emergency room patients rather than outpatients and those under collaborative care may be recommended.
Regarding the multidisciplinary team’s composition and qualification requirements, “emergency medicine specialists and doctors from other departments” showed a very low convergence rate and consensus. As well, the opinions suggested were “participation of other departments only when necessary,” “use of in-hospital collaboration,” and “environmental intervention of the community, in addition to the treatment for the disease is more important.” Therefore, the item was revised by adding the phrase “when a multidisciplinary evaluation is necessary,” but the final consensus could not be reached. Currently, the medicine specialists’ role in Emergency Department Based Post-Suicide Attempt Case Management is very important. However, since this research is on developing a hospital-based case management model, experts recognized that medical staffs in the psychiatry department are important in managing inpatients after the discharge, in line with questions about case management area. This may be due to the emergency medicine department’s difficulty attending to long-term case management and differences in the perceptions of highrisk suicide groups between departments. According to previous studies, the rate of suicide attempters treated in the emergency room getting referred to the psychiatry department was lower than the rate deemed necessary by the emergency medicine department because the patients and the guardians refused to do so [31]. Therefore, it is important to provide necessary services on a case-by-case basis even if they do not agree to treatment with the psychiatry department. In the long run, efforts to resolve differences in perceptions by departments are needed.
Further, the multidisciplinary team members of ACT originally are doctors and nurses from the department of psychiatry, social workers, rehabilitation counselors, and counselors for drug dependence [32]. In ACTION-J, it was limited to doctors and nurses of the psychiatry department, social workers, and clinical psychologists [33]. Therefore, at the present stage, the hospital-based case management service model can be focused on the department of psychiatry. However, even in the case of ACT in the United States, the primary care physicians and family medicine specialists are increasingly being assigned to 1 in 1,000 patients. Therefore, transferring specialists from other departments may need to be actively considered in the future.
In the case management method and period, the convergence rate of management target and method was high, but the management standard and period were low. According to a previous study that used the Delphi survey, the consensus rate of survey items agreed in advance through other guidelines or publications was high [34]. In this study, the management criteria and period of hospital-based case management were redefined by referring to overseas cases (ACTION-J: management once a month for six months) [33], so the convergence and consensus rate were relatively low. Additionally, experts suggested that, in considering the overlap with the existing case management service, compliance of the subjects, and the intensity of work of case managers, it is necessary to reduce the number and duration of case management and that the focus group and the maintenance group should be clearly defined. In terms of the intensity of work, it is necessary to supplement the management method, standards, and period in consideration of the work intensity, capacity, and exhaustion of case managers through a randomized controlled clinical trial or pilot study of a hospital-based case management service. Therefore, randomized controlled clinical trials are currently underway, with the support of the Korea Health Industry Development Institute.
Regarding case management contents, items other than “other physical care” showed a high convergence and consensus level. This may be due to a similar reason that the “emergency medicine specialists and doctors from other departments” in the “composition and qualification requirements of a multidisciplinary team” was not agreed upon; therefore, the “other physical care” item was removed. In the Mobile Integration Team (MIT) service, a case management program after discharge in New York State, the community connection of elderly patients with mental disorders and physical illness was included in the case management [20], and ACTION-J also recommends hospital visits for treatment of underlying diseases [33]. However, the importance of physical care is evaluated relatively low by experts in Korea, so further discussion through studies and pilot projects is necessary. Moreover, given the reality in Korea in which the family’s role and authority are significant [35], intervention and education for the family and the patient should be included in the case management content.
In “cooperation with existing case management services and establishment of a connection system” and “relationship with the existing Emergency Department Based Post-Suicide Attempt Case Management,” there was consensus in the plan to hire separate personnel from those that manage the Emergency Department Based Post-Suicide Attempt Case Management. However, the convergence rate and CVR were low. Regarding this, opinions such as “it is difficult to link the cases to community-based management team after being managed by the Emergency Department Based Post-Suicide Attempt Case Management,” “there needs to be a discussion on the difference and division of work between the case management by the existing Emergency Department Based Post-Suicide Attempt Case Management and the community-based case management,” and “it is necessary to integrate case management services that are currently being carried out in the basic center/city-wide center/suicide prevention center/ Emergency Department Based Post-Suicide Attempt Case Management.” Therefore, in the second round, the item that “requests can be made after providing a service equivalent to the manual for suicide attempters in emergency rooms” was removed. Cooperation with existing case management services and establishing the linkage system will be of high importance, given many experts’ opinions. Emergency Department Based Post-Suicide Attempt Case Management currently being implemented has its advantage that the government supports the case manager’s labor costs. Therefore, the case manager can solely focus on the suicide attempters in the emergency room.
Notwithstanding, a disadvantage is in the incomplete business stability, such as the case manager being contract workers [3]. Hospital-based case management will be easy to secure employment security through direct employment of case managers in hospitals by the medical insurance system, but whether there will be enough money to hire case managers is the key. In Japan, services are provided through the medical insurance system. However, the employed case managers also provide inpatients programs, such as other in-hospital programs like ward and family education. Therefore, in the short-term, emergency department-based case management through government funding and hospital-based case management through the medical insurance system will need to be performed simultaneously. Nonetheless, in the long run, integration of the two services will be necessary.
Therefore, since all items in the medical insurance system for case management met the criteria, all items’ convergence and consensus are of great significance. In Japan, after introducing the emergency room-based follow-up service of suicide attempters (ACTION-J), the intensive case management of suicide attempters in the emergency room reduced the suicide reattempt rate [33]. The program was incorporated into the medical insurance fee system by the Ministry of Health, Labor and Welfare [36]. ACT, in the United States, is also operated by Medicaid to ensure financial and employment security. The cost is charged for each service [37]. Therefore, to effectively implement hospital-based case management, it is essential to secure finance by connecting with the National Health Insurance Service. The significance of this study is that the basis for this was prepared through expert consensus. The Delphi survey showed that the convergence rate of “continuing support fee against suicide” and “suicide follow-up monitoring fee” was low. The experts suggested that the names of the items “continuing support fee” and “follow-up monitoring fee” were awkward. Previous studies revealed that the suicide reattempt rate decreased when the subject was in constant contact with the psychiatry department in various ways, such as outpatient treatment, provision of green cards, letters and postcards, and mobile messengers [13,16-18,38]. Therefore, continuous support and follow-up need to be part of the medical insurance cost and included in the case management. However, the effects of nonface-to-face contacts, such as phone and text messages, were not significant enough [38]. Thus, the convergence rate for the “suicide follow-up monitoring fee” may have been low. Moreover, considering the socio-economic difficulties of high-risk groups for suicide [39,40], it is necessary to reduce the copayment. Even so, various opinions, such as applying special exceptions of severe mental illness for a short period, were raised, so the “continuing support fee against suicide” had a low convergence rate.
As a result of this study, suicide prevention experts agreed on the necessity of hospital-based case management, and most of the developed operational plans were agreed on. The core of the developed plan was to provide services to patients who visited the hospital, conduct home visits, treat the patients directly, and pursue the stability and universalization of services through a medical insurance fee system. On method, standards, and period of hospital-based case management, which had a relatively low consensus rate, pilot project, additional research, and feedback from experts will be necessary. And the relationship with the existing Emergency Department Based Post-Suicide Attempt Case Management will require further discussion after the project expands through a parallel period to warrant employment security for case managers. Above all, it is essential to verify the evidence through a randomized controlled clinical trial such as Action-J in Japan. The advantages of this study are that the opinions of experts who are currently working in Emergency Department Based Post-Suicide Attempt Case Management and mental health and welfare centers in various positions such as psychiatry, emergency medicine, social welfare, and nursing were reflected, and the response rate of the panel was 100%. This study’s limitations are that the number of expert panelists was small, with 15 panelists, and eight specialists participated in the area of case management health insurance. However, suppose the number of participating panels is about 15, the median difference is not large [41]. A psychiatrist who is currently active as a standing member of the Health Insurance Review and Assessment Service and a director of insurance at the Korean Neuropsychiatric Association participated in the study. Accordingly, we believe the limitation may be supplemented.
In the future, it is expected that the hospital-based case management service based on the evidence in the field will be implemented as a new model that activates cooperation between emergency rooms, hospitals, and local communities across the country through randomized controlled studies and pilot projects, thereby contributing to the reduction of suicide rates in Korea.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Jong-Woo Paik, a contributing editor of the Psychiatry Investigation, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Author Contributions
Conceptualization: Jong-Woo Paik, Hwa-Young Lee. Data curation: Soung Nam Kim, Jeungsuk Lim. Formal analysis: Jeungsuk Lim. Methodology: Sang Min Lee, Hwan Lee. Supervision: Kyoung-Uk Lee. Writing—original draft: Hwan Lee, Jeungsuk Lim. Writing—review & editing: Haewoo Lee, Boung Chul Lee, Jong-Woo Paik, Hwan Lee.
Funding Statement
This study was supported by a grant of the Korea Mental Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (grant number: HM18C2083).
This research was supported by a grant of the Korea Health Technology R&D project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI19C0481, HC19C0307).