Current and Future Trends in Hospital Utilization of Patients With Schizophrenia in Korea: A Time Series Analysis Using National Health Insurance Data
Article information
Abstract
Objective
This study aimed to investigate trends in hospital utilization of patients with schizophrenia during the last 10 years in Korea and to predict future trends using time series analysis.
Methods
We determined the numbers of patients receiving outpatient or inpatient treatment for schizophrenia per month between 2010 and 2019, using National Health Insurance claims data. Facebook’s Prophet was used to fit time series models based on observations for the previous 120 months, and to predict trends over the next 36 months.
Results
The number of hospitalized patients per month has declined rapidly since 2015, but the monthly number of outpatient visits has steadily increased. Monthly hospital utilization has increased in patients aged ≤29 and ≥50 years, but has declined rapidly since 2014–2015 in patients in their 30s and 40s. The upward trend in overall hospital utilization has slowed considerably in recent years. These trends are expected to continue over the next few years.
Conclusion
This study revealed some notable changes in the hospital utilization patterns of patients with schizophrenia in recent years. There is a need to closely monitor and anticipate potential problems caused by these changing trends.
INTRODUCTION
Schizophrenia is a severe and chronic mental illness characterized by delusions, hallucinations, disordered formal thought, disorganized behaviors, negative symptoms, and cognitive impairment. In addition, many patients are unemployed due to their functional deficits and social isolation [1]. They are usually hospitalized several times throughout their lifetime due to discontinuation of treatment and subsequent recurrence of symptoms [2]. In particular, some untreated patients are involved in violence [3]. Therefore, schizophrenia places huge health, economic, and social burdens on patients, their families, and society [4].
Epidemiological studies have shown that the lifetime prevalence of schizophrenia ranges from 0.3%–0.7% worldwide [5]. Lifetime and 12-month prevalence rates of schizophrenia spectrum disorders in Korea have been reported as 0.5% and 0.2%, respectively [6]. Meanwhile, according to the National Health Insurance, the number of people treated for schizophrenia per year increased gradually from 2012 to 2017 in Korea [7]. This may be due to an increase in the number of patients visiting hospitals due to improved awareness of the importance of early diagnosis and ongoing treatment of schizophrenia [8,9]. However, experts have estimated that a considerable number of people affected by schizophrenia in Korea have still not received treatment [10].
The Korean government has implemented deinstitutionalization policies to support outpatient and community-based care [11], although hospital admission is still the main approach to the treatment of schizophrenia in Korea [12]. In particular, the Mental Health and Welfare Law, which strengthened regulations regarding involuntary admission, came into force in May 2017 [13]. As a result, patients, caregivers, and clinicians are now facing institutional changes [14]. However, violence perpetrated by patients with psychotic disorders has become a social issue in recent years [15], and experts have expressed concern about several problems caused by the rapid decrease in hospitalization rate and lack of preparedness of patients for deinstitutionalization [13].
Against this background, we expected to find significant changes in the hospital utilization of patients with schizophrenia in recent years. Time series modeling techniques are useful for analyzing patterns of change in a given variable, modelling seasonal effects, assessing the immediate and long-term impact of a salient event, and forecasting future trends [16]. Therefore, in this study, we conducted time series analyses to investigate hospital utilization trends in patients with schizophrenia and other psychotic disorders over the past 10 years, and to predict the likely trends for the next 3 years.
METHODS
Data sources and study population
We collected the monthly numbers of patients who received outpatient treatment and were admitted to hospital, at least once a month between January 2010 and December 2019, with primary diagnosis codes of schizophrenia (F20), schizotypal disorder (F21), delusional disorders (F22), acute and transient psychotic disorders (F23), schizoaffective disorder (F25), or other or unspecified nonorganic psychosis (F28 and F29), using the Health Insurance Review and Assessment Service (HIRA) database provided by the Health Insurance Big Data Open System [17]. The numbers of outpatients and inpatients were calculated based on the date of visit and first day of hospitalization, respectively [17]. We also obtained the monthly numbers of patients aged ≤29, 30–49, 50–69, and ≥70 years who received outpatient and inpatient treatment during the same period. This study included only patients covered by the National Health Insurance Service, and not those who were uninsured or receiving Medical Aid. This study was reviewed and approved by the Institutional Review Board of Chonnam National University Hospital (IRB number: CNUH-EXP-2021-047).
Time series analysis
We used Facebook Prophet, a time series forecasting additive model that fits non-linear trends considering seasonality and holiday effects [18]. As a forecasting model, Prophet is as sophisticated as the autoregressive integrated moving average (ARIMA) model, which the most widely used forecasting model [19]. The details of the time series analysis conducted in this study are as follows. First, we constructed a forecasting model from 120 months of data using the ‘prophet’ function, and incorporated multiplicative seasonality. The holiday effects of Korean New Year’s Day and Korean Thanksgiving was also modeled with extra regressors. Change-points where the monthly numbers of patients had abrupt changes in their trajectories were automatically selected. Next, the prediction was conducted (36-month forecasting period) using the ‘prediction’ function. Then, we visualized the predicted values with 80% uncertainty intervals for 2020–2022, together with the actual values up to 2019. Then, we visualized the predicted values with 80% uncertainty intervals for 2020–2022, together with the actual values up to 2019. All analyses were conducted using R (version 3.6.1; R Development Core Team, Vienna, Austria).
RESULTS
Current and future trends in hospital utilization
Figure 1 shows the trends in the numbers of patients with schizophrenia and other psychotic disorders receiving treatment per month over the past decade, and the prospective trends for 2020 and beyond. The number of patients receiving outpatient treatment has steadily increased and reached about 85,000 per month, although the rate of increase has slowed slightly since around 2016 (Figure 1A). The increase in the monthly number of outpatients is expected to continue for some time after 2020. However, the number of patients admitted to hospital per month peaked at about 13,000 per month in 2015, and then gradually declined, and is expected to decrease to less than the 2010 level of about 11,000 per month by 2022 (Figure 1B). Up to 2015, the total number of patients receiving treatment per month increased rapidly, but since around 2016, the increase has slowed and has recently stabilized at about 95,000 (Figure 1C). The forecasting model predicts that the total number of patients per month will remain at a similar level in the next few years after 2020.

Current and future trends in the numbers of patients with schizophrenia and other psychotic disorders receiving outpatient and inpatient treatment per month. The dots represent the actual numbers of patients and the red dashed line indicates the trend. The blue line with the uncertainty interval indicates the predicted numbers of patients. The red and blue vertical dotted lines represent automatically selected change-points and the date of enactment of the Mental Health and Welfare Law in 2017, respectively. A: Total patients. B: Outpatients. C: Inpatients.
Current and future trends in hospital utilization by age groups
Figure 2 shows the trends in the numbers of patients receiving treatment per month by age group. The monthly number of patients aged ≤29 years started to slowly increase from 2015, and is expected to increase steadily over the next few years. However, the number of patients aged 30–49 years has decreased rapidly since 2014–2015, and fell to <40,000 per month in 2019. The numbers of patients aged 50–69 and ≥70 years have increased rapidly since 2010. The number of patients aged 50– 69 years is expected to exceed that of patients 30–49 years, and to become the largest age group after 2022.
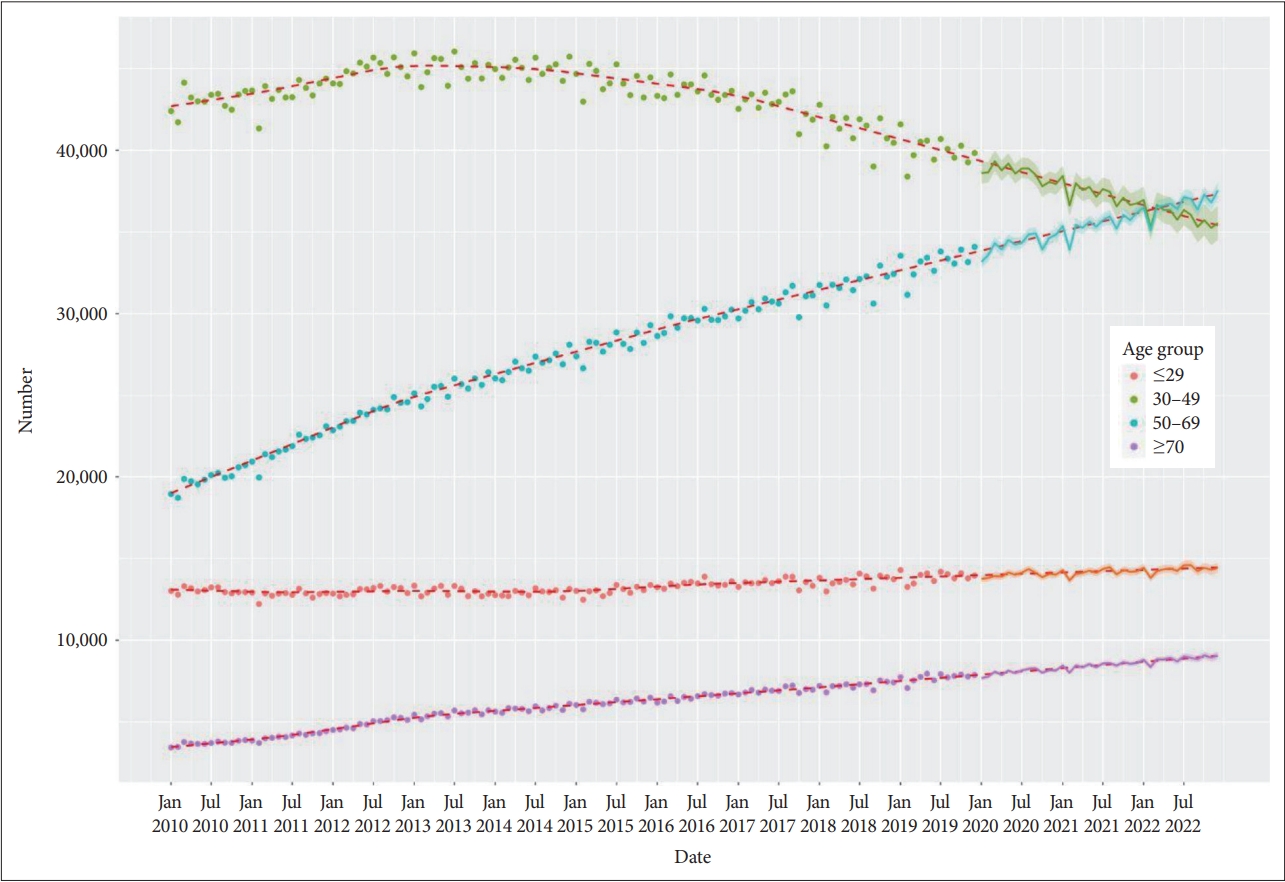
Current and future trends in the numbers of patients with schizophrenia and other psychotic disorders receiving treatment per month by age group. The dots represent the actual numbers of patients and the red dashed line indicates the trend. The line with uncertainty interval indicates predicted numbers of patients.
DISCUSSION
This study performed a time series analysis of the National Health Insurance claims data to understand monthly patterns of hospital utilization by patients with schizophrenia and other psychotic disorders in Korea. We found that hospital utilization trends began to change around 2015. Since then, the number of patients admitted to hospital each month has declined rapidly. In addition, hospital utilization has been decreasing in patients in their 30s and 40s, while it has been increasing in younger and older patients. Overall, the upward trend in hospital utilization of patients with schizophrenia and other psychotic disorders has slowed significantly in recent years. Our forecasting model predicts that these trends will continue over the next few years.
This study showed that the number of patients admitted to hospital per month with schizophrenia and other psychotic disorders began to decline around 2015 (Figure 1B). Given that the number of hospitalized patients receiving Medical Aid support has remained unchanged in recent years (39,628, 39,452, and 39,183 in 2017–19, respectively) [20-22], the total number of hospitalizations covered by National Health Insurance or Medical Aid also seems to be decreasing. Current policies aimed at reducing the number of beds in mental hospitals in Korea, together with strengthened legislation, may further accelerate this decline [11]. In this regard, further interrupted time series analysis is warranted to investigate changes in hospitalization trends before and after the Mental Health and Welfare Law was enacted [13]. Our findings suggest that we should monitor the declining hospitalization rate closely, and prepare for possible problems caused by rapid deinstitutionalization.
We found that, despite the rapid decline in the population aged ≤29 years over the past 10 years (from 18.5 million [36.5%] in 2010 to 15.9 million [30.7%] in 2019) [23], the number of patients aged ≤29 years has been increasing steadily (Figure 2). Because early diagnosis and treatment are critical for the treatment of schizophrenia, engagement of young patients in psychiatric treatment and reduction of the duration of untreated psychosis (DUP) are important. However, the DUP tends to be relatively long and treatment delays are more common in Korea compared with Western countries [24]. Our results show steady increases in the numbers of treated patients in their 20s and under, which suggests a potential improvement in public awareness in Korea of the need for early treatment of schizophrenia [8,9]. Further studies should investigate the association between DUP and increasing hospital utilization in young patients with schizophrenia.
In this study, it was noteworthy that the numbers of patients in their 30s and 40s receiving treatment each month have declined significantly since 2014–2015 (Figure 2). The proportion of the total population of Korea in their 30s and 40s has continued to decline over the past 10 years, from 17.2 million (34.08%) in 2010 to 15.5 million (29.81%) in 2019 [23], while patients in their 30s and 40s still account for the largest proportion of patients with schizophrenia [7,25]. The decreasing rate of hospital utilization by middle-aged patients in this study can be partially explained by changes in demographics and medical insurance status. However, despite the decreasing proportion of young people, the number of patients in their 20s and under has increased steadily. The number of patients in their 30s and 40s receiving Medical Aid has also not changed significantly since 2015.7 In this regard, our findings suggest that many middle-aged patients with schizophrenia may have withdrawn from treatment in their chronic stage. Over the years, various factors have been shown to reduce treatment adherence in middle-aged patients, such as inadequate support from families and social networks; therefore, we need to pay more attention to treatment maintenance in this population.
This study found that the monthly number of elderly patients has been increasing linearly (Figure 2), and the number of patients aged 50–69 years is approaching that of patients aged 30–49 years. This finding agrees with the results of Cho et al. [25], who reported increasing annual incidence rates of schizophrenia and schizophrenia-related disorders in patients aged >65 years between 2010 and 2015. This increase in the number of elderly patients may be attributed to the aging of the general population in Korea: the proportion of people in their 50s and 60s increased from 11.3 million (22.3%) in 2010 to 14.9 million (28.9%) in 2019, and that of people in their 70s and above increased from 3.6 million (7.1%) in 2010 to 5.5 million (10.6%) in 2019 [23]. Some elderly patients were diagnosed with schizophrenia when they were young, but many may be newly diagnosed with psychotic disorders secondary to dementia or alcohol use disorder [26]. Our findings underscore the need to prepare for problems with housing, social isolation, physical health, and the use of antipsychotic drugs in elderly patients.
Overall, the upward trend in the numbers of patients receiving treatment each month has slowed in recent years (Figure 1C). Considering the increase in the number of young and elderly patients, the recent slowdown in the upward trend in hospital utilization may be due to the rapid decline in the number of middle-aged patients. This may also be due to the steady increase in the number of patients covered by Medical Aid rather than National Health Insurance in recent years [20-22]. Since many patients in Korea may still not be receiving adequate treatment [10], we need to investigate why the increasing trend in hospital utilization has slowed.
This study had some methodological limitations. First, it did not include patients covered by Medical Aid, the number of which is comparable to the number of patients covered by National Health Insurance. Further studies are needed to investigate hospital utilization trends in all patients with schizophrenia through time series analysis. Second, due to the wide range of diagnosis codes selected, this study may have included some patients who did not actually have schizophrenia or other psychotic disorders. Third, we calculated hospital utilization rates based only on the number of patients receiving treatment each month, rather than the number of hospital visits, which is also an important indicator of hospital utilization. Fourth, our time series models could not address the effect of changes in mental health policies on hospital utilization over time. As the next step, we plan to conduct an interrupted time series analysis to explore this. Fifth, we used only one algorithm, Prophet, in the forecasting procedure. Additional analyses are needed using other forecasting techniques, such as ARIMA, to compare and combine forecasts.
In conclusion, hospital admissions of patients with schizophrenia and other psychotic disorders have declined in Korea. In addition, hospital utilization has rapidly decreased in middle-aged patients, but increased in young and elderly patients. As a result, the upward trend over the past decade in hospital utilization of patients with schizophrenia has slowed recently. These trends are expected to persist over the next few years. Close monitoring and preparation for potential problems caused by these changing trends in hospital utilization by patients with schizophrenia is needed.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Sung-Wan Kim, Seunghyong Ryu. Data curation: Seunghyong Ryu, Hee Jung Nam. Formal analysis: Seunghyong Ryu, Hee Jung Nam. Funding acquisition: Sung-Wan Kim. Supervision: Jae-Min Kim. Visualization: Seunghyong Ryu. Writing—original draft: Sung-Wan Kim, Seunghyong Ryu. Writing—review & editing: Jae-Min Kim, SungWan Kim.
Funding Statement
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI19C0481, HC19C0316).
