Association between Suicidal Ideation and Causes of Primary Care Visits: A Cross-Sectional Study to Identify Patients with Suspected Suicidal Ideation
Article information
Abstract
Objective
Suicide victims are likely to visit a primary care provider within 1 month of the suicide attempt. However, it is impossible for primary care providers to screen all patients for suicidal ideation or attempts. We, therefore, aimed to investigate potential differences in the chief diagnoses received by primary care patients with and without suicidal ideation, as this information may provide clues and predict patients at risk of suicide.
Methods
This cross-sectional study included 1,211 Korean adults aged ≥20 years who had participated in the Korea National Health and Nutrition Examination Survey during 2014 and provided information about their histories of suicidal ideation and visits to primary care providers. Multiple logistic regression analyses were used to examine whether suicidal ideation was associated with specific diseases after controlling for age, sex, household income, education, occupation, marital status, smoking, alcohol consumption, and physical activity.
Results
Among primary care patients, the sample-weighted percentage of suicidal ideation was approximately 12%. The diagnoses of neoplasm and mental disorder were associated with a higher likelihood of suicidal ideation {odds ratio (OR) [95% confidence interval (CI)] 8.32 (1.01–68.56) and 6.19 (1.72–22.33), respectively}. Notably, diseases of the musculoskeletal system and connective tissue were also associated with suicidal ideation [OR (95% CI): 1.93 (1.09–3.43)].
Conclusion
The observed visit patterns and correlations of certain diagnoses with suicidal ideation suggest that primary care physicians should pay attention to patients with relevant disorders, consider screening suicidal ideation, and properly consult to a psychiatrist.
INTRODUCTION
Suicide is a critical global public health issue [1], particularly in the Republic of Korea where the prevalence of suicide is among the highest worldwide. According to a report from the Korea Suicide Prevention Center, the national prevalence of suicide increased steadily from 16.6 to 33.5 per 100,000 people during 2009–2010 and decreased slightly thereafter to 26.6 per 100,000 people in 2018 [2]. In contrast, the average prevalence of suicide among Organization for Economic Cooperation and Development (OECD) countries were 11.5 per 100,000 people in 2017 [2]. This discrepancy highlights the status of suicide as a public health crisis in Korea.
The high suicide mortality patterns have elicited a range of preventive strategies worldwide. Several previous reports have stressed comprehensive and integrated multidisciplinary approaches for the reduction of suicide and suicidal behaviour [3-6], among which gatekeeper training is regarded one of the most effective strategies. Gatekeepers are individuals who come into frequent contact with members of the community; this category includes primary, mental, and emergency health care providers; teachers and other school staff; community leaders and police officers; and other first responders [3]. Some studies have reported that approximately 45% of suicide victims had contact with a primary care provider within 1 month of the suicide attempt [7], suggesting that primary care providers could play a prominent role in suicide prevention [8]. However, it would be impossible for primary care physicians to screen all visiting patients for suicidal ideation or attempts, as the general population is not considered a high-risk group. The U.S. Preventive Services Task Force (USPSTF) also concluded that “the current evidence is insufficient to assess the balance of benefits and harms of screening for suicide risk in adolescents, adults, and older adults in primary care [9].” In summary, the prevention of suicide would rely on the identification of patients who are likely to commit suicide.
The Korean National Health and Nutrition Examination Survey (KNHANES) includes data about suicidal ideation, primary care visit history, and information about diagnoses made during the most recent 2-week period. These data could form the basis of an investigation of differences in the chief complaints and diagnoses of primary care patients with and without suicidal ideation. The results of such an investigation could subsequently facilitate the prediction of patients at risk of committing suicide. Therefore, this study aimed to determine the association between suicidal ideation and the primary care visit history, using data from the KNHANES in 2014.
METHODS
Study participants
This study was conducted according to the guidelines set forth in the Declaration of Helsinki. All procedures involving human subjects were approved by the Institutional Review Board of the Korea Centers for Disease Control and Prevention (2013-12EXP-03-5C). Written informed consent was obtained from all subjects.
This cross-sectional study used data from the KNHANES, a nationwide survey of non-institutionalized civilian residents of South Korea that has been conducted by the Korean Ministry of Health and Welfare since 1998. Briefly, this nationwide representative study uses a stratified, multistage probability sampling design to select household units [10]. The KNHANES aims to evaluate the nutritional and health status of the general population and subsequently provide representative and reliable statistical public health data that can be used as a basis for health care policies.
This analysis was based on data obtained from 5,428 respondents to the 2014 survey who were aged ≥20 years. From this initial population, we excluded the following individuals for the following reasons: no information about outpatient visits during the most recent 2-week period (n=3,670); no visits to a primary care center (n=536); and missing data for the ninth question on the Patient Health Questionnaire (PHQ-9; n=11). This study included 1,211 Korean adults.
Study variables
The PHQ-9 is a reliable and valid screening tool used widely to detect depressive disorders, including suicidal ideation, in the general population [11]. The Korean version of the PHQ-9, which is also considered reliable and valid, was included in the KNHANES VI-2 survey [12]. In this study, we defined a participant as having suicidal ideation if they provided a positive response (i.e., “yes”) to the ninth item on the PHQ-9, which asked “Have you ever thought that you would be better off dead or of hurting yourself in the most recent 2 weeks?”
Diseases that served as the causes for visits to primary care providers were identified via diagnostic information and had been recorded by physicians according to the Tenth International Classification of Diseases (ICD-10). The following codes and classifications were applied: A00–B99, Certain infectious and parasitic diseases; C00–C97, Neoplasms; E00–E90, Endocrine, nutritional, and metabolic diseases; F00–F99, Mental and behavioral disorders; G00–G99, Diseases of the nervous system; H00–H59, Diseases of the eye and adnexa; H60– H95, Diseases of the ear and mastoid process; I00–I99, Diseases of the circulatory system; J00–J99, Diseases of the respiratory system; K00–K93, Diseases of the digestive system; L00–L99, Diseases of the skin and subcutaneous tissue; M00–M99, Diseases of the musculoskeletal system and connective tissue; N00–N99, Diseases of the genitourinary system; O00–O99, Pregnancy, childbirth, and the puerperium; R00–R99, Symptoms, signs, and abnormal clinical and laboratory findings, not elsewhere classified; S00–T98, Injury, poisoning, and certain other consequences of external causes; and Z00–Z99, Factors influencing health status and contact with health services. We also identified self-reported underlying diseases, including hypertension, diabetes mellitus, dyslipidemia, stroke, cardiovascular disease (angina or myocardial infarction), depression, and cancer diagnosed by a medical doctor.
The potential confounders included age, sex, residence, household income, education, marital status, body mass index (BMI), smoking status, alcohol consumption, and physical activity. The residence was classified as urban or rural. Household income was classified into quartiles. Education status was classified into two categories: high school or lower and college or higher. Occupations were classified as follows: manager, professional, or office worker; service or sales; manual worker; and unemployed (e.g., housewife or student). The cohabitation status was classified as either living alone or living together. BMI was derived from the measured weight and height and reported in units of kg/m2. Obesity was defined as a BMI of ≥25 kg/m2 according to the current Asian obesity guidelines [13]. A current smoker was defined as someone who had smoked ≥100 cigarettes (5 packs) throughout his or her lifetime and continued to smoke at the time of the survey. A heavy drinker was defined as a person who consumed at least one bottle of soju (Korean distilled spirits) during a 1-week period. Regular physical activity was defined as participation in vigorous activity (e.g., running or mountaineering) for ≥75 min/week or moderately intense activity (e.g., light swimming, badminton, or walking) for ≥150 min/week [14]. Strength exercise was defined as the performance of exercise at least twice a week.
Statistical analysis
The survey procedures in SAS 9.2 (SAS Institute Inc., Cary, NC, USA) were applied to complex sampling designs. The characteristics of the study population are reported as means±standard errors (SEs) for continuous variables and as weighted percentages (%) with SEs for categorical variables. We categorized participants into two groups according to suicidal ideation, using the ninth item of the PHQ-9. Differences in ICD10 codes among the two groups were analyzed using a weighted t-test and chi-square test. Multiple logistic regression analyses were used to examine the potential associations of suicidal ideation with specific diseases after controlling for age, household income, education, occupation, marital status, smoking, alcohol consumption, and physical activity. Statistical significance was set at a two-sided p-value <0.05.
RESULT
Table 1 presents the general characteristics of the study population, stratified by suicidal ideation. The sample-weighted frequency of suicidal ideation among primary care patients was 11.8%. Patients who expressed suicidal ideation were more likely to be female, have low income and education levels, live alone, be unemployed, and be less likely to perform strength exercise. Table 2 presents information about disease diagnoses made by primary care providers during the 2-week period before the survey according to ICD-10 codes and self-reported underlying diseases, according to the suicidal ideation status. Of the ICD-10 coded diseases, mental and behavioral disorders (F00–F99) and diseases of the musculoskeletal system and connective tissue (M00–M99) were significantly more frequent among individuals with suicidal ideation. Among self-reported underlying diseases, hypertension, stroke, and depression were significantly more frequent among individuals with suicidal ideation.

Diseases diagnosed by primary care providers and the self-reported underlying disease among participants per suicidal ideation (N=1,211)
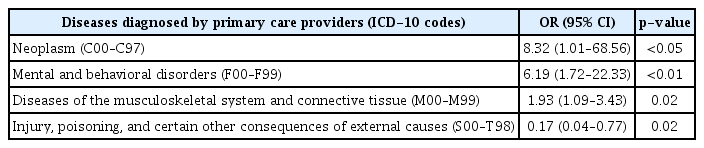
Table 3 presents the significant multivariable-adjusted odds ratios (ORs) with 95% confidence intervals (CIs) of ICD-10 coded diseases and suicidal ideation. Notably, diagnoses of neoplasm (C00–C97) and mental disorder (F00–F99) were associated with the greatest increases in the probability of suicidal ideation [OR (95% CI): 8.32 (1.01–68.56) and 6.19 (1.72–22.33), respectively], although diseases of the musculoskeletal system and connective tissue (M00–M99) were also associated with suicidal ideation [OR (95% CI): 1.93 (1.09–3.43)]. Conversely, injury, poisoning, and certain other consequences of external causes (S00–T98) were associated with a lack of suicidal ideation [OR (95% CI): 0.17 (10.04–0.77)]. We further calculated the frequency of visits to primary care providers during the most recent 2-week period. In an analysis stratified by ICD-10 codes assigned by primary care providers, injury, poisoning, and certain other consequences of external causes were significantly more frequent among individuals without suicidal ideation (p<0.01). No significant associations were observed between other diseases diagnosed by primary care providers and the presence of suicidal ideation.
DISCUSSION
In this cross-sectional study of data from the KNHANES, we identified that approximately 12% of primary care patients reported suicidal ideation. This rate was higher than the range of 1.0–7.3% reported by a review of suicidal ideation among primary care patients in the U.S. [15], and similar to the rates from German primary care studies in which the PHQ was used to assess suicidal ideation [16]. According to another Korean study surveying patients visiting selected 15 primary care facilities in Seoul and Gyeonggi-do Provinces, approximately 18% of those reported suicidal ideation [17], which was higher than those of this representative study due to the difference of the living area and age distribution of the population. These figures are higher than those of the Korean general population, which was approximately 6% in the 2013–2014 KNHANES, calculated using the question, “Have you ever seriously considered suicide in the last year? [18].”
The primary care patients with suicidal ideation in this study were more likely to be female, have a lower income and education level, live alone, and be unemployed, consistent with multiple reports describing risk factors for suicidal ideation [19-21]. We further investigated potential differences in the chief primary care diagnoses of patients with and without suicidal ideation and found that the former were more likely to receive diagnoses of neoplasms (C00–C97), mental and/or behavioral disorders (F00–F99), and diseases of the musculoskeletal system and connective tissue (M00–M99), while the latter were more likely to be diagnosed with an injury, poisoning, and certain other consequences of external causes (S00–T98).
Previous studies have reported that primary care patients with suicidal ideation were more frequently diagnosed with depression [22] and anxiety disorders [23], compared to those without suicidal ideation. Consistent with those findings, we observed a higher frequency of diagnosed mental and behavioral disorders (F00–F99) among patients with suicidal ideation. This finding is highly plausible, as a previous systematic review of psychological autopsy studies on suicide reported that >60% of suicidal deaths involved victims who had experienced a major depressive disorder or other mood disorders [24]. Moreover, patients with neoplasms (C00–C97) have a high risk of psychological problems [25], consistent with our findings.
Additionally, we identified diseases of the musculoskeletal system and connective tissue (M00–M99) as primary causes of visits to primary care providers among individuals with suicidal ideation. Although the paucity of studies evaluated the association between musculoskeletal disorders and suicidal ideation, a review of the psychological risk factors associated with back and neck pain reported that these factors play an important role not only in chronic pain but also in the etiology of acute pain, particularly during the transition to chronic problems [26]. Of musculoskeletal diseases, fibromyalgia, characterized by chronic, widespread musculoskeletal pain [27], is linked to depression and anxiety; indeed some authors have argued about the possibility to classify this syndrome into affective spectrum disorder [28]. Accordingly, patients with physical pain due to musculoskeletal disorders may experience depressive symptoms, which would explain the observed significant association with suicidal ideation.
Our analysis revealed that injury, poisoning, and certain other consequences of external causes were diagnosed more frequently in patients without suicidal ideation. On the other hands, one previous study based on a Korean national health insurance database reported that patients who visited a medical facility for injury, poisoning, and certain other consequences of external causes (S00–T98) had a significantly increased risk of suicide death [29]. This difference could be explained that severity of injury between primary care and emergency center. In the earlier study, disease information was solicited from all types of medical facilities, including psychiatric departments and emergency departments. In this study, however, we investigated only disease information from primary care patients with suicidal ideation, rather than suicidal death. Possibly, patients with injuries related to suicide attempts visited the emergency departments of general hospitals more frequently due to the severity of their conditions.
Currently, Korea reports the highest national frequency of physician visits worldwide. According to a 2017 OECD Health Statistics analysis, Korea reported the highest number of outpatient visits to physicians per capita among all OECD countries, with a rate of 16.0 per year in 2015 vs. the OECD average of 7.0 per year [30]. Given that the frequent clinical visits made by Korean patients and the finding that patients with specific diseases face a higher risk of suicidal ideation support the suggestion that Korean physicians should screen high-risk patients for suicidal ideation. Accordingly, we recommend that primary physician should consider undergoing screening for suicidal ideation, when patients with low income (checking insurance information), living alone, or unemployed complain the symptom including mental or musculoskeletal disorders should consider undergoing screening for suicidal ideation.
This study had some limitations. First, the cross-sectional design did not allow us to confirm the events that occurred between suicidal ideation and visits to primary care providers within the 2-week period prior to the survey. Second, the assessment of suicidal ideation was based only on the PHQ-9. Therefore, we may have underestimated the frequency of suicidal ideation and could not evaluate suicidal plans or attempts. Third, the ICD-10 codes were based on the history of self-reported visits to primary care providers. Therefore, further research is needed to evaluate these associations in greater detail. Despite these limitations, our study was the first to examine the association of suicidal ideation with musculoskeletal diseases and mental disorders in a nationally representative sample of primary care patients in the country with the highest suicide rate worldwide.
In conclusion, the observed visit patterns and correlations of certain diagnoses with suicidal ideation suggest that primary care physicians should pay attention to patients with relevant disorders, consider screening suicidal ideation, and properly consult to a psychiatrist.
Acknowledgements
None.
Notes
The authors have no potential conflicts of interest to disclose.
Author contribution
Conceptualization: Gyeongsil Lee, Jung-Ha Kim. Data curation: Gyeongsil Lee, Jung-Ha Kim. Formal analysis: Gyeongsil Lee, Jung-Ha Kim. Investigation: Gyeongsil Lee. Methodology: Jung-Ha Kim. Project administration: Jung-Ha Kim. Resources: Jung-Ha Kim. Software: Jung-Ha Kim. Supervision: Jung-Ha Kim. Validation: Jung-Ha Kim. Writing—original draft: Gyeongsil Lee. Writing—review & editing: Gyeongsil Lee, Jung-Ha Kim.