Risk Factors for Suicidal Ideation among Patients with Complex Regional Pain Syndrome
Article information
Abstract
Objective
Chronic pain frequently coexists with psychiatric symptoms in patients diagnosed with complex regional pain syndrome (CRPS). Previous studies have shown a relationship between CRPS and the risk of suicide. The purpose of this study was to assess risk factors for suicidal ideation in patients with CRPS.
Methods
Based on criteria established by the International Association for the Study of Pain, 39 patients diagnosed with CRPS Type 1 or Type 2 were enrolled in this study. Suicidal ideation was assessed using item 3 of the Hamilton Depression Rating Scale (HAMD), and symptoms of pain were evaluated using the short form of the McGill Pain Questionnaire (SF-MPQ). Psychiatric symptoms were assessed in using the Structured Clinical Interview for DSM-IV Disorders (SCID-I, SCID-II), the HAMD, the Hamilton Anxiety Rating Scale (HAMA), the Global Assessment of Functioning Scale (GAF), and the Pittsburgh Sleep Quality Index (PSQI).
Results
Twenty-nine patients (74.4%) were at high risk and 10 (25.6%) were at low risk for suicidal ideation. Risk factors significantly associated with suicidal ideation included depression (p=0.002), severity of pain (p=0.024), and low scores on the GAF (p=0.027). No significant correlations were found between suicidal ideation and anxiety or quality of sleep.
Conclusion
Significant risk factors for suicidal ideation in patients with CRPS include severity of pain, depressive symptoms, and decreased functioning. These results suggest that psychiatric evaluation and intervention should be included in the treatment of CRPS.
INTRODUCTION
Pain is associated with higher risk of suicide.1-3 In a recent review, Tong et al.1 reported that the lifetime prevalence of suicidal ideation (SI) and suicide attempts for patients with chronic pain were 5-14% and 20%, respectively. Edwards et al.3 found that more than 30% of subjects suffering from chronic pain reported some form of recent suicidal ideation. Large population-based studies have shown an association between various types of chronic pain conditions (e.g., migraine headaches, back pain, arthritis, fibromyalgia) and suicide risk, even with adjustment for mental disorders.4
Although it may be difficult to determine whether a mental disorder is a preexisting condition or is subsequent to chronic pain, comorbidity significantly increases the risk of suicide.2 Findings have shown that depression is the most common comorbid symptom, and studies indicate that 31-100% of patients with chronic pain suffer from depression.5 Moreover, Kroenke et al.6 reported that changes in the severity of pain predicted changes in the severity of depressive symptoms experienced by patients with chronic pain and vice versa. Symptoms of anxiety are similarly common in the medical profiles of patients with chronic pain. In a population-based study, the prevalence of anxiety disorders was 35% in persons with chronic pain compared with 18% in the general population.7 However, it is important to note that these studies used data collected primarily from patients with musculoskeletal and other relatively common neuropathic pain-related conditions (i.e., patients with pain associated with migraine headaches, arthritis, back pain, fibromyalgia, etc.).
Complex regional pain syndrome (CRPS) is a medical condition whose primary symptom is chronic distressing pain and it has been subdivided into type I (reflex sympathetic dystrophy) and type II (causalgia).8 CRPS may involve pain that is localized to an extremity (the arm, hand, leg, or foot) or pain that affects multiple parts of the body. Localized pain affecting a limb is often accompanied by impairment in the functioning of that extremity and the possibility of ongoing pain and severe disability.9 Although the mechanism underpinning CRPS remains unknown, investigators have proposed various hypotheses, including that CRPS is a systemic disease involving the central nervous system (CNS) and the peripheral nervous system (i.e., neuropathic) and associated interactions between the immune system and sensitive nociceptive nervous system transmission.10,11
Although CRPS has properties similar to those of other conditions involving peripheral neuropathy, it also has several distinct characteristics. For example, the subjective experience of pain in CRPS is accompanied by sudomotor and vasomotor dysfunction (i.e., changes in skin color and/or temperature).12 CRPS is viewed as among the most painful of all known diseases, with patients' scores on the McGill Pain Questionnaire (mean MPQ score of 42 of a possible 50) being among the highest of any diagnostic group, surpassing even the scores of patients who have experienced amputation of a limb or childbirth.13,14
It is prudent for clinicians to include a thorough suicide risk assessment in medical examinations of patients with CRPS given their apparent vulnerability due to functional impairments and severe pain and to the possibility of psychiatric symptoms associated with depression and other psychological diagnoses. Lohnberg's review12 of the relationship between CRPS and psychological and psychosocial factors found that CRPS was associated with depression, anxiety, reduced quality of life, and impaired occupational functioning. Additionally, a web-based epidemiological survey with CRPS-1 patients estimated that 20% had attempted suicide, and 46.4% reported experiencing suicidal ideation.15 However, few data about psychological comorbidity with respect to suicide risk factors in CRPS patients are available.
The primary aim of this study was to identify clinical factors related to suicidal ideation in patients with CRPS. Secondarily, we evaluated psychiatric comorbidity in this population. Results indicated an association between suicidal ideation and various psychiatric symptoms. We hypothesized that lifetime comorbid psychiatric symptomatology would increase the risk for suicidal ideation among individuals with CRPS.
METHODS
Participants
The subjects were outpatients at the Pain Clinic of Seoul National University Hospital. Patients included in the study met the following criteria: 1) aged 18 years or older; 2) presentation with CRPS symptoms; and 3) voluntary provision of informed consent for participation in the study. Exclusion criteria consisted of 1) younger than 18 years of age, 2) fewer than 6 months of CRPS treatment, 3) a medical history of neurological disease, 4) a history of substance abuse, and 5) previous treatment for any type of neuropsychiatric condition.
After obtaining approval to conduct the study from the Institutional Review Board, the procedures used in the study were fully explained to all subjects, who then provided informed consent to participate. The patient subjects were evaluated by physicians to confirm the presence of CRPS as defined by the International Association for the Study of Pain (IASP). Each subject was subsequently assessed by neuropsychiatric specialists who were blind to each patient's clinical profile to determine the presence and nature of any psychiatric symptoms.
Measurements
Structured Clinical Interview for the DSM IV-I, II
The Structured Clinical Interview for DSM-IV Disorders (SCID) is a diagnostic tool used to identify DSM-IV Axis I16 and Axis II disorders (major mental disorders and personality disorders, respectively).17 The instrument was designed to be administered by a clinician or trained mental health professional. The Korean version was used in this study.
Psychiatric symptoms
Psychiatric characteristics were assessed with Hamilton Rating Scale for Depression (HAMD)18 and the Hamilton Rating Scale for Anxiety (HAMA).19 The HAMD is a multiple-choice questionnaire that clinicians use to rate the severity of a patient's depression. A score of 0-7 is considered to be normal, and scores of 20 or more indicate moderately severe depression. For a comparison of depressive symptoms, we summed the HAMD items with the exception of item 3 (the suicide-risk item), which we excluded to avoid biasing the relationship between depression severity and suicide risk. The Hamilton Anxiety Rating Scale (HAMA) is a questionnaire used by clinicians to rate the severity of a patient's anxiety. It contains 14 symptom-oriented questions. Each of these symptoms is given a severity rating ranging from not present (0) to very severe (4). Total scores of 0-17 are considered to indicate mild anxiety, those 18-25 mild to moderate anxiety, and those 26-30 moderate to severe anxiety. Subjects were also rated on the Global Assessment of Functioning (GAF) Scale, which is based on Axis V of the Diagnostic and Statistical Manual of Mental Disorders,20 to assess psychological, social, and occupational functioning. Scores range from 1-100, with higher scores reflecting better functioning.
Suicidal ideation
The low-suicidal ideation (SI) group included those with scores of 1 or below on HAMD item 3 (0=suicide ideation absent, 1=feels that life is worth living), and the high-SI group included those with HAMD item 3 scores above 1 (2=wishes he were dead or any thoughts of possible death to self; 3=suicidal ideas or gesture; 4=attempts at suicide). This cutoff value has been commonly used in previous studies.21-23
Pittsburgh Sleep Quality Index
The PSQI24 is a self-administered questionnaire that assesses subjective sleep quality during the previous month. The self-rated items on the PSQI generate seven component scores (range of subscale scores, 0-3): sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbance, use of sleeping medication, and daytime dysfunction. The sum of these seven component scores yields one global score for subjective sleep quality (range, 0-21); higher scores represent po-orer subjective sleep quality, and those >5 are associated with poor sleep quality.
Short form of the McGill Pain Questionnaire
The short form of the McGill Pain Questionnaire (MPQ-SF)25 was used as an index of pain severity. Five scores are derived from the SF-MPQ; the Sensory Pain Rating Index (S-PRI), the Affective Pain Rating Index (A-PRI), the Total Pain Rating Index (T-PRI), the Present Pain Intensity-Visual Analogue Scale (PPI-MPQ-VAS), and the overall intensity of total pain. In this study, a visual analogue scale (MPQ-VAS) was used to assess pain severity. MPQ-VAS is a visual analogue scale that uses a 10-cm line divided into 1-cm sections. Patients indicate their level of pain by marking the appropriate place on the scale from 0 (no pain) to 10 (the worst possible pain).26
Statistical analysis
Between-group comparisons involving categorical data were performed using the chi-square statistic corrected for continuity; between-group comparisons involving continuous data (age and socio-economic status) were calculated using Student's t-test. Pearson's correlation analysis was used to assess correlations between suicidal ideation and other variables.
RESULTS
Demographic variables
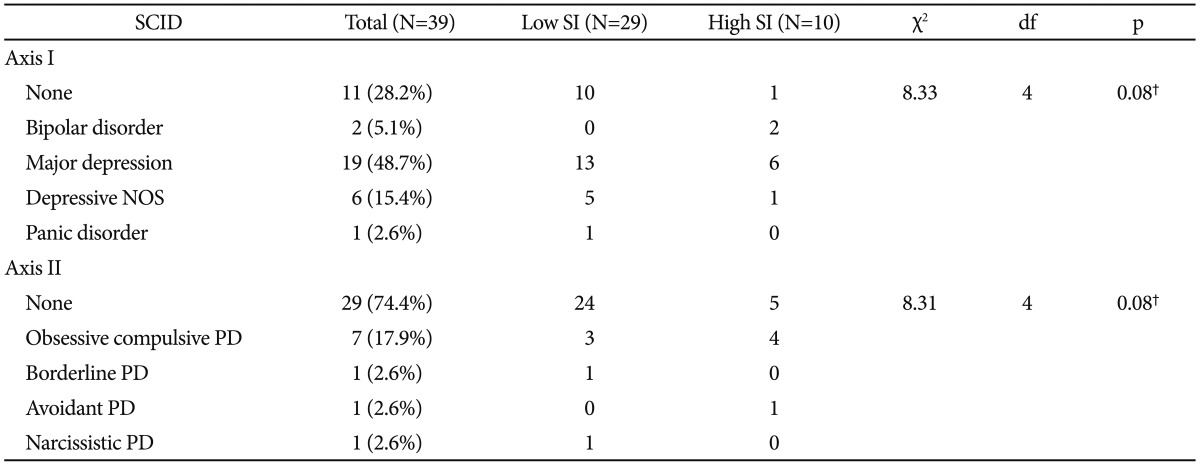
The sample included 39 patients with CRPS; 33 (84.6%) were diagnosed with CRPS Type 1, and six (15.4%) were diagnosed with CRPS Type II. Males accounted for 61.5% (n=24) of the patients, and females 38.5% (n=15). The mean age of the patients at their initial evaluation at the pain clinic was 37.87 (±11.94) years, and the mean number of years of education was 12.49 (±2.68) years. Patients reported having CRPS symptoms for a mean of 2.84 years (±2.49) at the time of evaluation and had been prescribed 4.28 (range, 0-7) different kinds of medications on average. The most frequently used medications were anticonvulsants and antidepressants. We found no significant differences between the two groups in terms of demographic characteristics and medications (Table 1). The most common psychiatric comorbidity according to the SCID was depression. Among those with depression, 19 (48.7%) met the criteria for major depressive disorder, and 6 patients (15.4%) were diagnosed with depressive disorder NOS. Two patients (5.1%) met the criteria for bipolar II disorder, and one patient met the criteria for panic disorder. In terms of Axis II, seven patients (17.9%) met the criteria for obsessive-compulsive personality disorder, and one each met the criteria for borderline personality disorder, avoidant personality disorder, and narcissistic personality disorder. Eight (18.2%) subjects were not diagnosed with any comorbid psychiatric disorders by the SCID-I or II. No significant differences were found between the two groups in SCID results (Table 2).
Clinical characteristics of patients with CRPS: low and moderate-to-high SI
Figure 1 presents the differences between low-SI and high-SI groups in terms of psychiatric symptoms and other variables. Twenty-nine patients (74.4%) were placed in the high-SI group, and 10 (25.6%) were placed in the low-SI group.
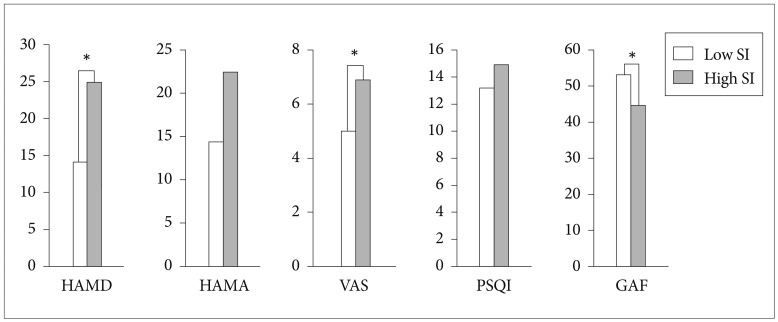
Comparison of symptoms profiles for patients with CRPS between high SI and low SI. *p<0.05. HAMD: Korean version of the Hamilton Depression Rating Scale, HAMA: Korean version of the Hamilton Anxiety Rating Scale, VAS (MPQ-SF): Visual Analogue Scale, PSQI (Total): Pittsburgh Sleep Quality Index, GAF: Global Assessment of Functioning, SI: suicidal ideation.
Anxiety was not a significant predictor of suicide risk, but depressive symptoms were. The HAMD average score of high-SI group (25.00±6.94 SD) was significantly higher than that of the low-SI group (14.03±9.49; F=1.67, t=-3.35, df=37, p=0.002).
The average pain intensity for each year after symptom onset was 5.50 (SD=2.3). The high-SI group reported greater pain intensity (6.90±2.81) than did the low-SI group (5.02±1.93; t=-2.36, df=37, p=0.02). The low-SI group also had significantly higher GAF scores (53.38±14.56) than did the high-SI group (44.90±7.68; t=2.33, df=30.2, p=0.03). No differences were found with regard to sleep quality, but the majority of patients reported poor sleep quality (13.64±4.22). Significant correlations were found between suicidal ideation and HAMD (r=0.72, p=0.00), HAMA (r=0.58, p=0.00), PSQI (r=0.43, p<0.01), and GAF (r=-0.56, p=0.00) scores.
DISCUSSION
This cross-sectional study gathered data about patients with CRPS who had no previous psychiatric symptoms using neuropsychiatric scales administered by a psychiatric specialist at a tertiary university-based pain center. To the best of our knowledge, this is the first study to assess predictors of suicide risk in patients with CRPS. The strengths of this study include its use of a structured interview (SCID) to diagnose mental disorders.
In terms of mental health-related variables, although we found no significant differences in the SCID results for the two groups, the HAMD scores were significantly higher in the high-SI than in the low-SI group, and we found a positive correlation between suicidal ideation and depressive symptoms. Little research has assessed the causal relationship between suicidal ideation and depression in patients with CRPS, but several studies on chronic pain have revealed that the presence of pain may hinder the detection and treatment of depression, and patients in pain are in a high risk for suicide.27-29 Surveys of patients with fibromyalgia have reported that depression is positively correlated with suicide risk30 and that depressed chronic pain patients who were experiencing suicidal ideation were twice as likely compared with non-depressed patients to have attempted suicide at least once before the study.1,31 Additionally, Edwards et al.3 reported that depression was the most consistent predictor of the presence and degree of suicidal ideation in patients with chronic pain. This result suggests that the significant risk factor is not the diagnosis of depression per se but the severity of depressive symptoms and their aggravation at a particular point in time. In our study, no differences were found between the groups group in SCID results; only depressive symptoms were significantly different. Therefore, clinicians should consider performing or ordering a psychiatric evaluation when patients with CRPS show depressive symptoms or suicidal ideation.
Pain severity strongly distinguished the high-SI from the low-SI group and was significantly correlated with suicidal ideation. Previous studies have suggested that persistent pain is associated with elevated rates of suicide-related behaviors. Ratcliffe et al.2 reported that the presence of chronic pain was uniquely associated with suicidal ideation and suicidal attempts after adjusting for common mental disorders and comorbidity, and several studies have reported a positive relationship between pain severity and suicidal ideation.3,32 These results suggest the importance of assessing suicide risk in patients with painful conditions, even in the absence of comorbid mental disorders.
We did not control for the interaction between pain and depression in our analysis of the predictive value of the factors under examination. However, several studies have shown a causal association between depression and pain in patients with CRPS. Kroenke et al.6 showed that pain and depression have strong and similar effects on each another over the course of 12 months and suggested a bidirectional and potentially causal relationship between pain and depression. Additionally, McDaniel33 reported three cases in which electroconvulsive treatment (ECT) was administered to patients with CRPS and depressive mood, and the results showed that the treatments improved both the depression and the pain symptoms. Considering that the severity of CRPS is the highest level among pain disorders,34 patient with CRPS would show significantly higher level of depression. Our results indicate that depression is the most common psychological symptom among those with CPRS. Approximately 70% of patients with this condition qualified for a diagnosis of depressive disorder according to the SCID, and more than 80% patients had been treated with antidepressants. We could not identify whether the treatment of depressive disorders led directly to improvement in pain symptoms, but it has been reported that pain severity is significantly correlated with depressive mood and that these are both associated with suicide risk.27,31,35 Therefore it is important to assess comorbid depressive symptoms starting at the first visit to prevent worsening of pain symptoms and suicidal ideation.
No difference was found between the high- and low-SI groups in terms of anxiety. This result is similar to those of other studies that reported that symptoms of anxiety were relatively less significant predictors of SI severity compared with depression.3 However, as with depressive symptoms, several studies have suggested a relationship between anxiety and pain.36,37 One meta-analysis showed an association between anxiety sensitivity and fearful appraisals of pain in clinical and nonclinical samples.38 Additionally, Means-Christensen and colleagues found an association between pain symptoms and both depression and anxiety.39 In our study, patients with CRPS showed moderate levels of anxiety (HAMA: 16.38±12.12), and a moderate-to-large effect size was found for its association with pain (r=0.58, p=0.00). Although we did not find significant results in this regard, these studies suggest that elevated levels of anxiety are associated with the severity of pain, which may be associated with subsequent depression and suicide risk.30
The two SI groups differed significantly in their scores on the GAF, which assesses patients' 1-year psychological, social, and occupational functioning and has been accepted as stronger predictor psychiatric symptoms.40,41 Additionally, this measure has been used to evaluate the functioning of patients with chronic and acute pain.42-44 This finding suggests that patients with CRPS have significantly higher rates of maladaptive functioning, which may relate to their increased psychopathology and lower general functioning, as evidenced by their increased HAMD scores and their lower GAF scores, respectively.
Although we found no significant difference with regard to suicidal ideation, most patients (97%) reported higher than 5 in PSQI total score (mean±SD=13.64±4.22) which means poor quality of sleep and we found a significant correlation between suicidal ideation and PSQI total scores (r=0.28, p=0.00). Several previous surveys about chronic pain suggested that various etiologies significantly interfere with sleep.30,45 Most of the patients suffered from sleep difficulties after they began experiencing chronic pain, and several studies showed a positive correlation between pain intensity and degree of sleep disturbance.46 Bigatti et al.45 suggested that improving the sleep quality of fibromyalgia patients would decrease their pain and depression. These results probably do not differ from those of other pain patients, but few studies have focused on patients with CRPS only. Thus, a large multicenter prospective study is needed to validate this association between sleep quality and pain, especially in patients with CRPS.
Similar with other chronic pain conditions, biological, psychological, and social factors are important in treatment of CRPS. Previous studies reported that chronic pain brings about disability, emotional arousal which in turn aggravates pain severity.47 Various therapies such as cognitive behavioral therapy, ergonomic training physiotherapy, patient education and medication have been suggested.48,49 These psychosocial and behavioral intervention as part of multidisciplinary treatment approach also would be effective in improvement of symptoms for CRPS.
Several limitations of this study should be considered when interpreting the findings. First, because the present study is cross-sectional, these results may not be generalizable to all CRPS patients. Although longitudinal investigations are necessary to replicate these findings, this study should assist patients with CRPS who may be at risk for suicidal ideation by underscoring the importance of regular assessment and psychological treatment. Second, the sample size was relatively small, which may have resulted in a selection bias. Several epidemiologic studies have reported a female to male ratio ranging from 2:1 to 4:150,51; however, the female to male ratio in our data was 1:1.6. This may be due to the low estimated incidence of CRPS (5.46-26.2 per 100,000 person-years)50,52 and to the fact that this study was conducted at a single center, which made it difficult to recruit an adequate number of patients over a short period of time. A large multicenter research needs to be performed to validate these results. Third, several modalities identified as important treatments for pain symptoms, such as ketamine infusion and nerve blocks, were not controlled in the present study.
CRPS is recognized as one of the most difficult conditions to treat among pain syndromes. This study found that the factors most strongly associated with suicide in patients with CRPS were depression, pain severity, and general functioning. Taken together, these results should reinforce the importance of psychiatric evaluations and multidisciplinary approach in the treatment of patients with CRPS.
Acknowledgments
This study was supported by the Original Technology Research Program for Brain Science through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2012-0006587).