INTRODUCTION
Previous studies have hypothesized that psychiatric symptoms could be major symptoms of cerebellopontine-angle (CPA) lesions,1 specifically in patients with acoustic neuromas in the CPA.2-4 One report described how a focal temporal-lobe tumor expanded to the CPA and caused postoperativepsychotic symptoms.5 However, in cases where psychotic patients show few or no neurological symptoms, magnetic resonance imaging (MRI) can be an extremely useful tool for evaluating organic lesions; this is often overlooked by psychiatrists. In this paper we reported an adult patient who suddenly developed psychotic symptoms that were associated with a right CPA lesion found on MRI.
CASE
A 37-year-old, right-handed woman visited a psychiatrist after she had experienced persecutory delusions and auditory hallucinations for a month. No specific problems were revealed in the physical examination at admission. During the persecutory delusion she felt that she was being stalked and had recently been wiretapped. She also heard a man's voice that talked about her behavior, including menstruation and toilet habits. She thought that he had installed closed-circuit television around her house to watch her and followed her on the subway. These symptoms became worse, and she felt that he had invaded her privacy. She was unable to go to the bathroom or eat. When her mother visited her apartment 2 days before admission to the hospital, the windows were covered with newspapers, and the house was full of waste. She described the things that were disturbing her to her mother. She also talked to herself, asking "Why did you follow me to install the cameras?" while crying and smiling.
The patient was the younger of 2 daughters. She had a normal birth and no history of seizures. She was calm, focused, and got along well with other children. After graduating from high school, she worked at a company for 5 years. She entered music college and maintained good grades. She had moved out of her parents' house 3 years before, when they pressured her to get married. There was no family or personal history of neuropsychiatric disorders. Her premorbid personality was well tempered and introverted.
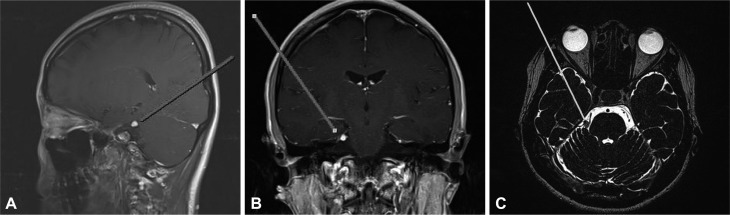
Brain MRI (Figure 1) revealed a tumor occupying the right CPA. The tumor was clinically diagnosed as a trigeminal Schwannoma. Examination by a neurosurgeon revealed few neurological problems. She exhibited auditory hallucinations, delusions of reference and persecution, and talked to herself while simultaneously crying and smiling. Mental status examination revealed alert consciousness on admission to a university hospital. She was cooperative during the interview and maintained good eye contact. She was oriented with regard to place and person. She did not show impaired memory function and answered questions with normal tone and speed. She did not show impaired cognitive functions. Although her thoughts were somewhat persecutory and included hallucinations, her thought process was relatively coherent. She was mildly anxious and her affect was blunted and appropriate. Her impulse control was moderate. Brain electroencephalogram (EEG) and a toxicology screen were performed to evaluate other organic causes, but there were no abnormal findings. Her MRI showed a small enhanced mass lesion in the right CPA region; T1-weighted images revealed a hyperintense signal (Figure 1A and B), and T2-weighted images revealed a hypointense signal (Figure 1C) within the foci. The imaging findings strongly suggested the possibility of acoustic Schwannoma. She was treated with a low dose of risperidone (1 mg daily), and her psychotic symptoms gradually and completely resolved over the next month. She is presently well and continues with antipsychotic drug maintenance.
DISCUSSION
Psychotic symptomssuch as auditory hallucinations and delusions without neurological sensory and motor symptoms are suggestive of functional psychosis. This case, however, had some distinct clinical characteristics. The symptoms developed very suddenly without any precipitating factor in a middle-aged patient. While there were several positive symptoms, there were minimal negative symptoms, such as those seen inschizophrenia.
Imaging revealed abnormal signals in the right CPA, which could cause psychotic symptoms. Therefore, this patient's psychotic symptoms could be due to the CPA mass, although it is possible that she suffered from 2 distinct disorders.
Previously published reports suggest that disturbances in the CPA region can cause psychiatric symptoms, including psychosis. Some studies also suggest that acoustic (trigeminal) Schwannoma is strongly associated with psychiatric symptoms. The CPA is a structure at the margin of the cerebellum and the pons where acoustic neuromas are usually found. CPA lesions cause a distinct neurologic syndrome due to the anatomic proximity of the CPA to specific cranial nerves. CPA lesions may compress surrounding structures, resulting in or producing psychiatric symptoms through disconnecting or affecting limbic pathways.1-4
There are many controversies regarding the laterality of brain lesions that cause psychiatric symptoms. This case was a right CPA mass. Several studies have reported that lateralized hemispheric dysfunction is a correlate of psychotic symptoms in schizophrenia and schizophrenia-spectrum disorders, but no clear consensus has been reached.6-14 Discrepancies in case reports and studies might be related to several factors, including demographic or clinical characteristics of the subjects, heterogeneous psychotic symptoms, and different drug regimens.15
Psychotic symptoms can also be major symptoms in temporal-lobe epilepsy. In this case, brain EEG was performed to assess other possible organic causes, but there were no abnormal findings. Further, the psychotic symptoms in this patient developed suddenly at a later age and completely improved after 1 month of antipsychotic drug treatment. Therefore, we confidently ruled out epilepsy as the cause of psychotic symptoms in this case.
In conclusion, our case with clinical and MRI findings demonstratesthat suddenly developed psychotic symptoms at a later age may be due to a right CPA lesion. This case shows that MRI is an essential screening tool for determining an organic basis for psychosis. It is not uncommon or unusual to perform MRI in cases that present with acute positive psychotic symptoms at a later age. However, because MRI cannot detect functional abnormalities, positron emission tomography and single-photon emission computed tomography are also useful for evaluating abnormalities that underlie symptom pathophysiology. Although we suggested employing these modalities, our patient did not agree for financial reasons.