Do Defense Styles of Ego Relate to Volumes of Orbito-Frontal Cortex in Patients with Obsessive-Compulsive Disorder?
Article information
Abstract
Objective
Although the importance of orbito-frontal cortex (OFC) is established in the pathogenesis of obsessive compulsive disorder (OCD), no study have evaluated its relation to the traditional psychodynamic perspective. In the present study, we aimed to evaluate the relationship between the defense styles consisting of mature, immature and neurotic defenses and OFC volumes of patients with OCD.
Methods
Subjects were selected among those of our previous study, and so eighteen patients with OCD and same number of healthy controls were took into the study. The patients and controls had underwent magnetic resonance imaging (MRI). In addition, the Defense Style Questionnaire-40 was administered to obtain defense styles of patients and controls.
Results
No significant relationship was found between the right OFC volumes of both the patient and control groups and their scores of mature, neurotic, or immature defense mechanisms. As for the left OFC volumes, the only significant relationship for the scores of immature defense mechanism was found in the patient group.
Conclusion
The results of the present study indicated that there was no significant relationship between OFC volumes of the patient group and their scores of mature, neurotic, or immature defense mechanisms, except a significant relation with the scores of immature defense mechanisms.
INTRODUCTION
Obsessive-compulsive disorder (OCD) comprising core symptoms of obsessions and compulsions is a common, chronic, anxiety disorder that can have disabling effects throughout lifetime with a wide range of clinical pictures. Its etiopathogenesis is obscure despite a huge different data coming from genetic, neurobiological, neurochemical and neuroimaging investigations.
Recent brain imaging techniques have revealed that specific circuits are responsible for the pathogenesis of OCD symptoms,1 particularly prefrontal-basal ganglia-thalamic-prefrontal circuits.2 Structural imaging studies of OCD have suggested basal ganglia and frontal pathology,2 with inconsistent reports of increases,3 decreases4,5 or no differences.6-12
In a recent meta-analysis, Whiteside et al.13 reported that meta-analytic results partially supported the conclusions drawn from previous narrative reviews that point to structures in the orbito-frontal cortex (OFC), caudate nucleus, anterior cingulate, and thalamus as the key brain regions in the pathophysiology of OCD. Functional imaging studies found altered activity in basal ganglia and prefrontal areas at rest and during behavioral challenge with feared stimuli in OCD patients.14 In addition to knowledge all above, as mentioned by MacMaster et al.,15 we should note that a critical brain region in this circuit is the OFC which is structurally the most ventral portion of the prefrontal cortex and have rich connections to the amygdala and dorsomedial thalamus16 areas implicated in OCD17-20 and functionally, it plays a role in linking affective value to reinforcing stimuli, sensory processing, and decision-making21 and which of all may be affected in OCD.22 On the other hand, OFC was probably found as the most important key brain region in our two previous study.23,24
According to psychoanalytic theory, obsessions and compulsions reflect maladaptive responses to unconsciously unresolved conflicts from early periods of psychological development and in Freud's view the patient's mind responded maladaptively to conflicts between unacceptable, unconscious sexual or aggressive id impulses and the demands of conscience and reality. This theory suggests that the ego marshalled certain defense mechanisms such as intellectualization and isolation, undoing to neutralize the offending ideas and impulses and reaction formation to adopt character traits exactly opposite of the feared impulses.
When we take a look at the psychiatric literature, there is dearth in the investigations which evaluate the relationship and interaction between neurobiological and psychoanalytic dimensions of psychiatric disorders. These investigations evaluating neurobiological and psychoanalytical dimensions of a variety of psychiatric disorders remain far from each other. In his review, Willick summarized recent advances, in that period, in neurobiological research which appeared to offer compelling evidence that the most pathognomonic feature of schizophrenia, the deficit or negative syndrome, might be associated with functional abnormalities in the frontal lobe of the brain which were correlated with those conceptualized by psychoanalytic theories of withdrawal of libido and loss of mental representation.25
Regarding OCD, no investigation has attempted to evaluate this relationship. In a brief report, Albucher et al.26 investigated the changes in defense mechanisms with the Defense Style Questionnaire after treatment of patients with OCD and found that after behavioral therapy the patients demonstrated significant decreases in Yale-Brown Obsessive Compulsive Scale scores and significant increases in the use of more adaptive defense mechanisms without changes maladaptive defense mechanism categories and concluded that personality as defined by defense mechanisms might be more amenable to brief behavioral treatment than previously thought. On the other hand, Katz proposed a model of 5-HT function involving the routine filtering and suppression of violent or libidinal impulses which appeared to resemble Freud's model of ego-id interactions at least in part, suggesting that it might be possible to psychobiologically substantiate a Freudian metaphor.27 Another effort came from Cath et al.28 who undertook to compare measures of psychopathology, personality and blood serotonin between Gillette de la Tourette syndrome (GTS) and OCD (without tics) and evaluated fifteen GTS without OCD subjects, 21 tic with (+) OCD subjects, 15 OCD without tic subjects and 26 controls (all without serotonergic medication) in regard to self-rated and clinician-rated measures of psychopathology and personality and reported that there were interaction effects on platelet MAO, 5-HT, Yale-Brown Obsessive-Compulsive Rating Scale severity, trait anxiety and Eysenck Personality Questionnaire neuroticism scores. In fact, the approaches existing an integration between psychoanalytical theory and neuroscience are based on Freud's opnion who he sought a unitary conception of mind and brain.26 In association with this, relatively increasing interest led some researchers to investigate the association between neurobiological mechanisms and psychodynamic processes. In one of this attemt, Schore et al.7,8 propose neurobiological mechanisms of psychodynamic processes, emphazising the developmental features of the right OFC. On the other hand, Northoff et al.20 were able to link sensorimotor regression, to a complex neural network including the OFC, medial prefrontal and premotor cortexes. Moreover, Solms6 and Solms et al.30 make inferences about the localization of early, immature and somatic defense mechanisms, based on psychoanalytic treatment in patients with orbitofrontal cortical lesions. Because of the fact that the OFC plays an important role in both emotion and cognitive interaction, Westen and Gabbard13,14 consider this region to be crucial in conflict and compromise. However, despite these attempts and importance of defense mechanisms in psychoanalytic theory and practice, their underlying neuronal mechanisms remain unclear.
Although the importance of OFC is emphasized both in the pathogenesis of OCD and in the neurobiological mecahisms based on psychodynamic process, no study have evaluated its relation to the traditional psychodynamic perspective. In the present study, we aimed to evaluate the relationship between the defense styles consisting of mature, immature and neurotic defenses and OFC volumes in the patients with OCD and thus, to take first step the interaction between psychodynamic and neuroanatomical dimensions of the disorder.
METHODS
Subjects and clinical evaluation
Subjects and clinical evaluation design were exactly same as our previous study23 which were composed of two age and sex matched groups: OCD and healthy subjects, each had 30 subjects, who were all right handed. The Diagnostic and Statistical Manual of Mental Disorders Fourth Version (DSM-IV) diagnoses were obtained using Turkish version of Structured Clinical Interview for DSM-IV (SCID).29 The patients with OCD were selected among the patients who had been recruited from Firat University School of Medicine Department of Psychiatry and had been invited to obtain their magnetic resonance imagings for our aforementioned study in which 30 patients had been included to adjust age and gender. Among these 30 patients, by age and sex adjustment, 24 patients were called by telephone and 18 accepted this. Only two of them were refractory patients while the others were treatment-responded (n=9) and drug-naive ones (n=7). Same number of comparison volunteers were selected among healthy persons who had been recruited from the hospital staff and had been invited to obtain their magnetic resonance imagings for our study aforementioned. Among these 30 controls, by age and sex adjustment, 18 were called and all accepted this. This study was carried out under guidelines of Helsinki Declaration. Written informed consent was obtained from all subjects.
As mentioned in our previous investigation,23 the exclusion criteria include the presence of any current or history of comorbid psychiatric disorder, current medical problems, or alcohol/substance abuse within the 6 months preceding the study. Healthy control subjects had no DSM-IV Axis I disorders in self or in a first-degree relative, as determined by the SCID non-patient version, no current medical problems, neurologic or psychiatric histories, and no use of psychoactive medication within 2 weeks of the study.
Of the patients, only four had any Axis II disorder (obsessive compulsive personality disorder in two patients, dependent in one and avoidant in one). As for the controls, none had any Axis I and II disorders. The severity of OCD, used defense styles were evaluated by using the Yale-Brown Obsession Compulsion Scale (Y-BOCS) and Defense Style Questionnaire (DSQ)-40, respectively.30,31 Defense mechanisms were divided into three groups by their psychoanalitical function: mature, neurotic and immature styles. The DSQ-40 are scored by obtaining the average of the two items for each scale. The factor scores are the average of the scale scores for scales 1-4 (mature), scales 5-8 (neurotic), and scales 9-20 (immature defenses). Mature defense styles are sublimation, humor, anticipation, and suppression. Neurotic defense styles include undoing, pseudoaltruism, idealization and reaction-formation whereas immature styles consist of projection, passive-aggression, acting out, isolation, devaluation, autistic fantasy, denial, displacement, dissociation, splitting, rationalization and somatization.
MRI procedure
As mentioned in our previous study,23 magnetic resonance imaging scans were acquired with a 1.5 T General Electric scanner. Spiral pulse sequences were employed because of insensitivity to subject motion. MRI was obtained on a 1.5-Tesla GE signa Excite high speed scanner (Milwaukee, USA). Spiral pulse sequences were employed because of insensitivity to subject motion. A high-resolution structural image of the entire brain was obtained using sagittally acquired 3D spiral fast spin echo high-resolution images [repetition time (TR)=2,000 ms, echo time (TE)=15.6 ms, field of view (FOV)=240 mm, flip angle=200, bandwidth=20.8, slice thickness=2.4 mm, echo spacing=15.6 ms, 8 echoes, resolution=0.9375×0.9375×1.328 mm]. The boundaries of structures evaluated were delineated on the coronal MR images according to standard brain atlases32-34 and were adapted from Noga et al.,35 Portas et al.,36 Lacerda et al.,37 Sassi et al.38 and Riffkin et al.39 For the tracing procedure for measuring the OFC, superior boundary was defined by a line extending from the anterior commissure to the posterior commissure. On the coronally, the posterior boundary was defined as the point when the olfactory sulcus was first noticed. The inferior boundary was accepted as the most inferior aspect of the cortex. The lateral and medial boundaries were defined as the most lateral edge of the cortex and the medial boundary of each hemisphere by the longitudinal fissure, respectively. Examples of the structures of OFC are presented in Figure 1. All volumes were reported in cubic centimeters. The test-retest relaiblity for tracing was r=0.92 for OFC.
Statistical analysis
Statistical analyses were conducted using SPSS for Windows software, version 13.0 (SPSS, Chicago, IL). Group differences in demographic variables involving continuous data were computed using independent t-test. Between-group comparisons involving categorical data were assessed using Chi-square test. Correlations were assessed with Spearman's correlation test.
RESULTS
There was no significant difference between the patients with OCD and healthy controls in age (mean age±SD=27.7±5.1 vs. 28.7±3.9 years, respectively; p>0.05) or gender (p>0.05).
Table 1 presents the unadjusted mean volumes of measured structures for the patients and healthy controls. We did not find any significant difference between the OCD patients and healthy controls on ICV (t=0.089, df=34, p>0.05), and total gray matter volumes (t=0.69, df=34, p>0.05), but there was significant greater total white matter volumes in the patients (t=2.16, df=34, p=0.038). Both sides of the OFC volumes of the patients were significantly smaller than those of healthy controls (t=-5.084, df=34, p<0.001 for right OFC and t=-5.415, df=34, p<0.001 for left OFC) even after covarying for ICV and Y-BOCS scores (F=4.88, p<0.05 for age, and F=4.12, p<0.05 for Y-BOCS).
As expected, scores of mature factor were 30.00±9.29 for patients and 41.28±12.54 for control subjects, respectively (t=-3.065, df=34, p=0.004). The scores of the neurotic factor were significantly higher in patient group compared to healthy comparisons [49.00±13.99 for patients and 36.06±6.86 for control subjects, respectively (t=3.524, df=34, p=0.001)]. In regard to scores of immature factor, these scores were also statistically significant higher in patients (116.00±26.92) compared to control subjects (78.67±17.38) (t=4.943, df=34, p<0.001). No gender-related defense style difference was found in both patient and control groups for any style (p>0.05).
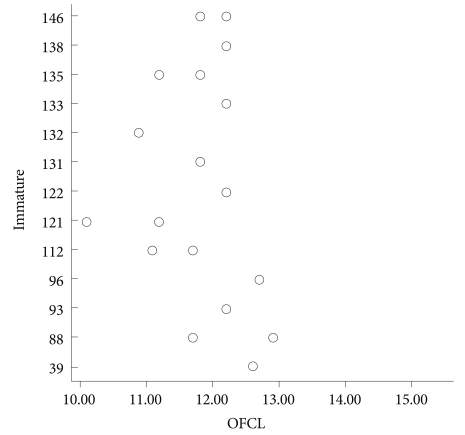
No significant relationship was found between the right OFC volumes of the patient group and their scores of mature (Spearman's rho=0.176, p>0.05), neurotic (Spearman's rho=-0.341, p>0.05), or immature defense mechanism scores (Spearman's rho=-0.191, p>0.05). As for the left OFC volumes, there was statistically significant association with the scores of immature defense mechanisms (Spearman's rho=0.653, p=0.003)(Figure 2). However, no association was found between the left OFC volumes and the scores of neurotic or matures defense styles (Spearman's rho=0.130, p>0.05 for the neurotic defense styles and Spearman's rho=-0.053, p>0.05 for the mature defense styles). For the healthy comparison group, no relationship was found between the right and left OFC volumes and the scores of any defense styles (Spearman's rho=-0.259, p>0.05 for the right OFC-mature styles; Spearman's rho=-0.311, p>0.05 for the right OFC-neurotic styles; Spearman's rho=-0.150, p>0.05 for the right OFC-immature styles; Spearman's rho=-0.140, p>0.05 for the left OFC-mature styles; Spearman's rho=0.089, p>0.05 for the left OFC-neurotic styles; and Spearman's rho=0.238, p>0.05 for the left OFC-immature styles).
DISCUSSION
To our knowledge, this is the first study which consists of brain volumetric variables and psychoanalitical data in OCD. Beyond finding greater volumes of total white matter and smaller OFC volumes as determined previously by our group,24 the main findings of the present study were us to find no significant relationship between the right OFC volumes of the patient group and their scores of mature, neurotic, or immature defense mechanism scores, but as for the left OFC volumes, to detect a significant relation with the scores of immature defense mechanisms (Spearman's rho=0.653, p=0.003) while no association was found about the scores of neurotic or mature defense styles.
This area is considerably novel even in all kinds of psychiatric disorders including schizophrenia and depression on which there are so many studies compared to OCD. In addition to our important findings aforementioned, another important finding was that the scores of mature defense styles were lower in the patients with OCD compared to healthy controls, while those of neurotic and immature styles were significantly higher in the patient group than healthy comparisons. Our this finding that the scores of mature defense styles were lower in the patients with OCD compared to healthy controls, while those of neurotic and immature styles were significantly higher in the patint group than healthy comparisons was actually expected one. Actually, this is an expected finding which has been supported by Albucher et al.26 found that after behavior therapy the patients demonstrated a significant decreases in Y-BOCS scores and significant increases in the use of more adaptive defense mechanisms without any significant changes in maladaptive defense mechanism categories.
The second and main finding of the present study was that no significant relationship was found between the right OFC volumes of the patient group and their scores of mature, neurotic, or immature defense mechanism scores, but as for the left OFC volumes, a significant relation was determined with the scores of immature defense mechanisms while no association was detected about the scores of neurotic or matures defense styles. In our unpublished study,40 we examined the relationship between the defense styles and NAA, CHO, and CRE values in hippocampal regions of OCD patients and found important correlations. As can be extracted from our another study, defense styles seem to be associated with neurochemical variables. However, one of the most important regions in the pathophysiology of OCD, OFC's volumetric data do not seem to be related to the defense styles, except a significant relation with the scores of immature defense mechanisms for the left OFC.
The meaning of the finding that there was no relationship between OFC volumes and neurotic defense styles but was a relationship between the immature defense styles and left OFC volumes but not right is unclear and needed further exploration. Several explanations may be done for this. Firstly, we should accept the fact that positive results may be artefact. Secondly, in our previous study,23 we found that first applying patients had significantly smaller left and right OFC volumes compared with treatment-responded patients and healthy controls, with a significant difference between refractory patients and treatment-responded patients for both sides and no significant difference between the volume of first applying patients compared to that of refractory patients. In that study, we suggested that reductions in OFC and increase in thalamic volumes might be associated with refractoriness of OCD and might not be due to changes in cingulate and caudate regions. This led us to consider that refractoriness to treatment might be associated with more use of immature defense mechanisms rather than neurotic ones. As for the issue of side, in that study,23 by using analysis of covariance controlling for age and intracranial volume, the reduction in left OFC was more obvious compared to right side despite for both sides there were significant difference compared to -responded patients and healthy controls. This difference may explain our finding found in the present study that there was statistically significant association with the scores of immature defense mechanisms.
Some factors need to be considered when interpreting these results. First, the relatively small and homogeneous sample may limit the generalizability of our findings to OCD. It requires the replication with larger samples whether our findings are applicable to cases of patients with OCD with psychotic features. Second, as we acknowledged, the statistical threshold applied is somewhat liberal, further underscoring the need for replication. Third, single but important key brain region for OCD, OFC was investigated in this study. Finally, whereas the current investigation utilized a retrospective design in part, a prospective research design is ultimately necessary.
In conclusion, the results of the present study indicate being no significant relationship between OFC volumes of the patient group and their scores of mature, neurotic, or immature defense mechanism scores, except a significant relation with the scores of immature defense mechanisms and lead us to consider defense styles seem to be associated with neurochemical variables in OCD, taking into consideration our unpublished study.