Korean Version of Mini Mental Status Examination for Dementia Screening and Its' Short Form
Article information
Abstract
Objective
We developed a Korean version of Mini-Mental Status Examination (MMSE) optimized for screening dementia (MMSE-DS) and its' short form (SMMSE-DS).
Methods
We constructed the MMSE-DS using the items of the two current Korean versions of MMSE and then construct the SMMSE-DS consisted of 13 items from the MMSE-DS based on the diagnostic accuracy of individual items for dementia. We investigated reliability and validity of MMSE-DS and SMMSE-DS on 1,555 subjects (1,222 nondemented controls, 333 dementia patients). We compared the diagnostic accuracy of the SMMSE-DS with that of the three full Korean versions of MMSE, and examined its' age- and education-specific optimal cutoff scores for dementia.
Results
The internal consistency obtained by Cronbach's coefficient alpha was 0.826. The inter-rater reliability and test-retest reliability were 0.968 (p<0.001) and 0.825 (p<0.001), respectively. It showed significant correlation with the Clinical Dementia Rating (CDR) (r=-0.698, p<0.05) and the three full Korean versions of MMSE (r=0.839-0.938, p<0.001). The area under the receiver operator curve for dementia of the SMMSE-DS was larger than those of the three full Korean versions of MMSE (p<0.001). Age, education and gender explained 19.4% of the total variance of SMMSE-DS scores. The optimal cutoff scores for dementia of the SMMSE-DS were estimated differently by age and educational attainment of the subjects.
Conclusion
The SMMSE-DS was found to be accurate, brief and portable instrument for screening dementia in Korean elders, and may be particularly useful for screening dementia in elderly populations with wide variation in educational levels.
Introduction
The prevalence of dementia is increasing and interventions are more widely available. This creates a need for accurate screening tests for early detection of the condition. Ideally, such tests should be adequately sensitive and specific to identify cognitively impaired individuals requiring comprehensive evaluation and management, and could be quickly and easily administered not only by physicians but also by nurses or other trained healthcare personnel.
The Mini-Mental Status Examination (MMSE) is the most widely used screening instrument for dementia.1-4 The MMSE contains 19 items and the maximum score is 30 points (10 points for orientation, 6 for verbal memory, 5 for concentration and calculation, 5 for language, 3 for praxis, 1 for visuospatial construction). Three Korean versions5-7 have been standardized and normative data have been obtained in tests with elderly Korean indivduals.8,9
However, MMSE, in the current form, has several limitations in dementia screening despite excellent inter-rater reliability and good criterion and construct validity.10-13 First, MMSE is not fully optimized for screening dementia because the test was originally developed to evaluate elderly psychiatric patients rather than those with dementia.14,15 For example, the relative weight of items for memory, which is the earliest and most common cognitive deficit in dementia, is only 6 of 30 points. This low weight is associated with a reduced diagnostic accuracy of MMSE in dementia assessment compared with other screening tests such as the Revised Hasegawa Dementia Scale (HDS-R).16,17 Second, MMSE performance in dementia diagnosis is more significantly influenced by educational level than are other screening instruments.18-21 Finally, MMSE cannot be fully administered to disabled elderly individuals with motor impairment because MMSE contains performance tests that assess praxis and visuospatial function.
Therefore, we developed a short version of the MMSE for dementia screening (SMMSE-DS) which is more accurate, briefer and can be administered more easily to the individuals with motor impairment on the basis of the diagnostic accuracy of each MMSE item for dementia, and then examined the psychometric properties of the SMMSE-DS system.
Methods
Subjects
All subjects were Korean elders aged 60 years or over. Cognitively normal control subjects were recruited from participants in the Korean Longitudinal Study on Health and Aging (KLoSHA)22 or from volunteers in the National Dementia Screening and Registry Program (NDSRP). The KLoSHA is a population-based longitudinal study on health, aging and common geriatric diseases in Korean elderly aged 65 years and older. The subjects with dementia were recruited either from the participants of the KLoSHA or the visitors to the Dementia Clinics of eight university hospitals in 2009.
Assessment
Each subject was examined by a geropsychiatrist with advanced training in the neuropsychiatry and dementia research according to the protocol of the Korean version of the Consortium to Establish a Registry for Alzheimer's disease (AD) Assessment Packet (CERAD-K).6 Three Korean versions of MMSE were coadministered to evaluate the concurrent validity of SMMSE-DS. Two of these questionnaires {Korean version of MMSE in the CERAD-K (MMSE-KC)6 and Korean version of MMSE in the Seoul Neuropsychological Screening Battery (K-MMSE)23} had been previously standardized, but one version (MMSE-DS) was newly constructed, within the present study, to develop the SMMSE-DS. Subjects diagnosed with dementia by the criteria of the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV),24 were enrolled in the patient group. Those who were functioning independently in the community and did not show any cognitive impairment formed the control group. Subjects with serious medical, psychiatric, or neurological disorders that might have affected cognitive function were excluded.
Formulation of the SMMSE-DS
We initially prepared a new Korean version of the MMSE-DS. All items of MMSE-DS, with the exception of a single question, were adapted from either MMSE-KC6 or K-MMSE.7 The five items for time orientation were adapted from MMSE-KC without modification. Five questions exploring for place orientation were adapted from the MMSE-KC with minor modification of scoring criteria. Three words testing immediate and delayed recall were adapted from MMSE-KC (tree, car, and cap), as these terms are more frequently used by Koreans25 than those in the K-MMSE. Serial 7s in the K-MMSE was adapted for the item testing concentration in the MMSE-DS. The items for naming test were also adapted from the K-MMSE (watch, pencil) since the items of the K-MMSE were easier to carry than those of the MMSE-KC (stamp, key). The repetition unit was adapted from MMSE-KC, as this may be less influenced by educational level than is the equivalent items in K-MMSE. The items for ideational praxis were adapted from the MMSE-KC since they were more similar to those in the original English version of MMSE than those of the K-MMSE. The visuospatial construction item was taken from the original English version of MMSE. Terms assessing reading and writing in the original English version of MMSE were modified into items evaluating judgment and abstract thinking, because 40.1% of Korean elders aged 65 years or more have not received formal education.26 The item for testing judgment was adapted from the MMSE-KC ("Why do you wash your clothes?"). Interpretation of a familiar Korean proverb ("Many a little makes a mickle.") was used to test abstract thinking.
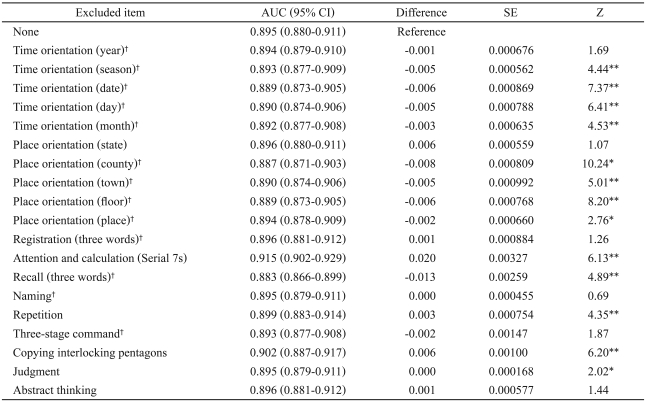
Next, we examined changes in areas under receiver operator curves (AUCs) of MMSE-DS excluding individual items, and constructed the 20-point SMMSE-DS by discarding the items that was not found to contribute to the diagnostic accuracy of the MMSE-DS for dementia.
Data analysis
To evaluate inter-rater reliability, two raters simultaneously assessed 31 participants (11 control subjects; 20 dementia patients). To examine test-retest reliability, the same raters administered MMSE-DS to the same participants 4 weeks after initial assessment. Inter-rater and test-retest reliability was determined using Pearson correlation coefficients, and internal consistency was examined using Cronbach's alpha coefficient.
To evaluate discriminant validity, mean scores of the MMSE-DS and SMMSE-DS of patient and control groups were compared by analysis of variance (ANOVA). The univariate normality assumptions were verified using the Welch and Brown-Forsythe modifications of Levene's test. The Games-Howell multiple comparison technique was applied post-hoc to ANOVA data.
To evaluate concurrent validity, correlations of MMSE-DS and SMMSE-DS with the other two Korean versions of MMSE (MMSE-KC and K-MMSE) were examined using two-tailed Pearson correlation tests, and correlations with the Clinical Dementia Rating (CDR)27 were examined by the Spearman rank-order correlation test.
We derived optimal cut-off scores satisfying both sensitivity and specificity criteria for dementia using receiver-operator characteristic (ROC) analysis. To assess the diagnostic accuracy of each test for dementia, we compared the AUCs of MMSE-DS, SMMSE-DS, MMSE-KC and K-MMSE by calculating the critical ratio "z", as proposed by Hanley and McNeil.28 Multiple linear regression analysis with stepwise variable selection assessed the relative contributions of age, education, and gender to MMSE-DS and SMMSE-DS scores. All statistical analyses were performed using Statistical Package for the Social Sciences (SPSS)(version 17.0) for Windows (SPSS Inc., Chicago, IL, USA).
Results
Subjects
A total of 1,555 subjects (1,222 nondemented controls; 333 dementia patients) were included in the present study. Among dementia patients, 142 had very mild dementia (CDR=0.5), 127 mild (CDR=1), 50 moderate (CDR=2), and 14 severe (CDR=3). A total of 242 patients (72.7%) were diagnosed with AD, 46 (13.8%) with vascular dementia (VD), 46 (13.8%) with dementia with Lewy body (DLB), 14 (4.2%) with frontotemporal dementia (FTD), and 8 (2.4%) with dementia of other etiologies. Demographic and clinical characteristics of all patients are summarized in Table 1.
Construction of SMMSE-DS
As shown in Table 2, the AUC of MMSE-DS increased when the six items testing place orientation for state, registration, attention/calculation, repetition, visuospatial construction and judgment were excluded, and the differences reached a statistical significance in the items for attention/calculation (z=6.13, p<0.001), repetition (z=4.35, p<0.001) and visuospatial construction (z=6.20, p<0.001). Of these items, five (orientation for state, attention/calculation, repetition, visuospatial construction and judgment) were not included in the SMMSE-DS. The item for registration was not discarded because this is a prerequisite for testing recall. In addition, we discarded the item testing abstract thinking because this was not included in the original English version of the MMSE, and the contribution of this item to the diagnostic accuracy of MMSE-DS was not statistically significant (z=1.44, p>0.05). Thus, SMMSE-DS is a 20-point scale containing 13 items including time orientation (5 points), place orientation (4 points), verbal memory (6 points), naming (2 points), and praxis (3 points).
Reliability
Both the MMSE-DS and SMMSE-DS showed excellent internal consistency. The Cronbach's alpha coefficients of the scales were 0.826 and 0.806, respectively. Inter-rater and test-retest reliabilities were 0.999 (p>0.001, Pearson correlation test) and 0.935 (p<0.001, Pearson correlation test), respectively, for MMSE-DS, and 0.968 (p<0.001, Pearson correlation test) and 0.826 (p<0.001, Pearson correlation test), respectively, for SMMSE-DS.
Validity
As shown in Table 1, SMMSE-DS, MMSE-DS, MMSE-KC, and K-MMSE scores differed significantly between control and dementia patients. As CDR increased in dementia patients, scores decreased significantly (p<0.001 by ANOVA). On posthoc analysis, scores were significantly lower in patients with dementia compared with control individuals, indicating that all of SMMSE-DS, MMSE-DS, MMSE-KC, and K-MMSE could validly discriminate between control and dementia patients. SMMSE-DS scores were significantly correlated with scores of the MMSE-DS (r=0.938, p<0.001), MMSE-K (r=0.924, p<0.001), K-MMSE (r=0.839, p<0.001), and CDR (r=-0.698, p<0.05), indicating that SMMSE-DS had a high concurrent validity (Table 3).
Diagnostic accuracy and optimal cutoff scores
The AUCs of the SMMSE-DS (AUCSMMSE-DS), MMSE-DS (AUCMMSE-DS), MMSE-KC (AUCMMSE-KC), and K-MMSE (AUCK-MMSE) were all greater than 0.80, indicating that all tests were useful in detecting dementia. AUCSMMSE-DS was significantly greater than AUCMMSE-DS (z=6.98, p<0.001), AUCMMSE-KC (z=7.56, p<0.001), and AUCK-MMSE (z=9.20, p<0.001), indicating that SMMSE-DS may be more accurate for the diagnosis of dementia than are the other three full Korean versions of MMSE (Figure 1).
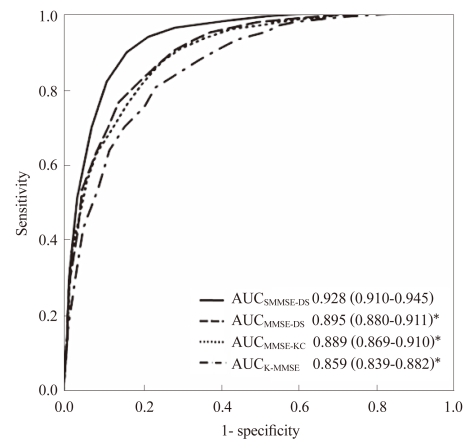
Comparison of areas under the receiver operator curve (AUC) of the short version of Mini-Mental Status Examination for dementia screen (SMMSE-DS) with those of the three full Korean versions of MMSE. *p<0.001. MMSE-KC: Korean version of MMSE in CERAD-K6, K-MMSE: Korean version of MMSE in the Seoul Neuropsychological Screening Battey,7 CERAD-K: Korean version of the Consortium to Establish a Registry for Alzheimer's disease Assessment Packet.
In subjects educated for 6 years or less, the AUCs of SMMSE-DS, MMSE-DS, MMSE-KC, and K-MMSE were 0.950 (0.937-0.963), 0.926 (0.909-0.942), 0.922 (0.905-0.939), and 0.892 (0.871-0.912), respectively. The AUCSMMSE-DS was significantly larger than AUCMMSE-DS (z=4.619, p<0.001), AUCMMSE-KC (z=5.047, p<0.001), and AUCK-MMSE (z=6.819, p<0.001). In patients who had been educated for 7 years or more, the AUC values of SMMSE-DS, MMSE-DS, MMSE-KC, and K-MMSE were 0.921 (0.901-0.942), 0.917 (0.896-0.938), 0.916 (0.895-0.938), and 0.888 (0.862-0.914). The AUCSMMSE-DS was larger than AUCK-MMSE (z=2.841, p<0.01), but comparable to AUCMMSE-DS (z=0.728, p=0.467) and AUCMMSE-KC (z=0.774, p=0.439).
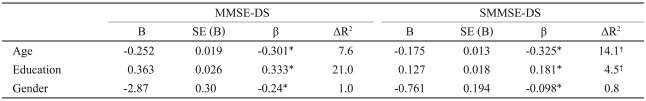
Stepwise multiple regression analysis revealed that age, gender, and educational level significantly affected SMMSE-DS and MMSE-DS scores (Table 5). These three demographic factors accounted for 19.4% and 29.6% of the total variance of SMMSE-DS and MMSE-DS, respectively. Although the demographic effect was significant in both tests, the overall R2 of demographic factors in the regression model of SMMSE-DS was significantly smaller than that of the MMSE (t=13.98, d.f.=1,554, p<0.001). Most of the difference in overall R2 between the two tests was attributable to the difference in the influence of education. The partial R2 of the educational level in the SMMSE-DS (4.5%) was about one-fifth that in MMSE-DS (21.0%) (t=42.29, p<0.001). The partial R2 age in SMMSE-DS was higher than that in MMSE-DS (t=12.19, p<0.001), and the partial R2 of gender in SMMSE-DS was similar to that in MMSE (t=1.17, p>0.05).
The optimal cutoff scores for dementia of the SMMSE-DS stratified by age and educational level are shown in Table 4. The AUCSMMSE-DS did not vary by educational level of subjects (z=1.58, p>0.05).
Discussion
We developed the Korean version of MMSE optimized for screening dementia (MMSE-DS) and its' short version (SMMSE-DS).
Our results show that SMMSE-DS performed better than did full versions of the MMSE, displaying both higher AUC values and increased sensitivity and specificity for dementia regardless of educational level of the subjects. The superiority of SMMSE-DS over full versions of MMSE can be attributed principally to differences in the cognitive measures included in the tests. Compared with full versions of MMSE, the relative weights of measures for memory and orientation were strengthened in SMMSE-DS. Because these parameters examine cognitive domains impaired early in dementia,29,30 such variations may have improved the diagnostic accuracy of SMMSE-DS. In addition, SMMSE-DS can be used in the uneducated elderly population more readily than the full MMSE version, because the SMMSE-DS does not feature tests on reading, writing, or copying of interlocking pentagons. Because the MMSE showed a higher false-positive rate in educationally disadvantaged populations,17 differences in diagnostic accuracy between SMMSE-DS and the full MMSE versions may be greater in poorly educated subjects. As might be expected, the diagnostic accuracy for dementia of SMMSE-DS was better than that of complete versions of MMSE in less-educated subjects, but was comparable to that of the full version MMSE in highly educated patients. These results indicate that the superiority of SMMSE-DS in the diagnosis of dementia, compared with complete versions of MMSE, may be greater in educationally disadvantaged populations.
The SMMSE-DS has several additional advantages in comparison with the full version of MMSE. First, SMMSE-DS is briefer than the full version of MMSE. Administration of SMMSE-DS takes much less time than is required for administration of full version MMSE because SMMSE-DS has less items than the full version MMSE (13 items versus 19 items). Second, SMMSE-DS is more portable than the full version of MMSE because SMMSE-DS does not include the paper-and-pencil tests included in the full version MMSE, such as the copying of interlocking pentagons. The brevity and portability of SMMSE-DS may be advantageous over the full MMSE in mass screening of dementia.
The present study had some strengths. First, the proportion of very mild (CDR=0.5) and mild (CDR=1) dementia patients in our patient group exceeded 80% (very mild: 42.6%, mild: 38.1%), and our results can thus be extrapolated to detection of mild dementia. Many previous studies included participants with severe dementia, and few reports have provided information on the accuracy of screening tests in the detection of mild dementia. The diagnostic accuracy data of such studies may be most appropriately extrapolated to detection of moderate dementia. However, it would be better to enroll subjects with mild dementia, who are usually the focus of screening tests in evaluating screening tests. Second, we compared diagnostic accuracy not only using sensitivity and specificity values, but also using AUC data. Although assessment of diagnostic accuracy using sensitivity and specificity is common, this approach is adequate only when decision criteria such as a cut-off score are agreed among physicians, and are invariant. Moreover, the decision criterion is susceptible to differences in the characteristics of study sample. For example, the sensitivity and specificity of MMSE varied from 71-92%, and 51-96%, respectively.14,15 In contrast, an AUC value is independent of any decision criterion and is less influenced by extraneous factors that affect patient response, although an AUC cut-off is neither perfectly reliable nor completely valid because no such estimation is free from the influence of study design or administration procedure. Thus, AUC values provide a better measure of predictive accuracy than do sensitivity and specificity figures.
Two limitations are apparent in the present study. First, the concurrent validity of the SMMSE-DS was tested in comparison with three full Korean versions of MMSE which have many items in common with SMMSE-DS. This might have exaggerated the observed correlation coefficients. Second, the sources of control and patient groups were different. Most control subjects were community-dwelling elderly individuals, whereas the majority of dementia patients were recruited from subjects visiting hospitals. Such differences in sample source may have exaggerated the AUC values for dementia of the SMMSE.
In conclusion, SMMSE-DS is an accurate, brief, and portable instrument for screening dementia in Korean elderly individuals, and may be particularly useful in detecting dementia in elderly populations with wide variations in education level.
Acknowledgments
This study was supported by a research grant from the Ministry of Health and Welfare, Korea (Grant NO. 08-2009-014).