1. Kim HJ, June K, Shin G, Choo J. Associations between job stress and work-related musculoskeletal symptoms in street sanitation workers. J Korean Acad Community Health Nurs 2013;24:314-322.

2. Rusli BN, Edimansyah BA, Naing L. Working conditions, self-perceived stress, anxiety, depression and quality of life: a structural equation modelling approach. BMC Public Health 2008;8:48PMID:
18254966.



3. Chang SJ, Koh S, Kang D, Kim S, Kang M, Lee C. Developing an occupational stress scale for Korean employees. Korean J Occup Environ Med 2005;17:297-317.

4. Kim Y. The Influence of a general hospital nurse's emotional labor, emotional intelligence on job stress. J Digit Convergence 2014;12:245-253.

5. Tomioka K, Morita N, Saeki K, Okamoto N, Kurumatani N. Working hours, occupational stress and depression among physicians. Occup Med (Lond) 2011;61:163-170. PMID:
21383384.


6. Yoshizawa K, Sugawara N, Yasui-Furukori N, Danjo K, Furukori H, Sato Y, et al. Relationship between occupational stress and depression among psychiatric nurses in Japan. Arch Environ Occup Health 2014;[Epub ahead of print].

7. Cho JJ, Kim JY, Chang SJ, Fiedler N, Koh SB, Crabtree BF, et al. Occupational stress and depression in Korean employees. Int Arch Occup Environ Health 2008;82:47-57. PMID:
18301911.


8. Kim K, Park J, Park B. The effects of job stress with depression and fatigue of firemen. J Korea Cont Assoc 2014;14:223-231.

9. Yang X, Ge C, Hu B, Chi T, Wang L. Relationship between quality of life and occupational stress among teachers. Public Health 2009;123:750-755. PMID:
19883926.


10. Aleman A. Use of repetitive transcranial magnetic stimulation for treatment in psychiatry. Clin Psychopharmacol Neurosci 2013;11:53-59. PMID:
24023548.



11. Li CT, Wang SJ, Hirvonen J, Hsieh JC, Bai YM, Hong CJ, et al. Antidepressant mechanism of add-on repetitive transcranial magnetic stimulation in medication-resistant depression using cerebral glucose metabolism. J Affect Disord 2010;127:219-229. PMID:
20598753.


12. Karsen EF, Watts BV, Holtzheimer PE. Review of the effectiveness of transcranial magnetic stimulation for post-traumatic stress disorder. Brain Stimul 2014;7:151-157. PMID:
24486424.


13. Nemeroff CB. Prevalence and management of treatment-resistant depression. J Clin Psychiatry 2007;68(Suppl 8):17-25. PMID:
17640154.


14. Sandrini M, Cohen LG. Noninvasive brain stimulation in neurorehabilitation. Handb Clin Neurol 2013;116:499-524. PMID:
24112919.



15. Zhu H, Lu Z, Jin Y, Duan X, Teng J, Duan D. Low-frequency repetitive transcranial magnetic stimulation on Parkinson motor function: a meta-analysis of randomised controlled trials. Acta Neuropsychiatr 2015;27:82-89. PMID:
25592544.


16. Pellicciari MC, Cordone S, Marzano C, Bignotti S, Gazzoli A, Miniussi C, et al. Dorsolateral prefrontal transcranial magnetic stimulation in patients with major depression locally affects alpha power of REM sleep. Front Hum Neurosci 2013;7:433PMID:
23935577.



17. Madsen IE, Lange T, Borritz M, Rugulies R. Burnout as a risk factor for antidepressant treatment - a repeated measures time-to-event analysis of 2936 Danish human service workers. J Psychiatr Res 2015;65:47-52. PMID:
25943951.


18. Ruotsalainen JH, Verbeek JH, Marine A, Serra C. Preventing occupational stress in healthcare workers. Cochrane Database Syst Rev 2014;(11):CD002892

19. First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSM-IV-TR axis I Disorders, Research Version, Patient Edition. New York: Biometrics Research, New York State Psychiatric Institute; 2002.
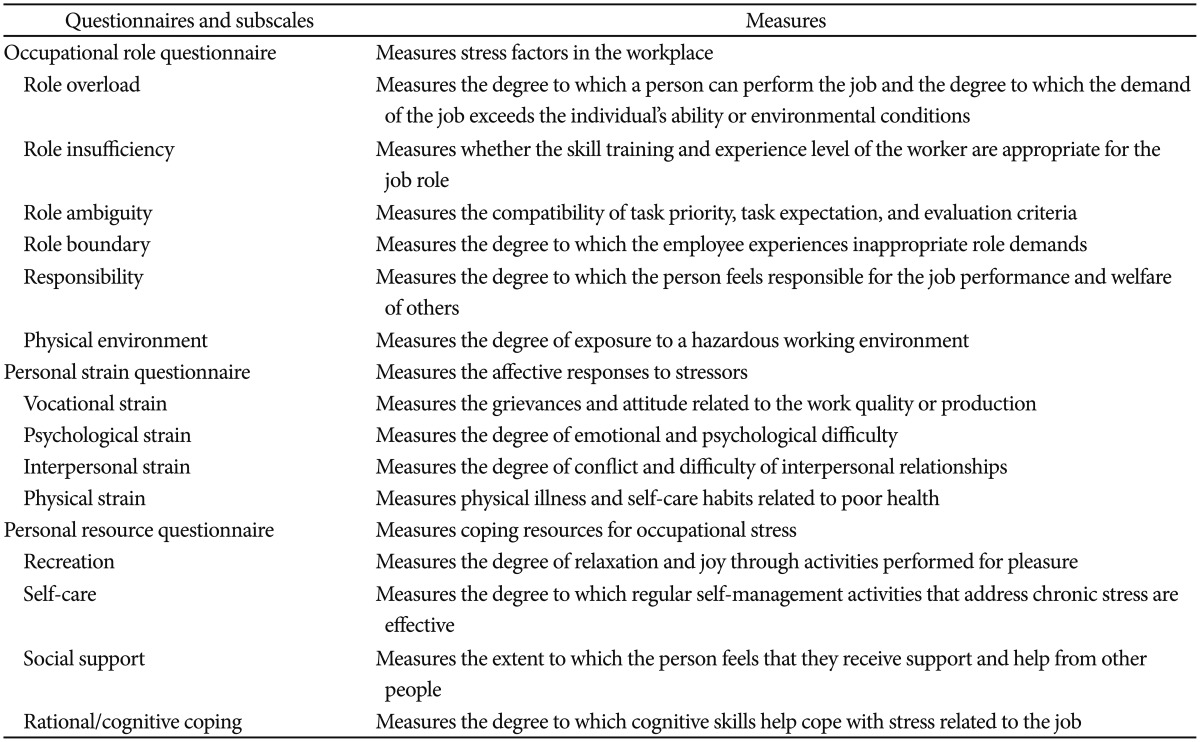
20. Osipow S, Spokane A. Occupational Stress Inventory: Manual Research Version. Odessa, FL: Psychological Assessment Resources; 1992.
21. Lee J, Byun J, Kim S, Lee H, Kim H. The impact of occupational stress on suicide ideation of subway drivers. Occup Environ Med 2014;71:A74

22. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry 1961;4:561-571. PMID:
13688369.


23. Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 1988;56:893-897. PMID:
3204199.


24. George MS, Lisanby SH, Avery D, McDonald WM, Durkalski V, Pavlicova M, et al. Daily left prefrontal transcranial magnetic stimulation therapy for major depressive disorder: a sham-controlled randomized trial. Arch Gen Psychiatry 2010;67:507-516. PMID:
20439832.


25. Lisanby SH, Gutman D, Luber B, Schroeder C, Sackeim HA. Sham TMS: intracerebral measurement of the induced electrical field and the induction of motor-evoked potentials. Biol Psychiatry 2001;49:460-463. PMID:
11274658.


26. George MS, Avery D, Nahas Z, Molloy M, Oliver NC, Risch SC, et al. rTMS studies of mood and emotion. Electroencephalogr Clin Neurophysiol Suppl 1999;51:304-314. PMID:
10590964.

27. Lui S, Wu Q, Qiu L, Yang X, Kuang W, Chan RC, et al. Resting-state functional connectivity in treatment-resistant depression. Am J Psychiatry 2011;168:642-648. PMID:
21362744.


28. Drevets WC. Functional anatomical abnormalities in limbic and prefrontal cortical structures in major depression. Prog Brain Res 2000;126:413-431. PMID:
11105660.