The Relationship between Impulsivity and Quality of Life in Euthymic Patients with Bipolar Disorder
Article information
Abstract
Objective
Bipolar disorder (BD) is characterized by elevated impulsivity, even during periods of remission. Many recovered BD patients have functional impairments, which can lead to poor quality of life (QoL). The aim of this study was to investigate the association between impulsivity and QoL in euthymic BD patients.
Methods
A total of 56 remitted or recovered patients with type I or II BD, diagnosed based on Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria, were recruited. Psychiatrists administered the Clinical Global Impression (CGI) for BD and the Global Assessment of Functioning (GAF) scales and then interviewed the subjects to assess clinical variables. Patients completed the Barratt Impulsiveness Scale (BIS-11) and the World Health Organization Quality of Life Assessment Instrument-Brief Form (WHOQoL-BREF). Pearson correlations, univariate regression analyses, and multiple linear regression analyses were performed.
Results
The BIS-11 total score was significantly correlated with the WHOQoL-BREF total score (r=-0.55, p<0.01) and with the WHOQoL-BREF subscales. After controlling for GAF score and other clinical variables, the BIS-11 total score (β=-0.43, p=0.001) was independently associated with overall QoL. Additionally, the BIS-11 total score was particularly strongly associated with the physical, psychological, and social domains of the multi-dimensional QoL scale.
Conclusion
Our results suggest that high impulsivity is related to low QoL in euthymic BD patients. Further studies are needed to examine whether interventions for high impulsivity effectively improve QoL in patients with BD.
INTRODUCTION
Bipolar disorder (BD) is a chronic mental illness characterized by recurring episodes of depression and mania or hypomania. The World Health Organization (WHO) labeled BD as one of 10 major causes of disability.1 The functional recovery rate is less than 50% for patients suffering from BD, even when considering individuals in remission.2-4 Patients with BD report lower quality of life (QoL) when compared with patients with other medical conditions, including asthma, obesity, and chronic back pain.5-8
QoL is a concept that encompasses various domains and includes physical, psychological, functional, social, economic, and vocational factors.9 The QoL of patients with BD is more impaired during depressive than manic or hypomanic episodes. 8 Even for remitted BD patients, the physical, mental, social, and environmental aspects of QoL are impaired.10,11 Recently, efforts to treat BD have targeted improving the level of functional recovery and QoL rather than ameliorating isolated symptoms as important goals.8
To achieve these goals, it is important to identify factors that affect BD patients' QoL. Demographic and clinical characteristics that contribute to poor QoL include prolonged illness duration,5 young age of onset,12 being female,13 history of suicide attempts,14 poor insight,11 high nicotine dependence,15 absence of a social support system,15 comorbid alcohol dependence, 16 comorbid anxiety disorders,17 numerous previous depressive episodes,18,19 and an extended undiagnosed period.20 Residual depressive symptoms are also associated with poor QoL.6 Additionally, Victor et al.21 reported that elevated impulsivity among patients with BD type I (BD-I) is associated with poor QoL. However, their study was limited because of their inclusion of patients with BD who were not in remission.
Impulsivity can be defined as a tendency toward quick, unplanned reactions to any stimulus without considering the negative consequences of those reactions.22 Impulsivity is one of the diagnostic criteria for hypomanic or manic episodes as defined by the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV).23 Elevated impulsivity is more frequently observed in BD patients than in the general population.24,25 Elevated impulsivity is not only related to suicide attempts and drug abuse among patients with BD but can also cause functional impairment.26-28 Furthermore, impulsivity remains high in BD patients even during remission.24-26,29-32 Therefore, elevated impulsivity may be a trait characteristic rather than a state characteristic of patients with BD.25
The current study investigated the relationship between impulsivity and QoL in euthymic BD patients. This study also examined which clinical variables, including impulsivity, contribute to poor QoL in BD patients.
METHODS
Participants
Patients with BD enrolled in this study were inpatients or outpatients in the Department of Psychiatry of Gyeongsang National University Hospital from May 2009 to December 2011. Psychiatrists diagnosed patients with BD according to DSM-IV criteria23 using a non-structured clinical interview. The criteria for inclusion in this study were 1) BD-I or BD-II diagnosis; 2) age between 18 and 65 years; and 3) remitted or recovered at the time of enrollment. Exclusion criteria were 1) diagnosed organic mental disorder; 2) mental retardation; 3) lifetime/current personality disorder; 4) concurrent alcohol and/or other substance abuse/dependence; and 5) presence of any other serious medical condition. The Institutional Review Board of Gyeongsang National University Hospital approved this study (approval number GNUH201301011).
Methods
In this study, remitted or recovered BD patients were recruited. The definition of remission or symptomatic recovery was based on the International Society for Bipolar Disorders (ISBD) Task Force report on the nomenclature of course and outcome in bipolar disorders.33 For inpatient participants, the Clinical Global Impression (CGI) assessment was administered weekly, and remission status was defined as a CGI score ≤2 for at least 2 weeks.33 For outpatient participants, symptomatic recovery was defined as a CGI score ≤2 for at least 2 months.33 Because inpatient participants are discharged from the hospital as soon as possible after remission from the acute episode of depression or mania, we could not recruit inpatient participants who had been in remission for at least 2 months, which was the criterion for outpatient participants. For this reason, we used different cutoffs for inpatient and outpatient participants with regard to remission of and recovery from BD. A total of 56 patients, 35 inpatients and 21 outpatients, were selected to participate in the study. All participants completed the Barratt Impulsiveness Scale (BIS) and the World Health Organization Quality of Life Assessment Instrument-Brief Form (WHOQoL-BREF). The Young Mania Rating Scale (YMRS) was used to assess manic or hypomanic symptoms. Semi-structured interviews were conducted to assess age of BD onset, number of past mood episodes, number of hospitalizations, family history, and presence of past psychotic symptoms.
Measures
BIS
The BIS was developed in 1959 to assess impulsivity. This test consists of three subscales34: 1) Attention Impulsivity, 2) Motor Impulsivity, and 3) Non-planning Impulsivity. The BIS-11 used in this study consisted of 30 questions from the eleventh edition of the scale. Total BIS scores generally range from 50 to 60 in healthy controls.35-37 The BIS-11 was translated into Korean by the authors. Because the BIS-11 Korean Translated Version was not verified for validity and reliability, internal coherence and test-retest reliability were assessed for the current study (22 respondents, average of 7 weeks in the test-retest period). The Cronbach's alpha coefficient was 0.77, and the intraclass correlations between test and retest scores for all of the individual items were statistically significant.
WHOQoL-BREF
To create a transculturally applicable QoL rating scale, the WHO created the WHOQoL-100 through contributions from 15 international centers.38 A shortened version of the WHOQoL-100 was developed for ease of application in clinical practice. Although an abridged version, this scale was created to properly assess the various QoL dimensions.39 The WHOQoL-BREF scale consists of 26 questions covering physical health (seven items), psychological health (six items), social functioning (three items), and environmental domains (eight items). A higher score indicates better QoL. The WHOQoL-BREF has been used in several studies assessing QoL among BD patients.40 QoL total scores generally range from 3.18 to 3.78 in healthy controls.16,41 The reliability and validity of this scale using Korean samples have been confirmed.42
Statistical analyses
Pearson correlation analyses were performed to assess the relationship between QoL total and subscale scores and various clinical variables including age, years of education, impulsivity, duration of illness, age of onset, number of past depressive episodes, number of hospitalizations, GAF score, and CGI score. Univariate regression analyses were performed to assess the relationship between QoL total and subscale scores, on the one hand, and each clinical variable, including BD subtype and history of suicide attempts, on the other. Significant variables from the correlation and univariate regression analyses (p-value<0.20), together with age, gender, and CGI score, were used as independent variables, and QoL total and subscale scores were treated as dependent variables in the multiple linear regression analysis. All statistics were analyzed using PASW Statistics version 18.0 (Chicago, IL, USA). In all cases, a two-tailed p-value<0.05 was considered statistically significant.
RESULTS
Demographic and clinical characteristics
Participants' sociodemographic and clinical characteristics are presented in Table 1. The average total impulsivity score was 61.48 (SD=8.95); the average subscale scores were 14.57 (SD=3.64) for attention impulsivity, 20.46 (SD=3.80) for motor impulsivity, and 26.45 (SD=5.18) for non-planning impulsivity. Based on the WHOQoL-BREF scale, the average QoL total score was 3.25 (SD=0.58), and the individual subdomain average scores were 24.21 for physical QoL (SD=4.54), 19.27 for psychological QoL (SD=3.99), 9.23 for social QoL (SD=2.30), and 25.25 for environmental QoL (SD=5.65).
Association of clinical variables with QoL
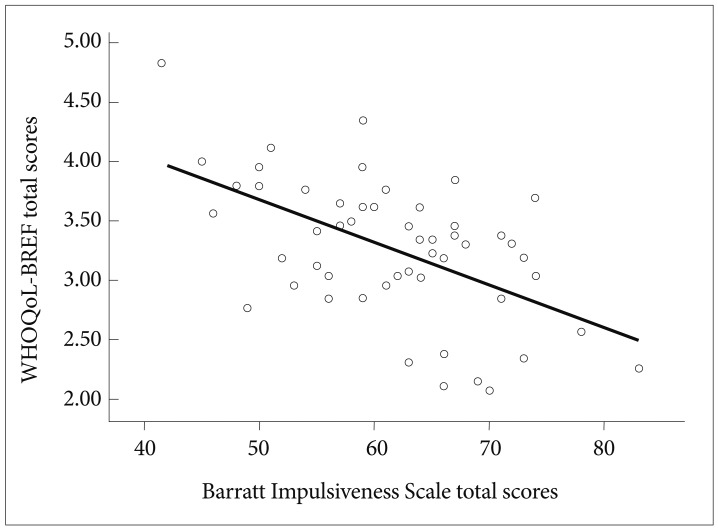
As shown in Table 2, QoL total scores were significantly associated with length of education (r=0.374, p=0.005), GAF score (r=0.509, p<0.001), CGI score (r=-0.283, p=0.034), total BIS score (r=-0.550, p<0.001)(Figure 1), and scores on all impulsivity subscales. Regarding the QoL subdomains of the WHOQoL-BREF, physical QoL was significantly associated with length of education (r=0.396, p=0.003), GAF score (r=0.461, p<0.001), CGI score (r=-0.288, p=0.032), total BIS score (r=-0.568, p<0.001) and scores on all impulsivity subscales. Psychological QoL was significantly correlated with length of education (r=0.307, p=0.022), GAF score (r=0.484, p<0.001), total BIS score (r=-0.550, p<0.001) and scores on all impulsivity subscales. Social QoL was significantly related to number of hospitalizations (r=-0.271, p=0.048), GAF score (r=0.324, p=0.015), total BIS score (r=-0.345, p=0.009), attention impul sivity (r=-0.307, p=0.021), and motor impulsivity (r=-0.280, p=0.036). Environmental QoL was related to length of education (r=0.320, p=0.016), number of hospitalizations (r=-0.330, p=0.015), GAF score (r=0.411, p=0.002), total BIS score (r=-0.360, p=0.006) and non-planning impulsivity (r=-0.310, p=0.020). History of suicide attempts had a marginally significant association with psychological QoL (F=3.816, df=1, p=0.056, adjusted R2=0.051) in the univariate regression analysis. In a separate univariate regression analysis, BD subtype had a statistically nonsignificant relationships to physical (F=2.523, df=1, p=0.118, adjusted R2=0.027), psychological (F=2.512, df=1, p=0.119, adjusted R2=0.027), social (F=0.021, df=1, p=0.885, adjusted R2=-0.018), and environmental (F=0.877, df=1, p=0.353, adjusted R2=-0.002) QoL.

Correlations between World Health Organization Quality of Life Assessment Instrument-Brief Form (WHOQoL-BREF) and clinical variables
Multiple linear regression models between clinical variables and QoL
Clinical variables that had significant associations with the QoL total and/or subdomain scores according to the Pearson correlation and univariate regression analyses (p-value<0.20), together with age, gender, and CGI score, were used in the multiple linear regression analyses. First, the QoL total score was used as the dependent variable; age, gender, years of education, total BIS score, GAF score, CGI score, and number of hospitalizations were entered as independent variables. Only the total BIS score (β=-0.43, p=0.001) was predictive of the QoL total score, explaining 41.5% of the variance in QoL (F=6.368, df=7, p<0.001, adjusted R2=0.415). In a separate analysis, we used physical QoL as a dependent variable. Age, gender, years of education, total BIS score, GAF score, CGI score and BD subtype were used in this second model. Again, only the total BIS score (β=-0.50, p=0.001) was predictive of physical QoL, explaining 41.8% of the variance in physical QoL (F=6.632, df=7, p<0.001, adjusted R2=0.418). Then, psychological QoL was entered as the dependent variable in a separate regression analysis. Age, gender, years of education, total BIS score, GAF score, CGI score, BD subtype, number of past depressive episodes, and history of past suicide attempts were entered as independent variables. Only the total BIS score (β=-0.38, p=0.010) was predictive of psychological QoL, explaining 24.9% of the variance in the psychological QoL (F=2.883, df=9, p=0.010, adjusted R2=0.249). Next, social QoL was entered as the dependent variable, and age, gender, years of education, total BIS score, GAF score, CGI score, and number of hospitalizations were entered as independent variables in a separate regression analysis. Once more, only the total BIS (β=-0.29, p=0.047) score was predictive of social QoL, explaining 17.4% of the variance in the social QoL (F=2.592, df=7, p=0.024, adjusted R2=0.174). Finally, environmental QoL was entered as the dependent variable, with age, gender, years of education, total BIS score, GAF score, CGI score, and number of hospitalizations entered as independent variables in the last regression model. Here, only the number of hospitalizations (β=-0.29, p=0.029) was predictive of the environmental QoL, explaining 25.3% of the variance in the environmental QoL (F=3.568, df=7, p=0.004, adjusted R2=0.253).
DISCUSSION
The current study explored the relationships of multiple clinical variables, including impulsivity, to QoL among remit ted or recovered patients with BD. The main findings of this study are as follows. First, high impulsivity was associated with low QoL across euthymic BD patients. Additionally, three impulsivity subscales were all significantly related to QoL. Second, despite controlling for overall functioning and several factors associated with QoL, impulsivity was independently associated with QoL. Third, impulsivity, along with physical, psychological, and social domains of a multi-dimensional QoL scale, were particularly relevant.
In this study, the impulsivity total score was related to the QoL total score and to the three QoL subdomains. In our multiple regression analyses, impulsivity was predictive of physical, psychological, and social domains of QoL. These results are consistent with results from previous studies.21 It must be noted that the influence of mood symptoms was minimized in the current study because the target subjects were patients in remission or recovery.
Recent studies of patients with BD demonstrated that elevated impulsivity was associated with overall functional impairment.28 This functional impairment has the potential to affect QoL among patients with BD. However, the current study showed that even when overall level of functioning was controlled, high impulsivity was independently related to QoL and subdomains of QoL. In other words, impulsivity can influence QoL through mechanisms distinct from functional impairment. Therefore, the results of the current study suggest that to improve QoL among patients with BD, it is not only necessary to restore functioning but also to control elevated impulsivity. However, the current study did not evaluate the level of functioning across a variety of areas. Instead, we used a single functional assessment tool, namely the GAF. The GAF might be influenced by symptoms as well as by the level of functioning. If symptoms are not evident, GAF sensitivity might be lower. Future research is needed to investigate whether impulsivity has an independent effect on QoL after controlling for the level of functioning across a variety of areas.
Many studies have suggested that patients with BD show neurocognitive impairments in sustained attention, verbal memory, and executive functioning not only during acute mood episodes but also during euthymia.43-48 In this study, the impulsivity subscale of an attentional measure showed a significant negative correlation with almost all QoL subdomains. Given that attentional impulsivity, a subscale of the BIS-11, involves a tendency to shift attention quickly,34 our results support previous findings that neurocognitive impairment is associated with poor psychosocial functioning and lower QoL in patients with BD.49,50
Regarding the correlations between the subscales of impulsivity and the subdomains of QoL, both the physical and psychological domains of QoL were related to the three subscales of impulsivity, and the social domain of QoL was related to the two subscales of impulsivity. In contrast, the environmental domain of QoL was related to only one impulsivity subscale. Furthermore, the regression analysis did not reveal a significant association between the environmental domain and impulsivity. This suggests that the influence of impulsivity is least evident in the environmental domain of QoL. It is not surprising that the psychological domain, which reflects positive/negative thoughts, self-esteem, body image, and personal beliefs, would be more closely related to impulsivity than would the environmental domain. Additionally, decreased psychological QoL was reported in patients with BD and comorbid substance dependence,16 which is directly related to impulsivity.26 Therefore, the results of the current study suggest that the specific predictors of the environmental QoL subdomain are likely quite different from those of the other QoL subdomains. Further research is warranted to replicate this finding.
Most of the known associated demographic and clinical variables were not related to QoL in our sample. However, impulsivity and number of hospitalizations did contribute to QoL. Demographic variables such as gender and age were not related to QoL; these findings are congruent with previous research.10 The age of onset and duration of illness were not related to QoL. The average age of onset for subjects in this study was 28.16 years (SD=9.81), relatively older than the known age of onset for BD.51 Using the age of onset for major mood episodes, rather than the age at which mood-related symptoms first appeared, would have probably affected the results of the current study. However, as a previous study suggested that age of onset and duration of illness were not associated with QoL,10 further studies are needed to examine how age of onset and duration of illness are related to QoL in more detail.
The current study had some limitations. First, because our patients were recruited at a tertiary university hospital, generalizing our results to other BD samples may be difficult. Second, recall bias may have occurred as a result of using a retrospective method to evaluate the age of onset, the number of mood episodes, and other clinical variables. Third, the limited number of participants may have affected the statistical validity of our results. Fourth, outpatient participants were in remission for at least 2 months, whereas inpatient participants were in remission for at least 2 weeks. Thus, in some cases, especially for hospitalized patients, the influence of subsyndromal mood symptoms on impulsivity and QoL cannot be completely ruled out. In this study, however, we minimized the influence of subsyndromal symptoms by controlling the CGI score in the multiple linear regression analyses. Fifth, Axis I and II disorders were diagnosed using non-structured clinical interviews instead of the structured clinical interview for DSM-IV Axis I and II (SCID-I, SCID-II).
Despite these limitations, one strength of this study was our observation of a relationship between impulsivity and QoL in remitted and recovered patients with BD. Additionally, impulsivity was independently associated with QoL even after controlling for several variables previously shown to affect QoL among patients with BD. Our findings suggest that clinicians should assess the impulsivity of BD patients in routine clinical practice.
In the future, treatment for bipolar disorder should focus on improving QoL rather than simply on improving mood symptoms. 52 To improve QoL, treatment programs must be developed to properly manage patients' impulsivity. Furthermore, additional research is needed to test whether regulating or adequately controlling impulsivity will improve patients' QoL.