How Childhood Maltreatment Is Related to Suicidality, Bipolarity and Central Serotonergic Activity in Patients with Major Depressive Disorder: A Cross-Sectional Pilot Study
Article information
Abstract
Objective
The aims of this study were to determine whether childhood maltreatment contributes to the occurrence of major depressive disorder (MDD) with bipolarity, and whether there is a relationship between central serotonergic activity, as assessed using loudness dependence of auditory evoked potentials (LDAEP), and childhood maltreatment.
Methods
Thirty-five MDD patients were stratified according to the presence or absence of childhood trauma into two subgroups, childhood trauma (CT) and no childhood trauma (NCT), using the Korean version of the Childhood Trauma Questionnaire (K-CTQ). The CT group was subjected to further analysis. Several psychometric ratings were also applied. In addition, auditory processing for the loudness dependence of auditory evoked potentials (LDAEP), which was used as a marker of serotonergic activity, was measured before beginning medication.
Results
There was a significant difference in total Korean Bipolar Spectrum Disorder Scale score between the CT and NCT groups (t=-2.14, p=0.04). The total K-CTQ score was positively correlated with the total Beck Scale for Suicidal Ideation (BSS) score (r=0.36, p=0.036). In particular, emotional abuse was positively correlated with the total Barratt Impulsiveness Scale (r=0.38, p=0.026), BSS (r=0.38, p=0.025), and Hamilton Depression Rating Scale (HAMD) (r=0.36, p=0.035) scores. There was also a positive correlation between LDAEP and total Hypomania Personality Scale (r=0.49, p=0.02) and HAMD (r=0.58, p=0.004) scores within CT group.
Conclusion
The findings of this study support that there is a relationship between childhood maltreatment and bipolarity in patients with MDD.
INTRODUCTION
Childhood maltreatment, including sexual abuse (SA), physical abuse (PA), emotional abuse (EA), physical neglect (PN), and emotional neglect (EN), is one of the most severe public-health problems worldwide.1 Childhood maltreatment is known to affect mental health in later adulthood;2 it is related to increased risk of major depressive disorder (MDD), bipolar disorder (BD), anxiety disorder, and alcohol abuse in adulthood.34 In the case of MDD, significant interactions with additive and recessive 5-HTTLPR (which encodes the serotonin transporter) genetic models were found for overall severity of childhood maltreatment.5 Li and colleagues found that in addition to MDD, a significant number of patients with BD reported experience of childhood abuse and neglect.6 A recent meta-analysis also revealed that physically abused, emotionally abused, and neglected individuals have a higher risk of developing depressive disorders than their nonabused counterparts.2 This childhood maltreatment seems to reduce central serotonergic neurotransmission and influence the onset of psychiatric disorder in later adulthood.789
The loudness dependence of auditory evoked potentials (LDAEP), which is measured using auditory processing, has recently been introduced as a metric of serotonin activity.10 The results of preclinical/animal research have indicated the LDAEP is a reliable indicator of central serotonergic activity in mood disorder.11 The LDAEP has been identified as being inversely associated with central serotonergic activity, with a large LDAEP reflecting low serotonergic neurotransmission and vice versa.12 Thus, it was hypothesized that depressed patients with childhood maltreatment affected central serotonin neurotransmission, as assessed using LDAEP. In addition, to date there have been no reports of a relationship between childhood maltreatment and MDD with bipolarity or bipolar spectrum disorder, which has no manic or hypomanic episode but has the characteristics of BD.13 Patients exhibiting MDD with bipolarity have more psychopathology features, including impulsive ty and suicidal ideation, than those with MDD without bipolarity.1415
The aims of the present study were to determine whether childhood maltreatment contributes to the occurrence of MDD with bipolarity, and whether there is a relationship between central serotonergic activity, as reflected by LDAEP, and childhood maltreatment. This is the first study to evaluate the relationship between childhood maltreatment and bipolarity.
METHODS
In total, 35 outpatients aged between 18 and 65 years who met the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV)-text revision criteria for MDD were screened at Ilsan Paik Hospital between 2013 and 2014. Subjects who had psychotic symptoms, any additional mental disorders on axis I or II of the DSM-IV were excluded in order to remove bias except alcohol abuse. None of the subjects had a history of hypomanic or manic episodes. The following inclusion criteria were applied to enroll MDD patients in this study: 1) no history of antidepressant treatment within 3 months before first visiting our hospital, and 2) having total Beck Depression Inventory (BDI)16 and Hamilton Depression Rating Scale (HAMD)17 scores exceeding 19 and 16, respectively, prior to the treatment (moderate-severe depression). Auditory processing for the baseline LDAEP, which was used as a marker of serotonergic activity in our previous study,14 was evaluated by measuring the auditory event-related potential before beginning medication with serotonergic agents.
The cohort was stratified into two subgroups according to the presence of childhood trauma (CT group) and no childhood trauma (NCT group), using the Korean version of the Childhood Trauma Questionnaire (K-CTQ),1819 which classified patients as positive for a history of childhood maltreatment based on mild to moderate cutoff scores of the total KCTQ score (i.e., 41 points).20 The K-CTQ is a 28-item selfreport questionnaire that consists of five subscales of childhood maltreatment experience: PA, EA, SA, PA, and EN. Each subscale comprises five items that are rated on a 5-point Likert scale, from 1 (never true) to 5 (very often true). In addition, It is appropriate for adults as well as adolescents (aged 12 and over). The entire cohort was also stratified into the following two subgroups according to whether they had suffered no maltreatment or had suffered one or more types of maltreatment (i.e., no vs one or more maltreatments) based on the moderateto- severe cutoff scores of five subscales: EA, ≥13; PA, ≥10; SA, ≥8; EN, ≥15; and PN, ≥10.20
Depression severity was assessed using HAMD and BDI. The Barratt Impulsiveness Scale (BIS),21 Hamilton Anxiety Scale (HAMA),22 Beck Scale for Suicidal Ideation (BSS),23 Beck Hopelessness Scale (BHS),24 Hypomania Personality Scale (HPS),25 and the Korean version of the Bipolar Spectrum Disorder Scale (K-BSDS)2627 were also applied. In this study, the K-BSDS was used to classify patients as positive for bipolarity based on moderately probable cutoff scores (i.e., 13 points).26 The CT group was subjected to further analysis. The study protocol was approved by the ethics committee of Inje University Ilsan Paik Hospital, and written informed consent to participate was obtained from all patients before beginning the investigation.25
RESULTS
A comparison of the demographic and clinical variables between the CT and NCT groups, defined according to the total K-CTQ score, is presented in Table 1. The mean total K-BSDS score differed significantly between the NCT group (11.25) and the CT group (15.45; t=-2.14, p=0.04). With the exception of SA, the mean scores of each subscale were significantly higher in the CT than in the NCT group. The number of subjects with alcohol abuse was significantly higher in the CT than in the NCT group (p=0.024), as was the number of subjects with bipolarity (p=0.008).
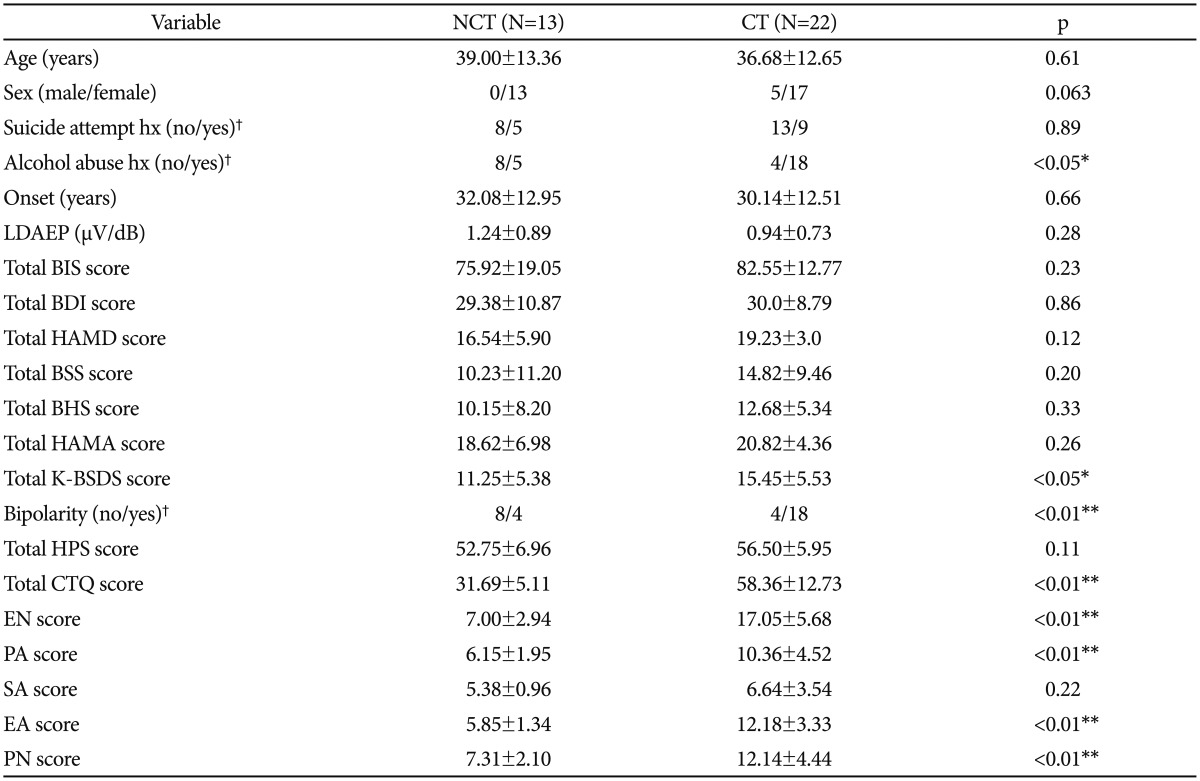
Comparison of demographic and clinical variables between the childhood trauma (CT) and no childhood trauma (NCT) groups, defined according to the cutoff (41 points) for the total Korean version of the Childhood Trauma Scale (K-CTQ) score
Table 2 presents the demographic and clinical variables among the subjects stratified according to the number of maltreatments suffered, defined according to the cutoff scores for the five K-CTQ subscales (i.e., EN, EA, PN, PA, and SA). The mean total BSS, BHS, and K-BSDS scores were significantly higher in the groups with one or more childhood maltreatments than in that without childhood maltreatment (BSS: t=-2.10, p=0.043; BHS: t=-2.52, p=0.017; K-BSDS: t=-2.94, p= 0.0061). The mean total K-CTQ scores and of each subscale, with the exception of SA, and the number of subjects with bipolarity (p=0.013) were significantly higher in the group with one or more childhood maltreatment than in the group without childhood maltreatment.
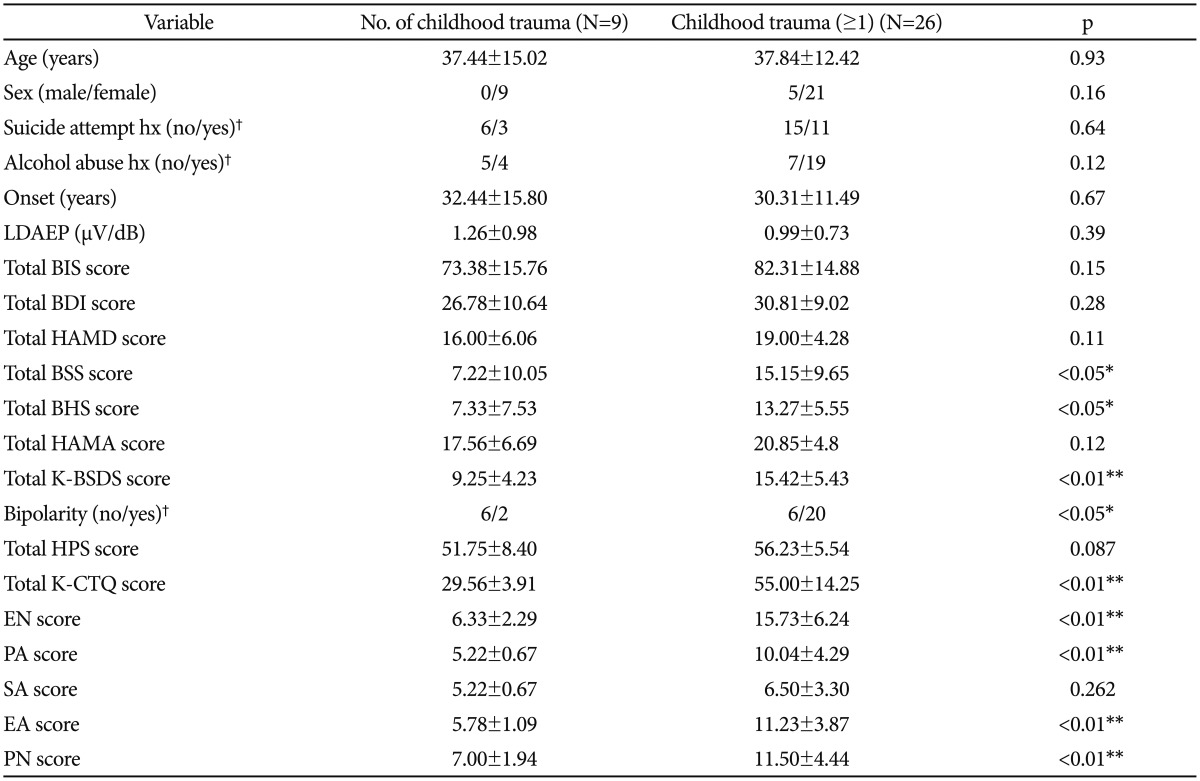
Comparison of demographic and clinical variables between the groups with and without any kind of childhood trauma defined according to cutoffs for five K-CTQ subscales
The total K-CTQ score was positively correlated with the total BSS score (r=0.36, p=0.036) (Figure 1). EA was positively correlated with the total BIS (r=0.38, p=0.026), BSS (r=0.38, p=0.025), and HAMD (r=0.36, p=0.035) scores. Patients with EA had higher BSS scores than those without EA (t=-2.77, p=0.009). EN was also positively correlated with the total BIS score (r=0.35, p=0.042). Finally, the number of subjects with alcohol abuse was also significantly higher in the PA group than in the group without PA (p=0.013).
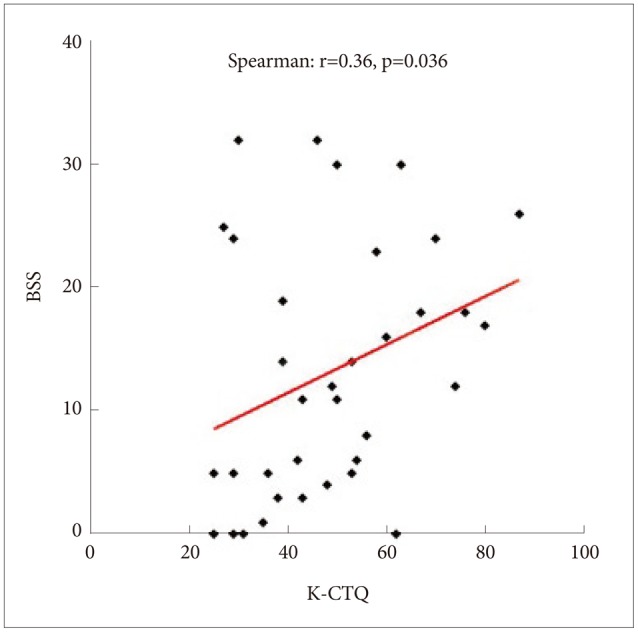
Correlation between the Korean version of the Childhood Trauma Questionnaire (K-CTQ) and Beck Scale for Suicidal Ideation (BSS).
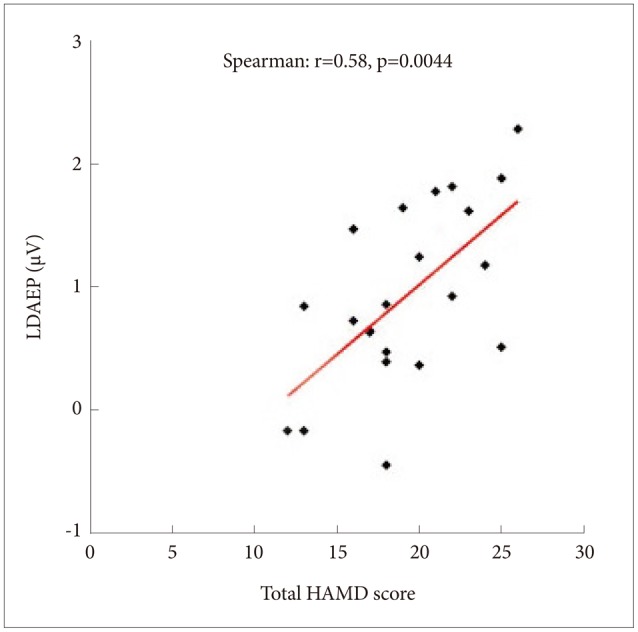
Further analysis of the CT group (n=22) total K-CTQ score was performed. There was a positive correlation between LDAEP and HPS score (r=0.49, p=0.02), but no correlation between LDAEP and K-BSDS score (r=0.37, p=0.091). In addition, there was a positive correlation between LDAEP and HAMD score (r=0.58, p=0.004) (Figure 2). The total K-CTQ score was positively correlated with the total BDI score (r=0.46, p=0.031). Finally, EA was positively correlated with the total BDI (r=0.48, p=0.021), BSS (r=0.56, p=0.007), and HAMA (r=0.49, p=0.022) scores.
DISCUSSION
This is the first pilot study to evaluate the relationship between childhood maltreatment and bipolarity, not BD. The patients in the CT group had a higher K-BSDS score than did those in the NCT group, although they had no hypomanic or manic episodes in their life and were not satisfied with even BD NOS. This means that childhood maltreatment or trauma is associated with both increased risk of bipolarity and BD. In addition, Ghaemi and colleagues proposed a definition for those patients who fall in the middle of the mood spectrum, between the classic unipolar and type I bipolar extremes, although it was controversial.1328 Thus, the present results may provide a clue as to the existence of a bipolar spectrum. Previous studies have already shown that childhood maltreatment was associated with an early age of onset, poor clinical course, suicidality, and substance abuse disorder in patients with BD.29 It was recently reported that exposure to childhood maltreatment potentiated the effects of recent stressors on adult mania.30 It was also reported that a significant number of patients with BD reported childhood maltreatment.6 Furthermore, compared to patients with unipolar depression, those with bipolar depression exhibited more suicidality, substance abuse, and impulsivity.28 In the present study, patients with one or more kinds of maltreatment had higher total BSS and BHS scores, and higher total K-BSDS scores as compared to MDD patients without any kind of maltreatment. This suggests that childhood maltreatment contributes to severe bipolarity or suicidality.
The total K-CTQ score was positively correlated with the total BSS score, and in particular, EA was positively correlated with the total BIS, BSS, and HAMD scores. These results show that the existence of childhood maltreatment was associated with worsening severity of illness and clinical course. Similarly, previous studies have demonstrated that childhood maltreatment is associated with the occurrence of psychiatric illness, including BD and MDD, with a potentially dose-dependent effect.31 Another study revealed that childhood trauma, including abuse or neglect, was associated with an increased risk of incident and recurrent mania, and that childhood trauma was associated with age at onset, and symptoms of postraumatic stress disorder and anxiety.6
Further analysis of the CT group revealed a positive correlation between EA and total HAMA and BDI scores. Thus, childhood maltreatment appears to affect anxiety levels in some individuals, as shown in another recent study.6 Regarding central serotonergic activity within the CT group, as depression severity elevated, the LDAEP also increased; in other words, central serotonergic activity decreased as the severity of depression increased. Similarly, previous study have shown that the LDAEP in patients is related to the severity of their depression, such that the more depressive they are, the stronger is their LDAEP, which reflects lower central serotonergic activity. In another study it was also indicated that there is a negative correlation between serotonergic activity and depression severity.14 In addition, some studies have demonstrated the existence of a relationship between childhood maltreatment and the serotonin system. A recent study found that the short variant of the serotonin transporter gene (5-HTTLPR) specifically sensitizes the effect of childhood maltreatment on whether adultonset depression leads to a chronic course.8 An interaction between 5-HTTLPR and a specific early environmental risk, such as SA or PA, has also been demonstrated in recurrent depressive disorder.5 Regarding central serotonergic activity within the CT group, as the HPS score increased, central serotonergic activity decreased, indicating that stronger bipolarity reflects lower serotonergic activity. In line with the present findings, Young and colleagues found decreased serotonin metabolite levels and turnover in patients with BD.32 However, BSDS score was not correlated with central serotonergic activity unlike HPS score in the present study. In addition, Wiste and colleagues found both norepinephrine and serotonin activities were lower in six suicides with BD compared to those with unipolar major depression.33 However, other studies have produced controversial and contradictory results.3435
The small sample in the present study limits the generalizability of the results. In addition, the K-BSDS is used only as a screening tool to help identify bipolarity, and not to analyze bipolarity itself. Notwithstanding these limitations, this is the first study to evaluate the relationship between childhood maltreatment and bipolarity.
In conclusion, the findings of this study support that there is a relationship between childhood maltreatment and bipolarity in patients with MDD. In other words, childhood trauma can be associated with both increased risk of bipolarity and BD. In future, more studies with larger cohorts are needed to confirm the findings.
Acknowledgments
This study was supported by a grant from National Research Foundation of Korea (NRF), funded by Ministry of Education (NRF-2014R1A1A2A10059345). The authors would like to thank Jo BW for her assistance with data collection.