Grief Response of Nursing Professionals Is Associated With Their Depression, Loneliness, Insomnia, and Work-Related Stress While Working in COVID-19 Inpatients Wards
Article information
Abstract
Objective
We aimed to explore whether nursing professionals’ psychological states affect their grief response for a patient’s death in the coronavirus disease-2019 (COVID-19) inpatients’ ward.
Methods
Survey was conducted among frontline nursing professionals working in COVID-19 inpatients wards at three tertiary-level affiliated hospitals of the University of Ulsan during April 7–26, 2022. Participants’ information such as age, years of employment, or marital status were collected, and their responses to rating scales including Pandemic Grief Scale (PGS) for healthcare workers, Stress and Anxiety to Viral Epidemics-9 items (SAVE-9), Patient Health Questionnaire-9 (PHQ-9), Loneliness and Social Isolation Scale, and Insomnia Severity Scale (ISI) were collected.
Results
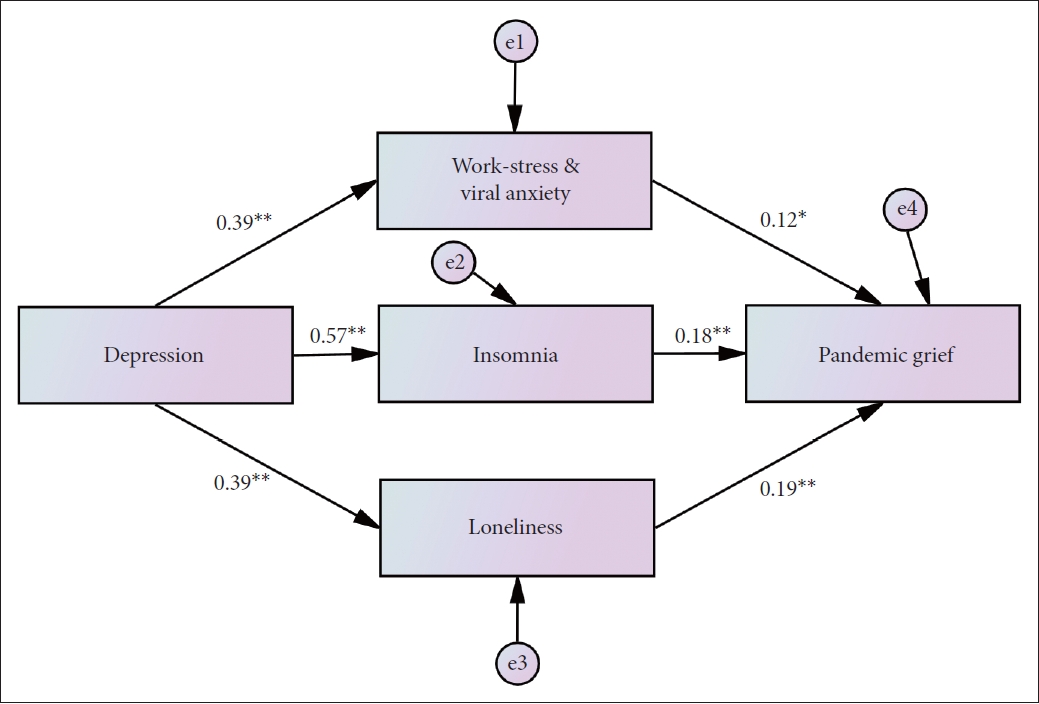
All 251 responses were analyzed. We observed that 34% reportedly suffered from depression. The linear regression analysis showed that a high PGS score was expected by high SAVE-9 (β=0.12, p=0.040), high PHQ-9 (β=0.25, p<0.001), high loneliness (β=0.17, p=0.006), and high ISI score (β=0.16, p=0.006, F=20.05, p<0.001). The mediation analysis showed that the depression of nursing professionals directly influenced their pandemic grief reaction, and their work-related stress and viral anxiety, insomnia severity, and loneliness partially mediated the association.
Conclusion
We confirm that frontline nursing professionals’ depression directly influenced their grief reaction, and their work-related stress and viral anxiety, insomnia severity, and loneliness partially mediated the association. We hope to establish a psychological and social support system for the mental health of nurses working in the COVID-19 wards.
INTRODUCTION
Through the coronavirus disease-2019 (COVID-19) pandemic, healthcare professionals, especially nursing professionals, are psychosocially affected by the uncertainty, workload, high risk of infection, and concerns about family members experienced during the COVID-19 pandemic [1]. More than a third of nurses suffered from psychological symptoms such as stress, anxiety, depression, and sleep disturbance [2]. A meta-analysis showed the prevalence of depression and anxiety as 22.8% and 23.2% among healthcare workers in COVID-19 pandemic [3]. The frontline nurses were particularly identified with high levels of stress, burnout, and moderate depression. COVID-19 has caused several challenges in nursing practice and nurses constantly face stressful situations that cause emotional exhaustion while providing complex treatment and care [1].
To prevent the spread of infectious diseases such as COVID-19, non-pharmacological interventions (e.g., social distancing) can be enforced in pandemic situations [4]. Therefore, physical distancing was also conducted in Korea [5] and the United States [6]. Reportedly, adherence to this physical distancing has also been associated with anxiety symptoms [7]. Some people try to maintain a strict social distance from others due to excessive stress and anxiety for the virus [8]. COVID-19 causes much psychological distresses such as stress, anxiety, and depression [9]. For example, during the COVID-19 outbreak, the wide increase of depression in Hubei province was confirmed [10]. In addition, the prolonged period of staying at home according to physical distancing rules was related to depression [7].
Anxiety for the pandemic and intolerance of uncertainty can influence depression. Intolerance of uncertainty can be defined as a way an individual perceives and responds to information in uncertain contexts [11]. This intolerance of uncertainty is related to the level of the general anxiety symptoms [12]. Generally, intolerance of uncertainty is considered as a cognitive vulnerability factor in the development and maintenance of anxiety [13]. Therefore, the intolerance of uncertainty and viral anxiety might influence adherence to physical distancing. However, the intolerance of uncertainty is a known risk factor for the development of depression [14]. Consequently, depression can inhibit the adherence to physical distancing [15]. Therefore, to explore whether the intolerance of uncertainty influences depression is meaningful.
Healthcare workers’ loneliness also should be explored. Perlman and Peplau [16] define loneliness as a mental, unpleasant, and distressed situation that results from a discrepancy between one’s expected level of social relationships and the actual conducted level of connectivity. As physical distancing prevents going to school or work and avoids face-to-face contact, it can affect the loneliness felt by individuals. During pandemics such as SARS [17] or COVID-19 [18], the quarantine policy significantly relates to loneliness, which is closely related to various risk factors of loneliness. For example, loneliness caused by COVID-19 more likely occurred in young people [19], while having a job or living with one’s spouse decreases the chance of loneliness [20]. Therefore, loneliness can raise risks such as depression and anxiety [21]; however, its management and further evaluation are required in a pandemic.
Psychological distress is a new issue to emerge in the pandemic era. Experts mention that this feeling of adapting to the pandemic is similar to grief, and one can experience emptiness and sadness [22]. In addition to this personal grief, healthcare workers can also experience professional grief caused by patients’ death due to COVID-19 infection in a medical environment [23]. Nurses in COVID-19 wards are more frequently exposed to these situations. Reports also state that restrictions due to social distancing also raise the possibility of a complicated grief [23]. Therefore, in the context of COVID-19, it may be important to evaluate the combined grief that nurses can experience and provide psychological support.
In this study, we aimed to explore whether nursing professionals’ psychological states affect their grief response for a patient’s death in the COVID-19 inpatients’ ward. We hypothesized that 1) depression will be positively related to grief response, 2) viral anxiety will be positively associated with grief response, 3) loneliness will be positively associated with grief response, 4) insomnia will be positively associated with grief reaction, and 5) psychological state will at least partially mediate the relationships between depression and grief response of nursing professionals working in COVID-19 inpatients ward.
METHODS
Participants and procedure
The researchers studied frontline nursing professionals working in COVID-19 inpatients wards at three tertiary-level affiliated hospitals of the University of Ulsan during April 7–26, 2022, which included Asan Medical Center in Seoul, Ulsan University Hospital in Ulsan, and GangNeung Asan Hospital in Gangneung, South Korea. Participant age, sex, and marital status were obtained, and no identifiable personal information was collected. Moreover, we collected information about COVID-19, such as “Have you witnessed any deaths from COVID-19 while working in COVID-19 inpatient wards?” “Have you been quarantined due to COVID-19 infection?” “Did you get infected with COVID-19?” and “Have you been vaccinated against COVID-19?” We also examined their past psychiatric history and current distress. The e-survey form was designed according to the Checklist for Reporting Results of Internet e-Surveys guidelines [24], and investigators verified its usability and technical functionality before implementation. A total of 339 nurses worked in COVID-19 inpatient wards in each hospital (239 in Asan Medical Center, 150 in Ulsan University Hospital, and 50 in GangNeung Asan Hospital), and we collected responses from 60% (n=203) of all eligible population. After excluding inappropriate or incomplete responses, 251 responses (134 in Asan Medical Center, 93 in Ulsan University Hospital, and 25 in GangNeung Asan Hospital) were finally analyzed from the 266 collected (143, 94, and 29, respectively).
The three Institutional Review Boards approved the study protocol, and each waived the written informed consent for the study (Asan Medical Center: 2022-0323; Ulsan University Hospital: UUH 2022-02-016-003; and GangNeung Asan Hospital: 2022-03-003-001).
Symptom assessment
Pandemic Grief Scale for healthcare workers
The Pandemic Grief Scale (PGS) for healthcare workers is an adapted version of the PGS, a self-report rating scale for assessing grief reactions in the COVID-19 pandemic [25] for healthcare workers. The original investigator of the PGS revised the scale for healthcare workers. The PGS for healthcare workers includes 5 items that are scored on a 4-point scale (0: not at all; 3: nearly every day). The higher total score means the probability of a dysfunctional grief response of healthcare workers when they experienced the death of a patient of whom they took care. The original English version was translated into Korean version by a bilingual expert, and the Korean text was back-translated into English by another bilingual expert. A third bilingual expert checked both the original English version and the reversed translation to find subtle variations. In this study, we applied the Korean version of the scale, and Cronbach’s alpha among this sample was 0.89.
Stress and Anxiety to Viral Epidemics-9 items
The Stress and Anxiety to Viral Epidemics-9 items (SAVE-9) is a self-rating scale, which can measure work-related stress and viral anxiety specifically in response to viral epidemic [26]. It consists of 9 items which are rated on a 5-point Likert scale (0: never; 4: always). In this study, we applied the original Korean version of the SAVE-9 scale, and Cronbach’s alpha among this sample was 0.83.
Patient Health Questionnaire-9
The Patient Health Questionnaire-9 (PHQ-9) is a self-report rating scale developed to assess an individuals’ severity of depression [27]. It consists of 9 items which can be scored on a 4-point scale (0: not at all; 3: nearly every day). A higher total score reflects a severe degree of depression. In this study, the Korean version of the PHQ-9 (www.phqscreeners.com) was applied, and Cronbach’s alpha among this sample was 0.88.
Loneliness and Social Isolation Scale
The Loneliness and Social Isolation Scale (LSIS-6) is a selfreport rating scale developed to assess an individuals’ social isolation and loneliness [28]. It consists of 6 items, and each item can be rated on a 4-point scale. A higher total score means a higher level of loneliness and social isolation. The original Korean version of the LSIS-6 scale was applied in this study, and Cronbach’s alpha among this sample was 0.74.
Insomnia Severity Scale
An Insomnia Severity Scale (ISI) is a self-report rating scale developed to assess an individuals’ severity of insomnia [29]. All 7 items in the ISI scale can be scored on a 5-point Likert scale. A higher total score indicates a high level of insomnia severity. The Korean version of the ISI [30] was applied in this study, and Cronbach’s alpha among this sample was 0.88.
Statistical analysis
We conducted the statistical analysis using the SPSS version 21.0 for Windows (IBM Corp., Armonk, NY, USA) and Jamovi 2.2.5 (https://www.jamovi.org/). Clinical characteristics were summarized as mean± standard deviation, and the level of significance was defined as two-tailed p<0.05. To explore the factors for the nursing professional’s grief response, participants were categorized into two groups based on their PHQ-9 scores: depressed group (PHQ ≥10) and non-depressed group (PHQ <10). For comparisons between two groups, continuous variables and categorical variables were analyzed using the Student’s t test and chi-square test. A partial Spearman’s rank correlation was used to explore the correlation among age and rating scales (PGS, SAVE-9, PHQ-9, loneliness, and ISI), using PHQ-9 as a control variable. A linear regression analysis was applied to see the influence of age and each variable (PGS, SAVE-9, loneliness, and ISI) on depression. Finally, to scrutinize the mediating effect of work stress and viral anxiety, insomnia, and loneliness on the relationship of depression to pandemic grief, a bootstrap method with 2,000 resamples was implemented among all participants.
RESULTS
Of 251 participants, 166 (66.1%) responded with less than 10 points for PHQ-9 (non-depressed group) and 85 (33.9%) responded with 10 points for PHQ-9 or higher (depressed group). There was no difference for sex, age, religion, years of employment, or marital status between two the groups. Also, regarding these questions on COVID-19 and psychiatric history, the two groups showed no meaningful gap for their responses to “Are you taking care of COVID-19 infected patients?” “Did you experience being infected with COVID-19?” “Did you experience being quarantined due to infection with COVID-19?” “Did you get vaccinated?” or “Did you have experience or treated depression, or insomnia?” However, there were some differences for questions (non-depressed vs. depressed) “Have you ever experienced the death of a COVID-19-infected patient that you took care of yourself?” (p=0.012), and “Now, do you think you are depressed or anxious, or do you need help for your mood state?” (p<0.001). In addition, they showed differences for PGS (p<0.001), SAVE-9 (p<0.001), PHQ (p<0.001), loneliness (p<0.001), and ISI (p<0.001) (Table 1).
The partial correlation analysis adjusting depression showed that old age was related to high loneliness (r=0.26, p<0.01). A high PGS score was significantly correlated with SAVE-9 (r=0.30, p<0.01), PHQ-9 (r=0.47, p<0.01), loneliness (r=0.35, p< 0.01), and ISI (r=0.40, p<0.01). The SAVE-9 score was correlated with PHQ-9 (r=0.39, p<0.01), loneliness (r=0.14, p<0.05), and ISI (r=0.29, p<0.01). The PHQ-9 score was correlated with loneliness (r=0.39, p<0.01) and ISI (r=0.57, p<0.01). Loneliness was significantly correlated with ISI (r=0.27, p<0.01) (Table 2).

Partial correlation coefficients of each variable in nursing professional working in COVID-19 inpatients ward (N=251)
The linear regression analysis, which was conducted to explore which variables expect the grief reaction of nursing professionals who were working in COVID-19 inpatients ward, showed that a high PGS score was expected by high SAVE-9 (β=0.12, p=0.040), high PHQ-9 (β=0.25, p<0.001), high loneliness (β=0.17, p=0.006), and high ISI score (β=0.16, p=0.006, F=20.05, p<0.001) (Table 3). The mediation analysis showed that the depression of nursing professionals directly influenced their pandemic grief reaction, and their work-related stress and viral anxiety, insomnia severity, and loneliness partially mediated the association (Table 4 and Figure 1).

Linear regression analysis to explore variables expecting grief response of nursing professionals working in COVID-19 inpatients ward (N=251)
DISCUSSION
In this study, we aimed to explore whether nursing professionals’ psychological states affect their grief response for a patient’s death in the COVID-19 inpatients ward. We observed that 34% reportedly suffered from depression. Their pandemic grief responses were expected because of high levels of stress and viral anxiety, depression, loneliness, and insomnia severity. The depression directly influenced their grief reaction, and their work-related stress and viral anxiety, insomnia severity, and loneliness partially mediated the association.
Nurses, as medical professionals, see patients’ pain and death closely, and sometimes watch the bereaved families closely. In particular, nurses working in emergency departments or intensive care units (ICU) are more exposed to this environment [31]. Studies have shown that the prevalence of depression is higher in frontline healthcare workers facing COVID-19 patients than in general medical staffs [32]. The fact that grief response is associated with depression is closely correlated with the results of this study. Many literature reviews on nursing occupations directly related to the patient’s death are available, such as oncology [33] or ICU nurses [34]. In addition, support for their grief experienced in the field has been emphasized. A study conducted on palliative care providers in the COVID-19 situation also emphasizes the presence of communication and care for their grief [35]. However, studies on nurses in COVID-19 intensive wards under virus-induced health and job stress in pandemics are rare. The significance of this study is that we attempted to investigate the factors affecting pandemic gripe in nurses in the COVID-19 ward and found a significant relationship between depression and mourning responses. In this study, we confirmed the existence of a significant gap in grief response between the depressive and non-defensive groups. Therefore, we can expect that the grief response can be reduced by early intervention for depression.
There was a significant correlation between pandemic grief and viral anxiety response. If the anxiety is higher, it is more difficult to restore one’s life, because of the painful emotions endured in the grief situation. Resilience may also have mediated this reaction. It is known that the resilient nurse showed lower anxiety during COVID-19 [36]. In addition, resilience helps to adapt to the grieving process [37]. In the results of this study, the relationship between pandemic grief and anxiety may be a result reflecting these. In addition, the mediation of viral anxiety in the relationship between depression and pandemic grief also shows that the anxiety felt by individuals can indirectly affect the mourning response. In a pandemic situation, whether it is an anxiety about the self, people around them, or the situation, anxiety can act comprehensively and have a mediating effect.
During the pandemic, the prevalence of insomnia increased [38]. In addition, depression and anxiety also increased [39]. A bidirectional relationship exists between insomnia and depression [40]. This point is consistent with the result that depression has an effect on insomnia in the results of this study. In addition, sleep disturbance is well accompanied in the mourning response and weakens physical and mental health [41]. Owing to this point, it is thought that insomnia mediated the relationship between depression and pandemic grief.
Intense feelings of grief can isolate oneself from others. In this respect, there will be a significant association between loneliness and pandemic grief. In addition, in this study, loneliness was confirmed to mediate the relationship between depression and pandemic grief. It is known that social support has a positive effect on the grief [42]. Because social support having a positive effect on grief, it is expected that social support will affect the grief in lonely people with less social support. This result seems to be correlated with the fact that social support is known to exacerbate mental health [43].
This study has the following limitations. First, anxiety caused by the COVID-19 may have been underestimated because the COVID-19 period was quite long after COVID-19 and the survey was conducted after the survey population had been 100% vaccinated. Second, since the social distancing policy was alleviated for the “with COVID-19 policy” in Korea, depression caused by social distancing may have been estimated too low. Third, since the survey was conducted only for domestic nurses, it may be different from overseas social distancing policies and nurse working environments. Fourth, we have used the PGS for healthcare workers, which was newly developed [44] and not fully validated yet [45], in this study to examine their grief response by using the healthcare workers-specific grief scale. Interpretation should be done with caution. Lastly, there is a relatively large number of samples of female nurses. However, there is a lack of data for male nurse. Despite the above limitations, this study has the following meanings. First, it was confirmed which factors interact in the relationship between depression and grief of nurses during the pandemic period. This study can contribute to providing psychological support for grief through intervention in these factors. Second, it is meaningful in that this study was conducted on nurses only in the COVID-19 ward who have seen many COVID-19 patients and been exposed to patients dying. Finally, by studying the effect of depression on the grief of nurses in the COVID-19 ward and confirming the difference in mourning responses between the depressed group and the non-depressed group, the importance of their mental health was confirmed.
In conclusion, this study explored the significant correlation between grief response and depression of nurses working in COVID-19 wards in pandemic situations. We confirm the mediating effect of loneliness, insomnia, and work-related stress, which were not previously reported. Between the depressed and non-depressed groups, there were significant differences in pandemic grief, depression, work-related stress, loneliness, and insomnia. In addition, a significant correlation was confirmed between the psychological symptoms of nursing professionals. Through this study, we hope to establish a psychological and social support system for the mental health of nurses working in the COVID-19 ward.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
Seockhoon Chung, a contributing editor of the Psychiatry Investigation, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Author Contributions
Conceptualization: Jihoon Hong, Junseok Ahn, Jin Yong Jun, Jangho Park, Jeong Hye Kim, Young Rong Bang, Seockhoon Chung. Data curation: Jihoon Hong, C. Hyung Keun Park, Harin Kim. Formal analysis: Jihoon Hong, Seockhoon Chung. Funding acquisition: Jihoon Hong, Seockhoon Chung. Investigation: Seockhoon Chung. Methodology: Jihoon Hong, Youjin Hong, Junseok Ahn, Jin Yong Jun, Jangho Park, Young Rong Bang, Seockhoon Chung. Writing—original draft: all authors. Writing—review & editing: all authors.
Funding Statement
This work was supported by the Student Research Grant (2022-0629) of University of Ulsan, College of Medicine, Seoul, Korea.