The Effectiveness of Virtual Reality Intervention for COVID-19-Related Psychological Distress: A Systematic Review
Article information
Abstract
Objective
The prolonged coronavirus disease-2019 (COVID-19) pandemic is likely to cause psychological distress in people. This systematic review aimed to identify the effectiveness of virtual reality (VR)-based psychological intervention among individuals with psychological distress during the COVID-19 crisis. PubMed, Ovid MEDLINE, Cochrane Library, Web of Science, Embase, and PsycINFO databases were searched for articles published until July 2022.
Methods
The available citations were deduplicated and screened by two authors using the title and abstract information. Eligibility criteria were constructed according to the PICOT guidelines. Empirical studies of all designs and comparator groups were included if they appraised the impact of an immersive VR intervention on any standardized measure indicative of psychological distress (stress, anxiety, depression, and post-traumatic symptoms) or improvements in quality of life in participants, including COVID-19 patients, medical staff working with COVID-19 patients, and people who had experienced strict social distancing during the COVID-19 pandemic.
Results
The results were discussed using a narrative synthesis because of the heterogeneity between studies. Seven of the studies met the inclusion criteria. There were two randomized controlled trials and five uncontrolled studies on VR interventions.
Conclusion
All studies reported significant improvement in a wide range of psychological distress during COVID-19, ranging from stress, anxiety, depression, and post-traumatic symptoms to quality of life, supporting the efficacy of VR-based psychological intervention. Our results suggest that VR intervention has potential to ameliorate COVID-19-related psychological distress with efficacy and safety.
INTRODUCTION
Coronavirus disease-2019 (COVID-19), caused by the SARSCoV-2 virus, was first identified in Wuhan, China, in late 2019, and swiftly spread to the other countries. Subsequently, the World Health Organization declared the COVID-19 outbreak a global “pandemic” in March 2020 [1]. Since then, it has lasted for more than two years, forcing the world to face unprecedented medical, economic, and social challenges. Economic and psychological effects caused by social distancing and preventive measures against COVID-19, as well as physical health problems due to infection, have affected public mental health. Consequently, stress, anxiety, fear, depression, and post-traumatic stress related to COVID-19 are emerging as global issues [2-4].
The pandemic has had a harmful effect on public mental health, leading to psychological crises [5]. People are more likely to experience severe anxiety and depression due to the prolonged COVID-19 pandemic. It is likely to be a traumatic stressor for some high-risk mental health groups [6]. A domestic survey [7] on the psychological impact of COVID-19 reported that approximately 30% of participants experienced mild to moderate anxiety symptoms and peritraumatic distress, and more than 30% of participants had mild to moderate depressive symptoms.
The number of newly reported COVID-19 cases has been declining globally since the end of March, 2022 [8]. However, some of the patients with COVID-19 continue to experience serious and persistent physical and psychological aftereffects. COVID-19 patients may have been exposed to a life-threatening situation depending on the severity of the symptoms, and there is a risk that their mental health will deteriorate due to persistent aftereffects or stigma and hate responses to confirmed patients [9]. Healthcare workers are likely to have post-traumatic symptoms during the COVID-19 pandemic [10]. They not only have a high risk of infection but also continue to be exposed to long disasters, which are likely to cause severe stress and mental fatigue [11,12]. A quantitative study with nurses in Korea indicated that more than 50% of nurses who cared for COVID-19 patients were classified into post-traumatic stress risk groups, and most of them experienced psychological distress [13]. Imposing quarantine, such as social distancing, cancellation of mass gatherings, and school closures, are the most effective measures to prevent the spread of virus infection, while it is a risk factor for mental health problems [14]. People who have been placed under COVID-19 stay-at-home orders showed anxiety, fear, worry about the future, sleep problems, and increased suicidal ideation [15].
COVID-19 makes it difficult for people to receive face-toface medical and psychological support, forcing clinicians to deliver treatment via audio/videocalls, e-mail, or the Internet [16]. Given the deteriorating mental health due to isolation and physical distancing in the context of COVID-19, it is needed to address the inevitable mental health problem using digital technologies [17]. Online mental health interventions embedded in virtual reality (VR) are considered a promising solution [18]. VR is a technology that digitally furnishes a three-dimensional (3D) ambiance [19], and the virtual social world is a controlled environment experienced under the guidance of a therapist. The virtual environment allows participants to experience a sense of presence in an immersive, computer-generated, 3D interactive environment and to experience controlled delivery of sensory stimulation via a therapist, including visual, auditory, olfactory, and tactile cues [20]. VR therapy, which has recently been verified for its effectiveness, has high potential to be applied to COVID-19-related interventions. VR had various health usages during the pandemic including physical and cognitive rehabilitation, pain management, treatment of psychological disorders, and healthcare professional training [21]. Also, VR has the potential to facilitate remote therapies that can be more consistent, scalable, and available [22].
Different from traditional face-to-face psychotherapy, a combination of visual and auditory stimuli in VR can be used to create an immersive experience, which may reduce perceived distress and negative affect, and induce relaxation and positive affect [23]. VR interventions have been developed for various psychological and psychiatric conditions [24,25]. Notably, it makes individuals with post-traumatic stress disorder (PTSD) fully immerse in the traumatic scene and create an evocative environment that may augment a patient’s imaginative exposure with multi-sensational experiences [20,26]. Many studies have found that VR-based therapies may be effective for a broad range of mental disorders, including panic disorder [27], phobias [28], major depressive disorder [29], and PTSD [30]. Additionally, VR interventions demonstrated effectiveness in case of natural disasters. VR-based interventions effectively alleviated PTSD symptoms, anxiety, and depression caused by natural disasters [31,32]. Metaanalysis studies have shown moderate to large effects of VR interventions compared to control conditions for anxiety and depression outcomes (e.g., waitlist, placebo, relaxation, and treatment as usual) [33], and a large effect size for VR therapy on anxiety disorders, which was comparable to in vivo conditions [34].
Prior studies revealed the potential of digital therapeutic technology like as immersive VR that offer cost-effective, scalable, and on-demand solution to address mental problems. Since COVID-19 era has prolonged yet, VR intervention has the potential strength to minimize face-to-face intervention [22]. Despite the growing importance and necessity of distant-delivered treatment or non-directive treatment for psychiatric problems in this pandemic era, there has not been much research related to VR interventions for COVID-19-related psychological distress [35]. Although various studies have found that VR-based therapies could be beneficial for various mental health disorders, there has been a paucity of information on whether beneficial effect of VR-based intervention could be generalized into patients and medical staff with COVID-19-related mental-health problems [36]. To the best of our knowledge, one systematic review study [36] conducted a systematic review of VR technology for the treatment of mental health problems during COVID-19. Despite the thoroughness of the findings of the first systematic review, Hatta et al. [18] had limitations in the selection bias and heterogeneity of the included studies. Therefore, this study aimed to overcome these limitations and review the literature by applying more sophisticated and rigorous standards. The main objective of this study was to identify the effectiveness of VR-based psychological intervention among individuals with psychological distress during the COVID-19 crisis.
METHODS
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. This review was registered under registration number CRD42022351974 in the International Prospective Register of Systematic Reviews (PROSPERO).
Search strategy
Search strategies were developed in collaboration with a research team and an experienced librarian. Keywords related to VR and COVID-19-related psychological distress were developed by the research team, and a librarian searched the following electronic databases: PubMed, Ovid MEDLINE, Cochrane Library, Web of Science, Embase, and PsycINFO. A database search was conducted on July 22, 2022. We used the following search terms: (COVID 19 OR SARS-CoV-2) AND (psychological distress OR anxiety OR depression OR stress, psychological OR quality of life OR COVID-19 stress syndrome) AND (virtual reality exposure therapy OR virtual reality). Furthermore, a search for registered clinical trials (clinicaltrials. gov), grey literature, and references of the included studies was conducted to identify potentially relevant studies. The search strategy is presented in Supplementary Material (in the online-only Data Supplement).
Eligibility criteria
Eligibility criteria were constructed according to the PICOT guidelines [37]. To be eligible for inclusion, the articles had to fulfill the following criteria. Regarding the population (P), the criteria included adults experiencing COVID-19-related psychological distress. The participants included COVID-19 patients, medical staff working with COVID-19 patients, and people who had experienced strict social distancing during the COVID-19 pandemic. No age, sex, race, or ethnicity were applied. For intervention (I), psychological intervention studies using VR were included. For comparison (C), studies using the treatment as usual or waitlist group as a control group (controlled studies), or studies using baseline (pre-intervention) as a control condition (uncontrolled studies) were included. Outcomes (O) included reductions in psychological distress (e.g., stress, anxiety, depression, and post-traumatic symptoms) or improvements in quality of life. For study type (T), only peerreviewed original articles using the following study designs were considered: cohort studies, before-and-after studies, casecontrolled studies, and randomized controlled studies.
Exclusion criteria included 1) psychological distress unrelated to COVID-19; 2) non-psychological interventions using VR (e.g., VR tour); and 3) studies that did not report the outcome of interest. In addition, the following studies were excluded: reviews, case reports, commentaries, letters to the editor, daily reports, books, protocol registrations, and abstracts without full text.
Selection process
All relevant citations were saved by the reference manager, EndNote. Two reviewers (SA Lee and S Heo) independently screened each citation according to the inclusion/exclusion criteria stated above. Eligibility of the studies was determined by reading the titles and abstracts of the retrieved articles. If there was insufficient information in the abstract regarding inclusion or exclusion, the full text was reviewed before the final decision. The results were compared to identify inconsistencies, and inter-examiner conflicts were resolved through discussion with a third reviewer (S Kim). A PRISMA flow diagram was used to organize and keep track of the numbers of studies that were included/excluded.
Data extraction
Three reviewers (SA Lee, S Heo, and S Kim) created a detailed table for data extraction using Microsoft Excel. Six evaluators (SA Lee, S Heo, S Kim, C Park, Y Jung, and G Ji) independently extracted data using a prespecified form. The first author, year of publication, study design, country, population characteristics, number of participants, age, intervention, control, and outcome were extracted from the included studies. In addition, data related to the VR intervention included its content, duration of intervention, total number of sessions, and whether it was combined with other treatments. Finally, three evaluators (SA Lee, S Heo, and S Kim) reviewed the data extraction results, and any disagreement regarding the extracted data was resolved by consensus among the reviewers.
Methodological quality appraisal
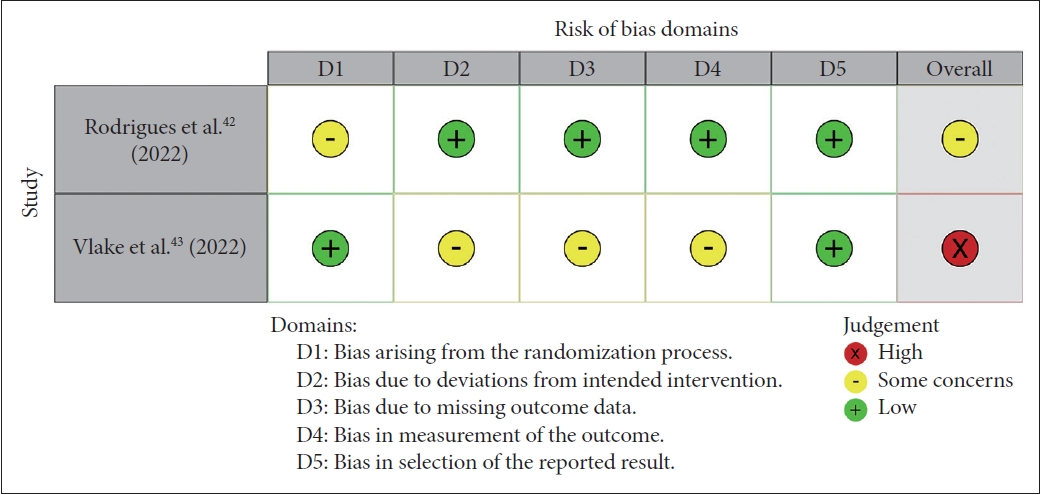
Two evaluators (SA Lee and S Heo) independently assessed the quality of all the included studies, and any discrepancies were resolved by a third evaluator (S Kim). As this review included studies using different designs, the relevant quality assessment tools were applied according to the study design. The risk of bias in randomized controlled trials (RCTs) was assessed using the revised Cochrane risk of bias tool for randomized controlled trial (RoB 2.0 [38]). In addition, the National Institutes of Health (NIH) quality assessment tool for before-after (prepost) studies with no control group [39] was used to evaluate the methodological quality of before-after studies without control groups. These are recommended as reliable and valid quality assessment tools and have been widely adopted in many systematic reviews [38,39]. The RoB 2.0 tool contains six domains: 1) bias arising from the randomization process, 2) bias due to deviations from intended interventions, 3) bias due to missing outcome data, 4) bias in measurement of the outcome, 5) bias in the selection of the reported result, and 6) overall bias. Each domain in RoB 2.0 comprises a series of signaling questions, and each question was rated as “yes,” “probably yes,” “probably no,” “no,” or “no information.” Once the signaling questions were answered, a risk-of-bias judgement was assigned one of three levels to each domain: low risk of bias, some concerns, and high risk of bias. The overall risk of bias was judged at three levels, depending on the level of risk for an individual domain.
The NIH quality assessment tool for before-after studies with no control group consisted of 12 questions: 1) study question; 2) eligibility criteria and study population; 3) study participants representative of clinical populations of interest; 4) all eligible participants enrolled; 5) sample size; 6) intervention clearly described; 7) outcome measures clearly described, valid, and reliable; 8) blinding of outcome assessors; 9) follow-up rate; 10) statistical analysis; 11) multiple outcome measures; and 12) group-level interventions and individual-level outcome efforts. Each question was evaluated as “yes,” “no,” “cannot determined,” “not applicable,” or “not reported.”
Data synthesis
The studies included in this review used heterogeneous populations (e.g., COVID-19 patients, COVID-19 medical staff, and people who had undergone strict social distancing during the pandemic) and included various outcomes such as stress, anxiety, depression, post-traumatic symptoms, and quality of life. Therefore, quantitative synthesis (meta-analysis) could not be performed due to clinical and methodological diversity in the included articles [40], and narrative synthesis was conducted.
RESULTS
Study selection
A flowchart of the data selection process is shown in Figure 1. Of the 630 articles that were initially imported for screening, 259 duplicates were excluded. A total of 371 studies were screened for titles and abstracts. A total of 132 studies on unrelated subjects, including orthopedic training, tourism industry, and animation course teaching, were excluded. By screening the full text of 239 studies, 232 articles were removed for the following reasons: non-relevant type of study including reviews, case reports, commentaries, and letters (n=136); nonrelevant population such as aviophobia patients, people with substance use disorders, people living with dementia, and people with autism (n=47); non-relevant interventions such as face-to-face therapy, online therapy in the group, virtual concerts, and gamification (n=35); non-relevant outcomes including a simple survey for satisfaction and perceived benefit of VR; a survey focused on providers’ use of telecommunication modalities and telehealth training and practice (n=5); and non-English (n=9). Finally, seven studies were included in this systematic review. The key results of this study are summarized in Table 1.

Flowchart of the selection strategy and inclusion/exclusion criteria for the systema-tic review according to PRISMA guideline.
Study characteristics summary
Among the seven studies included in the systematic review, in terms of population, three [41-43] out of seven studies were conducted on COVID-19 patients and two [44,45] on medical staff. Two studies [46,47] were conducted on people who had experienced strict social distancing during the COVID-19 pandemic. Regarding the intervention, most of the VR content contained calming natural scenery stimuli that induced relaxation. Groenveld et al. [41] used multimodal VR (physical, cognitive, and relaxation/distraction exercise), and the study by Vlake et al. [43] used COVID-19-related ICU (Intensive Care Unit) stimuli in a virtual environment, which was the only study using an exposure therapy component. The VR intervention time per session was reported to be approximately 10 minutes in four studies [42,43,46,47]. Additionally, 3-minute-VR was used in one study [44] and 30-minute-VR in another study [41]. The duration of VR intervention was one week in two studies [46,47] and six weeks in one study [41]. Only a single session was conducted in three studies [42-44], and one study [45] did not accurately report the duration.
Regarding study design, five [41,44-47] were within-subject-designed uncontrolled studies (pre-to post-intervention comparison), and two [42,43] were between-subject-designed controlled studies (intervention versus control group comparison). Among the five before-and-after studies, two studies [44,45] of COVID-19 medical staffs conducted pre-post comparisons using VR intervention only. However, since studies conducted on COVID-19 patients and those experiencing strict social isolation used a combination of VR intervention and social exercise [46,47], or/and cognitive exercise [41,46], it was difficult to clearly elucidate the effectiveness of VR intervention, except for other factors. Two RCT studies used a rigorous design to verify the efficacy of VR interventions; however, in the study by Rodrigues et al. [42], anxiety and depression were significantly reduced. A study by Vlake et al. [43] reported no significant improvement in clinical symptoms (anxiety, depression, and post-traumatic symptoms), except for quality of life.
Within-subjects-designed uncontrolled studies without comparison
Nijland et al. [45] conducted a pre-post intervention study with assessments immediately before and after VR relaxation sessions. The participants were 326 ICU nurses at the University Medical Centre Groningen working in one of the four ICU for COVID-19 patients. VR relaxation (VRelax), including videos of calming natural environments, lasted longer than 10 minutes. Participants were recommended to use VR for at least 10 min; however, actual use duration data were not collected. Primary outcomes were perceived stress and resilience, which were measured using the Visual Analog Scale-stress (VAS-stress), the Perceived Stress Scale 10 (PSS-10), and the 10-item Connor-Davidson Resilience Scale. After the VRelax sessions, the mean perceived stress level was lower than before the VRelax sessions.
Riva et al. [47] studied to investigate the effectiveness of a selfadministered at-home daily VR-based intervention (“COVID Feel Good”) for reducing the psychological burden experienced during the COVID-19 lockdown in Italy. Riva et al. [48] developed “COVID Feel Good” to help overcome the psychological burden of the coronavirus by relieving anxiety, improving well-being, and reinforcing social connectedness. It was a weekly self-help VR protocol based on the “Secret Garden” VR video online (www.covidfeelgood.com), which simulates a natural environment aiming to promote relaxation and self-reflection. Forty individuals who had experienced strict social distancing for at least two months participated in this study. The intervention lasted one week, and the intervention protocol consisted of two parts: the first part included 10 minutes VR video entitled “The Secret Garden,” which could be accessed through both an immersive modality (participants’ smartphone and a basic low-cost cardboard VR headset) and a non-immersive modality (the YouTube App); and the second part involved a week-long social exercise with a different topic every day. Regarding primary outcome measures, participants exhibited improvements from baseline to post-intervention for depression levels, stress levels, general distress, and perceived stress, but not for perceived hopelessness, which could be measured through a decrease in the Depression Anxiety Stress Scales (DASS), PSS-10, and Beck Hopelessness Scale (BHS).
Beverly et al. [44] performed a within subject pre-post study with 102 frontline healthcare workers, including direct care providers, indirect care providers, and support or administrative services. The protocol included the Tranquil Cine-VR simulation, which consisted of a video capture of a lush, green nature preservation, and runs in a three-minute session. The primary outcome was subjective stress, which was measured using VAS-stress. There was a significant reduction in stress scores from pre-to post-simulation. Participants who met the cutoff for high-stress pre-simulation showed a greater reduction in subjective stress scores compared to participants who did not meet the cutoff pre-simulation.
Groenveld et al. [41] examined the feasibility of self-administered VR exercises for COVID-19 patients in a communitybased practice or outpatient rehabilitation clinic in the Netherlands. Initially, 48 participants were enrolled; one patient did not start VR and seven patients withdrew mostly due to dizziness. Participants performed the multimodal VR exercises for 6 weeks, each lasting no more than 30 minutes, which consisted of VR physical exercises and VR mental exercises through applications to reduce stress and anxiety and promote cognitive functioning. Primary outcomes included anxiety, depression, and quality of life, which were measured using the Hospital Anxiety and Depression Scale (HADS), the Short Form-12 (SF-12), and the Positive Health questionnaire. There was a significant increase in the SF-12 score and positive health questionnaire after 6 weeks. The decrease in the total HADS score was not significant for the total group, but was significant for the subgroup of patients who used mental VR applications.
Meyer et al. [46] evaluated the online self-help protocol “COVID Feel Good” in 38 German samples who had experienced at least two months of strict social restriction. This study was conducted using a within-subject pre-post design with a waiting list. The 7-day self-help protocol included the 10 minutes VR video “Secret Garden” developed by Riva et al. [48] and social or cognitive exercise. This protocol aimed to reinforce coping skills, protect self-esteem, recognize emotional discomfort, find personal meaning even in difficult times, and revise core assumptions and beliefs. Primary outcomes were depression, anxiety, general stress, perceived stress, and hopelessness. The scales of outcome measurement were the DASS, Subjective Units of Distress Scale, PSS-10, and BHS. There was a statistically significant effect of time, displaying the difference between all primary outcomes except for hopelessness. Treatment effects on general distress, stress, anxiety, and depression persisted for two weeks after participation.
Between-subjects-designed controlled studies
A randomized study by Rodrigues et al. [42] evaluated whether VR contributes to the control of pain symptoms, sensation of dyspnea, perception of well-being, anxiety, and depression in patients hospitalized with COVID-19. The participants were enrolled from inpatient wards for patients with COVID-19 at four sites in Brazil and randomly assigned to two groups. Twenty-two patients in the intervention group underwent therapeutic VR video and occupational therapy, whereas the other 22 patients in the control group received non-therapeutic VR and occupational therapy. Therapeutic VR included videos with images of landscapes and/or mindfulness techniques to promote relaxation, distraction, and stress relief, whereas non-therapeutic VR included a video with advertisements not related to relaxation and well-being content. The primary outcomes were anxiety and depression, which were measured using HADS. Concerning the HADS, only the experimental group showed a difference from baseline to postintervention. Between-group differences were not observed.
Vlake et al. [43] conducted a multicenter randomized controlled trial. This study aimed to explore the effects of ICU-VR on mental health and on patients’ perceived quality of, satisfaction with, and rating of ICU aftercare among COVID-19 ICU survivors. The participants enrolled in a university teaching hospital and three university-affiliated secondary care hospitals were randomly assigned to either the intervention group (60-minute-consultation and ICU-VR intervention) or the control group (only consultation without VR intervention). The primary outcomes were anxiety, depression, post-traumatic symptoms, and quality of life. There was a non-significant improvement in the clinical symptoms, which could be measured through changes in assessed using the Impact of Event Scale-Revised, HADS, the Short-Form 36 (SF-36), and the European Quality of Life 5 dimensions in the experimental group. ICU-VR improved satisfaction with and overall rating of ICU aftercare compared with controls.
Methodological quality of the included studies
This systematic review included two RCT studies and five before- and-after studies with no control group, so that the quality assessment tool was mixed and used according to the study design. Five before-and-after studies with no control groups were assessed using the NIH quality assessment tool (Table 2). Two RCTs studies were evaluated using RoB 2.0 (Figure 2).

Risk of bias assessment using NIH quality assessment tool for before and after (pre-post) studies with no control group
As a result of the quality assessment, most studies included in this review had methodological limitations. First, five of the seven studies were before-and-after studies, which had insufficient designs to rigorously verify the effectiveness of the intervention. In particular, Nijland et al. [45], Beverly et al. [44], and Groenveld et al. [41] met only five of the 12 criteria. Specifically, the above three studies lacked participant representativeness and the sample size was not calculated to obtain statistical significance. In addition, the outcome assessor was not blinded using only the self-report scale, and follow-up loss was not properly managed. The low quality was also attributed to the fact that only pre- and post-tests were performed, and outcomes were not measured multiple times. In the before-andafter studies included in this review, Riva et al. [47] was the only study assessed to have a low risk of bias. On the other hand, there were only two RCT studies that used rigorous methodologies, and even then, the quality was assessed from some concerns [42] to a high risk of bias [43].
DISCUSSION
To the best of our knowledge, this is the first systematic review to provide an up-to-date overview of the effectiveness of VR-based psychological interventions in individuals experiencing psychological distress during the COVID-19 crisis. In total, there were seven studies eligible for this systematic review— two RCTs and five uncontrolled studies. We could not synthesize the data for a meta-analysis because of the heterogeneity between the studies; they had different populations, assessment tools, outcomes, and duration of studies. Instead, we conducted a systematic literature search of all accessible resources, minimizing selection bias and subjective selection bias.
The participant groups included COVID-19 patients [41-43], people who experienced strict social restrictions [46,48], and medical staff working with COVID-19 patients [44,45]. In the former two participant groups (COVID-19 patients and people who underwent strict social distancing), overall, significant improvement was reported in a wide range of psychological distress during COVID-19, ranging from stress, anxiety, depression, and post-traumatic symptoms to quality of life, supporting the efficacy of VR-based psychological intervention. However, in terms of treatment content, the studies that showed clearer effects were eclectic in that social or cognitive exercise [46,47], or occupational therapy [42] were combined with VR intervention, making it difficult to tease the efficacy of VR apart from other therapeutic modalities. In studies that utilized VR only [41,43], the beneficial effects were not pronounced or consistent in psychological distress (stress, anxiety, depression, or post-traumatic symptoms) or quality of life. In the medical staff working with COVID-19 patients, only two uncontrolled studies have been conducted in which post-treatment outcomes were compared to the pre-treatment baseline. They commonly used various calming natural environment images (e.g., lush and green nature preserve) as the background of VR [44,45]. In addition, they used VAS-stress scale for assess changes in stress levels, which showed a significant reduction in perceived stress.
In contrast to Hatta et al.’s [18] systematic review, which dealt with a similar topic, we applied a more rigorous approach to select eligible studies. The four VR treatment studies included in Hatta et al. [18] were excluded from our study due to problems with inclusion or outcome criteria. For example, participants were convenience sample of young adults recruited from an introductory university course [49] or inclusion criteria were not specifically described [50,51]. Although Kolbe et al.’s [52] study was a VR intervention for COVID-19 patients and health workers, they only analyzed outcomes regarding user experiences (e.g., satisfaction after VR intervention, intent for recommendation), which did not fit the outcome criteria. Yang et al. [51] focused on VR tours, which are not considered as psychological interventions for therapeutic purposes.
Taken together, our systematic review suggests future directions for studies that intend to utilize VR for COVID-19-related psychological distress. First, the development of VR content should be based on the current knowledge of core psychopathology and psychological sciences to be more effective. Most existing studies have shown participants peaceful or pleasant images (e.g., natural environments) in immersive VR modalities, lacking an active treatment component. Because nature-related stimuli are easily accessible and safe to most people and can effectively induce general positive emotions [47], they had the advantage of being universally available to a large population with heterogeneous symptoms. They also reaped some success in satisfying the increased mental service needs in a timely manner. However, these early VR interventions were apart from major streams of evidence-based treatment, partly because they were developed before empirical studies clearly described what constitutes the COVID-19-related psychological distress and which factors should be considered important as mechanism of treatment. This is a major caveat of existing studies that hinders further development of this area. To advance this field a step forward, there is a dire need for true confusion that synthesizes evidence-based treatment literature with VR technology. The success of VR exposure therapy for PTSD is a good example of how synergetic effects arise from meticulously combining therapeutic theory and innovative technology [53]. Many previous studies have shown that VR exposure therapy provides vivid, realistic virtual stimulation to increase participants’ immersion [54] and reduce participants’ dropout rate compared to traditional exposure therapy [30]. As such, VR technology can be effectively applied to exposure therapy, an evidence-based treatment for PTSD or anxiety disorders, so it is necessary to consider this when developing VR for COVID-19-related psychological distress in the future. Moreover, it is necessary to consider the heterogeneity in the experience of COVID-19-related psychological distress to develop VR interventions with adequate coverage and depth. As increased stress or anxiety was relatively common during the pandemic [3,5], VR stabilization techniques (e.g., containment, light stream, and sensory grounding) can satisfy the needs of the general population. In contrast, a VR intervention, like traditional VR exposure therapy with additional adaptation of VR-related scenarios, would be more conducive to vulnerable groups of individuals who continue to suffer from chronic, severe post-traumatic symptoms.
Second, seven studies included in the present systematic review have shown that VR is a feasible and acceptable innovative method to reduce psychological distress and improve quality of life in the place where the participants stayed (e.g., hospitals, ICU, workplaces, and home). This confirms that VR may serve as a reachable and immersive way to bring practical clinical interventions to hospitalized patients, health-related workers, and patients in the COVID-19 recovery phase, mainly during the ongoing COVID-19 pandemic. Future studies should focus on the fact that VR is necessary for a more traditional style of face-to-face consultation settings [52,55]. Moreover, most virtual environments in VR videos provided visual and auditory elements. Multimodal VR improves physical and cognitive function in post-stroke rehabilitation [41,56]. VR with added tactile and olfactory elements would be helpful in building a more realistic VR environment for interventions for psychological problems. In addition, the differences in the domain regarding efficacy might be due to the design of the VR intervention. Purpose-designed VR interventions seem to be more effective and will support the use of VR in personalized medicine [41,57]. VR relaxation has revealed that VR approaches have high patient satisfaction and benefits regarding psychological distress. A wide range of VR applications in different domains motivated participants to apply and improve treatment adherence and self-efficacy.
Third, from a methodological point of view, multiple issues must be addressed to provide higher-quality evidence. A small sample size may restrict the statistical power; therefore, the minimum number of participants per group should be determined in the power calculation analysis prior to data collection. The mean duration of VR intervention was inconsistent; hence, it was difficult to determine the optimal duration to maximize treatment outcomes and minimize cybersickness.
Lastly, existing studies mostly relied on self-reported data for assessing treatment outcomes, which can be criticized for validity. Therefore, diversifying measurements using physiological or behavioral data would be helpful to better capture treatment outcomes at different analytical levels. In addition, a long-term follow-up assessment is necessary to determine whether the treatment effect is enduring.
Overall, the existing studies had low methodological quality, and a meta-analysis was not possible due to high heterogeneity. Currently, the total number of VR-based psychological intervention studies was limited. There were only two RCTs, and their methodological quality was evaluated as “some concern” to “high risk of bias.” Therefore, well-designed RCTs with enhanced methodological quality are needed to test the efficacy of VR interventions for the treatment of COVID-19-related psychological distress. Although the number of final literatures itself is not a deciding factor to conduct a systematic review and there is no minimum number of studies to include in a systematic review [58], this limited number of existing literatures may be interpretated as signifying that it is premature to perform a systematic review. Even when there is no study finally included, a systematic review can be meaningful to provide experts’ perspectives on a focused topic [18]. Also, the number of initially screened articles was 239 after excluding unrelated PICOTs, which indicates that there is burgeoning interest and evidence of possible role of VR-based psychological interventions for COVID-19-related mental problems. Thus, we thought that a systematic review of this topic is necessary now to provide an overall picture of the published research to date and make suggestions to improve the quality of future research.
Despite the limited number and low methodological quality of existing studies, our results suggest that VR intervention has promising potential to ameliorate COVID-19-related psychological distress with efficacy and safety. In a world where the demands for mental health service are steeply increasing in response to unforeseen social and natural disasters including the pandemic, well-designed, evidence-based VR interventions can function as useful supplement or alternatives of traditional face-to-face psychotherapy. And our review suggests the major points that needs to be addressed to turn the potential of VR intervention into real progress in the near future.
Supplementary Materials
The online-only Data Supplement is available with this article at https://doi.org/10.30773/pi.2022.0337.
Search Strategy for Mapping Review
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
Ji Sun Kim, a contributing editor of the Psychiatry Investigation, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Author Contributions
Conceptualization: Bin-Na Kim, Ji Sun Kim. Formal analysis: Seul-Ah Lee, Simyang Heo. Investigation: Somin Kim, Chaeyeon Park, Yujin Jung, Garam Ji, Hyeon-Ah Lee, Kibum Kim, Sungkean Kim. Writing—original draft: Seul-Ah Lee, Simyang Heo. Writing—review & editing: Bin-Na Kim, Ji Sun Kim.
Funding Statement
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI22C0619).
Acknowledgements
This study was also supported by Soonchunhyang University.