Level of Psychological and Somatic Symptoms Predict Perimenopausal Syndrome Severity Better Than Obstetric and Psychiatric History Do Among Korean Women
Article information
Abstract
Objective
Menopause symptoms can vary in type, duration, and severity. The purpose of this study was to investigate the key factors predicting severe symptoms among Korean perimenopausal women with various demographic data, obstetric and psychiatric histories, and menopausal symptoms screening scale scores.
Methods
Data were collected from 1,060 women, and 4 latent classes were identified using latent profile analysis, with 6 major categories of menopausal complaints. Among the 4 classes, we selectively used data from the “all unimpaired” and “all impaired” groups. Menopause rating scale (MRS), sociodemographic, obstetric, and psychiatric factors were assessed, and hierarchical logistic regression analyses were conducted with the “all impaired” group as a dependent variable.
Results
Marital status and scores on the psychological and somatic subscales of the MRS were statistically related to being in the “all impaired” group. Otherwise, family history of menopausal symptoms, menarche age, and history of other psychiatric disorders were not statistically significant predictors of being in the “all impaired” group.
Conclusion
The psychological and somatic subscales of the MRS predict the severity of perimenopausal syndrome better than obstetric and psychiatric history do among Korean perimenopausal women. Psychological and somatic symptoms as well as genitourinary symptoms in menopausal patients should be closely evaluated.
INTRODUCTION
The transition to menopause, perimenopause, is a natural event in every woman’s life, led by a progressive decrease in reproductive hormones. By definition, perimenopause is the transitional time around menopause (permanent termination of menstruation) when menstrual periods become irregular before they finally stop. It mostly occurs between 40 and 60 years of age and can last for 2–10 years [1-5]. During perimenopause, many women experience physiological and psychological changes, including vasomotor (hot flashes, night sweats), somatic (headaches, joint and muscle aches), cognitive (trouble concentrating, forgetfulness), urogenital (vaginal dryness, frequent voiding, changes in sexual desire), and psychological (insomnia, mood changes, anxiety, irritability) changes [5-7]. Although most symptoms are not fatal, they might affect all aspects of quality of life and have a negative impact on the physical and mental health of perimenopausal women [8,9].
Perimenopausal symptoms vary in terms of duration, prevalence, and severity. A previous study conducted in the United States found that vasomotor symptoms, one of the primary menopausal complaints for which women seek therapeutic management [10,11], last for an average of 10 years [12], with an extended duration in women whose symptoms started earlier [13]. In addition, approximately 75% of women experience varying degrees of menopausal symptoms ranging from mild to very distressing [14]. In general, roughly half of symptomatic women report only mild severity while the other half complain of moderate-to-severe symptoms [15,16].
Previous studies have discovered various risk factors affecting perimenopause symptoms, including ethnicity, socioeconomic features, medical and psychiatric histories, age, obesity, and lifestyles [13,17-19]. Previous multivariable logistic regression analysis revealed that older age, unemployment, irregular menstruation, and constipation were risk factors while a high monthly family income was a protective factor for perimenopausal syndrome [20]. Other studies have also shown that older age, low education level, and history of previous premenstrual syndrome are associated with a high risk of perimenopausal symptoms [21-23].
As a screening tool for menopausal women’s overall health, the menopause rating scale (MRS) consists of 3 domains of symptoms identified from factorial analysis and statistical methods: psychological, somatic, and urogenital [24,25]. MRS has been used as an efficient screening tool internationally for over 20 years with good validity [26] and was also proven to be useful as a single tool to evaluate the severity of age- or menopause-related complaints among middle-aged women [27].
Considering the high prevalence, heterogeneity, and negative impact of perimenopause symptoms on women’s overall health, there is a growing demand for new evidence regarding the perimenopause period. In this study, we aimed to find the major factors predicting the high-risk group for the severe perimenopausal symptoms among various factors such as sociodemographic, obstetric, and psychiatric factors, and scores on MRS. In addition, we hypothesized that the MRS scale would be the most important predictor among these.
METHODS
Study participants
This research was part of a cross-sectional study of Korean women aged 40 to 60 years concerning psychosomatic symptoms among Korean perimenopausal women conducted at the Chung-Ang University Hospital, Seoul, Korea. We collected data from 1,060 perimenopausal women through a research company (Macromill Embrain Co., Ltd., Seoul, Korea). To include only perimenopausal women among 40 to 60 years in this study, we recruited those whose last menstrual period was within one year and those whose menstrual cycle had recently become irregular compared to past. Participants’ perimenopausal symptoms were evaluated, including overall menopausal symptoms, depression, somatic symptoms, insomnia, memory, sexual dysfunction, and overactive bladder symptoms. Based on this data, we conducted a latent profile analysis as a statistical method, which assumes that the observations are made up of a blend of dissimilar distributions and aims to identify subgroups based on the characteristics of individuals’ response patterns and reveal similarities in individuals within groups [28,29]. Using scores of six scales on mood, somatic symptoms, sleep, memory, sexual symptoms, and urinary symptoms, multidimensional psychosomatic symptom profiles were classified according to differences in the level of symptoms and the degree of co-occurrence of symptoms. As a result, 4 latent classes were identified: 1) all unimpaired (class 1, n=530); 2) impaired sexual function, while others are unimpaired (class 2, n=186); 3) unimpaired sexual function, while others are impaired (class 3, n=216); and 4) all impaired (class 4, n=128). That means, class 1 showed low-level symptoms on all six scales, with class 4 showed high-level symptoms on all scales. The statistical analysis method and statistical indices of the latent profile analysis that led to the deduction of the 4 groups were discussed in our previous report [30].
In the current study, we selectively used data from the “all unimpaired” group reporting few menopausal symptoms and the “all impaired” group reporting severe menopausal symptoms among the study population. We then investigated the factors predicting the likelihood of being in the “all impaired” group among various factors such as sociodemographic, obstetric, and psychiatric factors, and subscale scores of MRS.
The study protocol was approved by the Chung-Ang University Hospital Institutional Review Board (reference number: 2160-001-464) and written informed consent was provided by all participants.
Measures
MRS
The MRS was used to measure health-related quality of life in middle-aged women [24,31]. The MRS consists of 11 questions measured on a 5-point Likert scale, ranging from 0 to 4 points. The scale comprises 3 domains: psychological, somatic, and urogenital. Previously, MRS demonstrated a high level of internal consistency (Cronbach’s alpha=0.87) [26].
Sociodemographic factors
Sociodemographic factors collected for this study were age, marital status, educational level, job status, and average monthly family income.
Obstetric factors
Obstetric history collected for this study included premenopausal menstrual cycle regularity, complete menopause status, family history of menopause symptoms, the period from the onset of menopause, menarche age, number of pregnancies, and number of deliveries.
Psychiatric factors
The psychiatric factors investigated for this study included a history of premenstrual syndrome, postpartum depression, postpartum psychosis, and other psychiatric disorders.
Statistical analysis
The distribution of sociodemographic, obstetric, and psychiatric characteristics across the study population was calculated. For univariate analyses, we used independent t-test and chi-square tests to compare variables between participants in the “all unimpaired” group and “all impaired” group.
To determine the influence of MRS subscales on the severity of perimenopausal symptoms, hierarchical logistic regression analyses were performed. In Model 1, the association between sociodemographic factors and perimenopausal symptoms was tested. Obstetric factors were added to Model 2 to test the associations of obstetric history with sociodemographic factors. Psychiatric factors were added to Model 3 to test the association of psychiatric history beyond the effects of sociodemographic factors and obstetric history. Finally, MRS subscale scores were added to Model 4 to test the association of MRS subscale scores with sociodemographic, obstetric, and psychiatric factors. Statistical significance was set at p=0.05 (two-sided). We used the Complex Samples module of the SPSS Statistics software package, version 19 (IBM Corp., Armonk, NY, USA), to conduct all analyses.
RESULTS
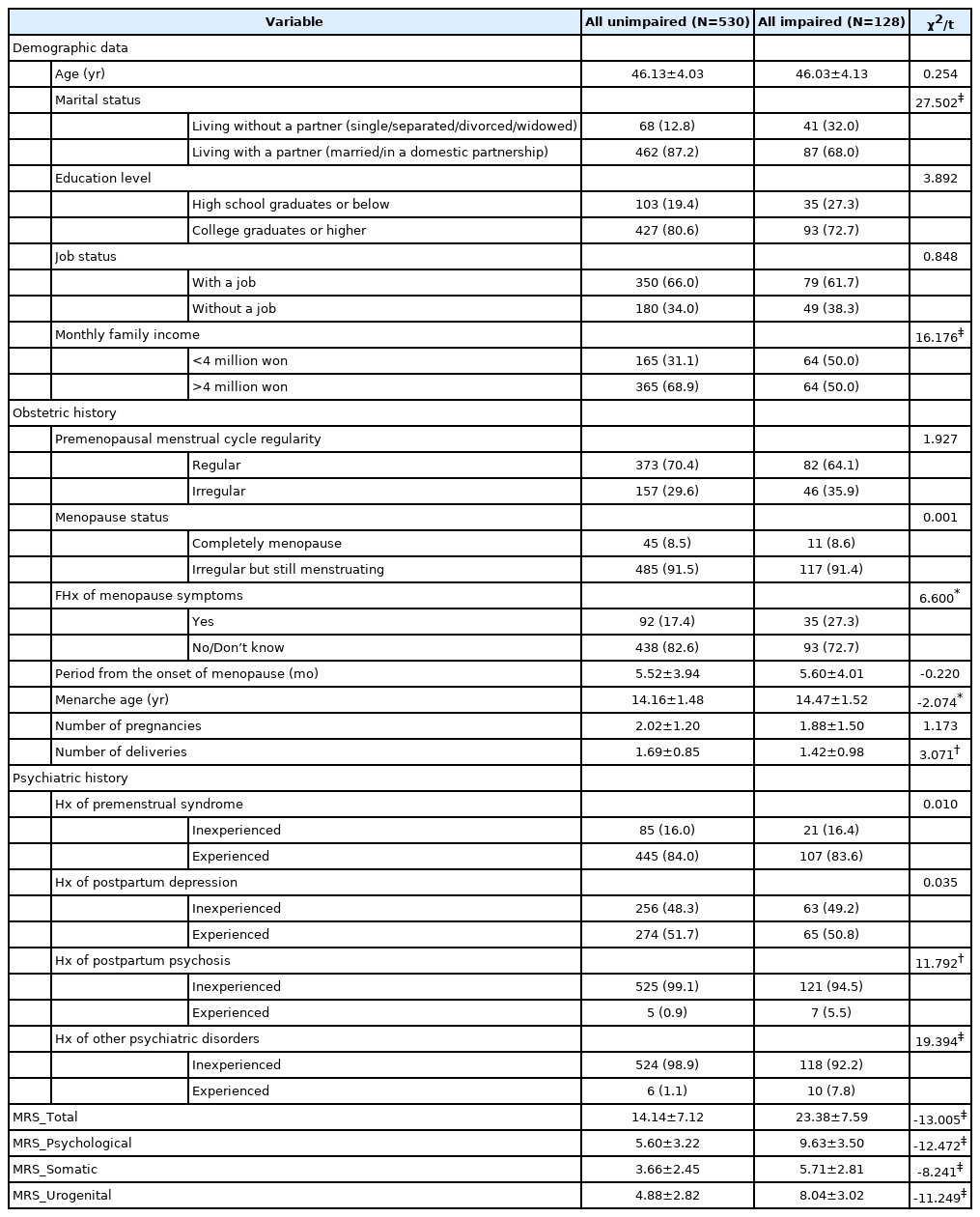
The comparison of demographic data, obstetric history, and psychiatric history between the “all unimpaired” group and the “all impaired” group
The distribution of sociodemographic, obstetric, and psychiatric characteristics across the study population is presented in Table 1, and a comparison of these characteristics between the “all unimpaired” group and the “all impaired” group is presented in Table 2. The participants in the “all impaired” group are more likely to live without a partner and have less monthly family income than those in the “all unimpaired” group. In addition, participants in the “all impaired” group are more likely to report a family history of menopause symptoms, older menarche age, and small number of deliveries compared to those in the “all unimpaired” group. Regarding psychiatric history, the participants in the “all impaired” group are more likely to have a history of postpartum psychosis or other psychiatric disorders compared to those in the “all unimpaired” group. The total MRS scores and all 3 subscale scores (psychological, somatic, and urogenital) were higher in the “all impaired” group than in the “all unimpaired” group.
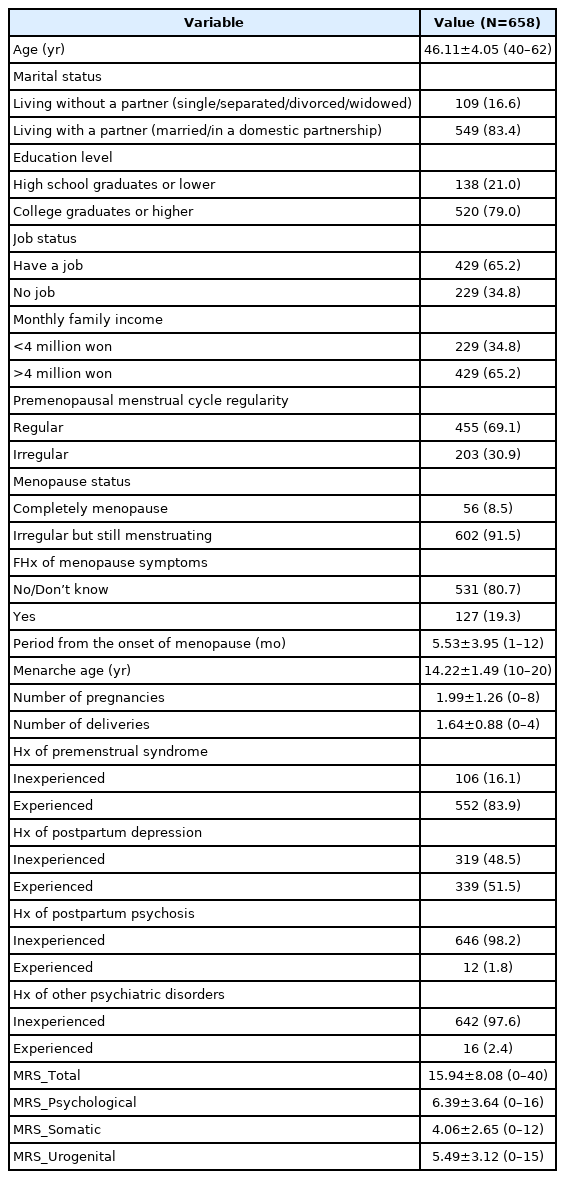
The distribution of sociodemographic, obstetric, and psychiatric characteristics of the study population
Results of hierarchical logistic regression analyses of MRS subscale scores with the “all impaired” group as a dependent variable
Table 3 summarizes the results of the hierarchical logistic regression analyses, which tested the association between being in the “all impaired” group and the sociodemographic, obstetrical, and psychiatric factors, and the MRS subscale scores among postmenopausal women. All 4 models of hierarchical logistic regression showed a significant overall model fit. In Analysis Model 4, both model χ2 (186.988, p<0.001) and the Nagelkerke R2 value (0.395, explaining about 39.5% of the variance in the dependent variable) reflected that the analysis model was adequate to account for being in the “all impaired” group. Looking at the practical effectiveness of the model according to classification accuracy, 19 variables in Analysis Model 4 noticeably improved its explanation accuracy to 85.9% for the group membership of the dependent variable. Wald statistics were used to define whether each indicator had a significant individual relationship with being in the “all impaired” group. Among the independent variables, marital status and scores on the psychological and somatic subscales of the MRS were statistically related to being in the “all impaired” group in Analysis Model 4. The marital status and menarche age score were statistically related to being in the “all impaired” group in Analysis Models 2 and 3. In addition, a history of other psychiatric disorders was statistically related to being in the “all impaired” group in Analysis Model 2. However, marital status, age at menarche, and history of other psychiatric disorders were statistically non-significant in Model 4.
DISCUSSION
This study aimed to determine the association between several sociodemographic, obstetric, and psychiatric predictors and perimenopausal symptom severity during perimenopause. The results of logistic regression analyses revealed that marital status and scores on the psychological and somatic subscales of MRS were statistically related to being in the “all impaired” group. Otherwise, family history of menopausal symptoms, obstetric history, and history of other psychiatric disorders were not statistically significant predictors for being in the “all impaired” group.
Between the two groups, the menarche age of the participants in the “all impaired” group was higher than that of the participants in the “all unimpaired” group. In addition, later menarche age as a dependent variable was identified as a significant risk factor before MRS was added to Model 4 in the regression analysis. The age at menarche has been implicated to be associated with disease risk in women in late life [32-34]. Specifically, early age at menarche is associated with risks of hypertension [35], cardiovascular disease [36], endometriosis [37,38], and metabolic disorders [39]. On the other hand, later age at menarche is associated with risks of depression [40] and lower bone mineral density [41]. In relation to depression, it has been suggested that the duration of the reproductive period, rather than the age at menarche itself, is negatively associated with depression prevalence. A meta-analysis of 14 studies revealed that late menopause age and long duration of reproductive years were associated with a decreased depression risk in post-menopause life [42-44]. A longer reproductive period represents longer exposure to endogenous female hormones, including estrogen and progesterone. Estradiol, the main estrogen, moderates the various pathways implicated in the etiologies of depression, anxiety, and various stress reactions, including the regulation of serotonin neurochemistry [45], activation of the hypothalamic pituitary adrenal axis and immune system, and neuroplasticity [46]. Considering the role of estrogen, we might infer that short exposure to estrogen due to late menarche might have contributed to the occurrence of various menopausal symptoms and depression.
Hierarchical logistic regression analysis revealed that living without a partner and high scores on the psychological and somatic subscales of MRS significantly influenced the severity of perimenopausal impairment. Our findings on the relationship between marital status and perimenopausal impairment are consistent with those of previous studies showing that married women’s overall perimenopausal health status is better than that of single/divorced/widowed women, probably because of their more positive views about menopause [47-49]. One study revealed that sexually active women reported low total MRS scores and low somatic, psychological, and urogenital subscale scores [50]. In studies conducted on Koreans, it has been repeatedly reported that disease status (hypertriglyceridemia, metabolic syndrome, and depression) and health behaviors (smoking, binge drinking, and inadequate sleep) were significantly poor in middle-aged populations not living with partners [51-53], and our findings are consistent in this context. Meanwhile, there have been contradictory findings that married women complained more of vasomotor, genitourinary, or sexual symptoms than single/separated/widowed women [17,54-56]. In particular, more sexual problems in women living with partners have been associated with comparatively active sexual lives [55]. Therefore, additional studies are needed to determine the relationship between marital status and the severity of menopausal symptoms.
Results on the association between MRS subscale scores and perimenopausal symptoms severity are more notable. From the results of the hierarchical logistic regression analyses, only psychological and somatic subscales of MRS were significant predictors of being in the “all impaired” group among various obstetric and psychiatric factors. Family history of menopause symptoms, menarche age, and history of other psychiatric disorders were found to be risk factors only before MRS was added to Model 4. This means that the 2 MRS subscales account for much more weight in evaluating the general health of middle-aged women related to perimenopause symptoms, regardless of obstetric or psychiatric history. Moreover, it is worth noting that the current MRS psychological and somatic subscale scores were more important predictive factors than psychiatric history, including premenstrual syndrome, postpartum depression/psychosis, and other psychiatric disorders, which were previously emphasized as important risk factors for perimenopausal symptoms [21,23].
Taking a closer look at the characteristics of the MRS scale, the 3 dimensions and 11 questions of MRS are described as follows: 1) psychological: depressive mood, irritability, anxiety, and physical and mental exhaustion; 2) somatic: hot flashes/sweats, heart discomfort, insomnia, and muscle and joint discomfort; and 3) urogenital: sexual problems, bladder problems, and vaginal dryness. Conventionally, interest in menopausal symptom treatment has been limited to gynecological hormonal and non-hormonal treatments targeting urogenital symptoms such as urinary incontinence and vaginal dryness and vasomotor symptoms such as hot flashes and night sweats [11,57,58]. In a study conducted in the USA, only 2% of participants reported having visited a psychiatrist for perimenopausal symptom treatment, while 63% reported visiting gynecologists [11]. Regarding therapeutic targets as reported by the study participants, vasomotor and genitourinary symptoms including hot flashes (21.9%), osteoporosis (7.3%), menstrual cycle regulation (3.6%), and vaginal dryness or irritation (4.4%) were reported frequently, whereas psychological symptoms including anxiety (1.2%) and depression (0.9%) were reported relatively infrequently [11]. Interestingly, however, in the same study, the main symptoms that healthcare professionals discussed with patients were psychological and somatic symptoms such as difficulty sleeping, exhaustion, depression or anxiety, muscle- and joint-ache, and lack of energy as well as vasomotor symptoms such as hot flashes and night sweats [11]. In line with our findings, this also suggests that psychological and somatic symptoms that can be treated by psychiatrists are the main impairing symptoms in perimenopausal women, although they are often overlooked as therapeutic targets and it is difficult to sufficiently improve the somatic and psychological symptoms with conventional perimenopause treatment such as hormone therapy [59].
This study has some limitations that should be considered when interpreting the results. First, the cross-sectional design enabled the identification of associations, but not necessarily causal relationships. Second, because we collected data using a self-reported online survey, a reporting bias should be considered. It has been shown that women often fail to provide reliable reports, particularly regarding the history of menstrual cycle-related mood disorders and peripartum psychiatric disorders such as premenstrual syndrome (PMS), peripartum depression, or peripartum psychosis [60]. This might be due to the characteristics of retrospective descriptions and the tendency of a long time elapsed since labor. Therefore, it is important to remember that information about PMS and peripartum psychiatric history could be over- or under-reported. Third, laboratory data on biological hormone levels, including estrogen and follicle-stimulating hormone, were not available in this study. If sex hormone levels could be measured, it would have been possible to accurately determine participants’ menopausal stage and understand the precise biological role of hormonal factors on perimenopausal symptoms. Fourth, the two latent class groups included in this study may not sufficiently represent the characteristics of the entire population. Therefore, further longitudinal studies using a more diverse and representative population would be helpful to confirm the validity and generalizability of the current results.
In summary this study aimed to identify the determinant factors of menopausal symptom severity among perimenopausal Korean women using multivariate regression analysis. Consequently, psychological symptoms including depressive mood, irritability, anxiety, and physical/mental exhaustion and somatic symptoms including hot flashes/sweats, heart discomfort, insomnia, and muscle/joint discomfort assessed with the MRS scale predicted the severity of perimenopausal syndrome better than a family history of menopausal symptoms and the obstetric or psychiatric history of perimenopausal Korean women did. In conclusion, MRS (more precisely, the psychological and somatic subscales of MRS) is an excellent screening tool, which is important to offset the effects of other risk factors in regression analysis. In addition, more careful evaluation and treatment should be performed on individuals reporting high scores on the psychological and somatic subscales of the MRS. Thus, psychological and somatic symptoms, as well as genitourinary symptoms in menopausal patients, should always be closely evaluated. Further research on various treatment methods that focus on the treatment of psychological and somatic symptoms is needed.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Ji Sun Hong, Jeong Seok Seo. Data curation: Da Seul Kim, Seunga Han. Formal analysis: Da Seul Kim, Sun Mi Kim. Investigation: Soyeon Kim, Seunga Han. Writing—original draft: Soyeon Kim, Ji Sun Hong. Writing—review and editing: Sun Mi Kim, Jeong Seok Seo.
Funding Statement
This study was supported by the Chung-Ang University Research Grants in 2021 and the National Research Foundation of Korea (NRF) grant funded by the Korea government (Ministry of Science and ICT Information and Communication Technology; MSIT) (No. NRF- 2021R1G1A1008625).