The Change of Suicidal Ideation Over a 12-Week Naturalistic Treatment of Depression: Comparison Between Young People and Older Adults
Article information
Abstract
Objective
We investigated the differences in suicidality between young people and older adults with depression over the course of 12-week naturalistic treatment with antidepressants.
Methods
A total of 565 patients who had moderate to severe depression (Hamilton Depression Rating Scale [HAM-D] score ≥14) and significant suicidal ideation (Beck Scale for Suicide Ideation [SSI-B] score ≥6) were recruited from 18 hospitals. Participants were classified into two groups: the younger group (13–24 years of age, n=82) and the older group (≥25 years of age, n=483). Total scores over time on the SSI-B, HAM-D, and Hamilton Anxiety Rating Scale (HAM-A) were assessed and compared between the two groups.
Results
At baseline, the younger group had lower HAM-D scores (21.0 vs. 22.2; p=0.028) but higher SSI-B scores (19.4 vs. 15.6; p<0.001) compared with the older group. The overall 12-week proportion of patients with resolved suicidality was 44.1% in the younger group and 69.2% in the older group. Although the improvement in the HAM-D and HAM-A scores did not differ between the groups, suicidal ideation in the younger group remained more severe than in the older group throughout the treatment. The ratio of the subjects who achieved HAM-D remission or response but did not achieve SSI-B remission was significantly higher in the younger group than in the older group.
Conclusion
These data suggest that in depressed youths, suicide risk is a serious concern throughout the course of depression even when favorable treatment outcomes are obtained.
INTRODUCTION
Suicidal behavior in young people has been recognized as a serious public health concern worldwide. Suicide is the second leading cause of death among adolescents and young adults in the United States and worldwide [1,2]. In 2019, 8.9% of high school students attempted suicide one or more times and 18.8% seriously considered suicide within the past year in the United States [3]. Although the prevalence of actual suicide deaths among adolescents is low (10.5 per 100,000) [4], approximately 40% of teenagers will make a subsequent attempt within 2 years of their initial suicide attempt [5]. The risk of later suicide completion in subjects who have previously attempted suicide is increased by 10–60 fold [6,7].
Depression is one of the most prominent predictive factors of suicidal behavior among both adults and young people [8,9]. The findings of psychological autopsy studies showed a high prevalence of mental illness in adolescent suicide victims with affective disorders the most common [5,10]. The National Comorbidity Survey Replication Adolescent Supplement (NCS-A) reported that 75% of adolescent suicide attempters and 56% of adolescents with suicide ideation met lifetime criteria for major depression or dysthymia [11,12]. Major depressive disorder is a stronger predictor of suicide compared to other psychiatric disorders characterized by anxiety, agitation, and poor behavioral control [9,13]. A meta-analysis found that 26.3% of suicides in males and 31.6% in females are attributable to a mood disorder [14].
However, multifactorial origins of suicidal behavior are more emphasized in young people [15]. Although treatment of depression has constituted the most reliable preventive strategy for suicide, a meta-analysis of pediatric antidepressant trials paradoxically indicated that antidepressant treatment might be implicated as a possible precipitating factor for suicide in the young people under 25 years of age [16,17]. It has been proposed that antidepressants may induce behavioral activation such as irritability or akathisia, which would facilitate suicidal ideation and behavior combined with their traits of high impulsivity and agitation [18]. However, uncertainty over this issue remains. Even in the psychosocial treatment of adolescent depression, emergent suicidality is also a common occurrence. Bridge et al. [19] found that the incidence rate of emergent suicidality over 12 to 16 weeks of psychotherapy was similar to those reported in antidepressant trials. Recent research has emphasized that the suicidal risk secondary to untreated depression is greater than that of a side effect of antidepressant treatment [20]. However, few studies have directly focused on whether young people with suicidal ideation have a distinctive course of suicidality during treatment compared to adults. Just as the clinical nature of depression in young people varies with diverse symptoms that are incongruous with traditional diagnostic criteria for depression [21], the features of suicidality associated with depression and treatment of that may also differ between the two groups. It could be important to decide the appropriate duration of close monitoring for the young people under the depression treatment.
The present study is based on a secondary analysis of cohort data from the Clinical Research Center for Depression (CRESCEND) study, which is a naturalistic, prospective, multi-center, clinical study of depressive disorders. In this study, we investigated the differences in suicidality between young people and older adults with depression during the course of antidepressant treatment. Previously, we found several differences of suicide-related characteristics between young people and older adults with depression using crosssectional data of 1,004 subjects of the CRESCEND study [22]. In the current study, the patients (n=565) who had significant suicidal ideation at the beginning of treatment were selected, and their changes of severity in suicidal ideation, depression, and anxiety were observed during the 12-week treatment. We expected to find differences in the course of suicidal ideation and its relationships with depression and anxiety severities between the two groups.
METHODS
Study overview
The CRESCEND study is an observational cohort study of the clinical outcomes of participants with depressive disorders. It includes two phases over 9 years of follow-up. In phase I, eligible participants began the study with a baseline visit to the hospital and were assessed at 1, 2, 4, 8, 12, 24, and 52 weeks. Phase II involved an extension study in which participants were evaluated annually over the course of years 1–9. Eighteen hospitals (16 universities and two general hospitals) have collaborated in the ongoing CRESCEND study. At least two hospitals were recruited from each province and contributed to patient recruitment and follow-up. The central coordinating center is located in the Psychiatric Department of the Catholic University Medical Center in Seoul and provides educational support and coordination for enrollment and follow-up of study participants. The data-management center is in the Preventative Medicine Department of the Catholic University College of Medicine and provides support for obtaining data and quality control.
Because the CRESCEND study was designed to fit into actual clinical settings as much as possible, broad inclusion criteria and minimal treatment restrictions were employed. Enrollment occurred in a naturalistic clinical environment of both outpatient and inpatient settings regardless of depression subtype. Treatment interventions were also conducted in a naturalistic fashion, and each clinician was granted total discretion to determine the type, dose, and regimen of antidepressant and other medications.
Data on sociodemographic, clinical, and treatment-related characteristics were obtained by clinical research coordinators, who were trained and certified in clinical report form (CRF) implementation and data collection methods by the central coordinating center and supervised by the clinicians of the regional centers. Psychologists and resident psychiatrists served as the raters at each site. Meetings for training and certification of raters were held twice per year. Participant data were recorded on a predetermined CRF at each visit, recorded on the website homepage of the CRESCEND study within 2 days, and monitored by personnel at the data-management center. A detailed description of the CRESCEND study sample and design is available elsewhere [23,24].
Participants
All patients with a depressive disorder who were reviewed at the study hospitals were approached regarding participation in this study. The clinicians assessing and diagnosing patients applied the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria [25]. The DSM-IV-based Structured Clinical Interview was administered at week 2 to the subsample who agreed to participate for purposes of confirmation [26]. All patients included in this study were beginning new treatment episodes, whether depressive symptoms were first onset or recurrent. No advertisement to recruit participants was issued, and no financial compensation for study participation was provided. The time frame for baseline recruitment was from January 2006 to August 2008.
Inclusion criteria were 1) outpatients and inpatients aged >7 years and 2) a DSM-IV diagnosis of a depressive disorder (major depressive disorder with or without psychotic features, dysthymic disorder, depressive disorder not otherwise specified). Exclusion criteria were 1) a current or lifetime comorbid DSM-IV diagnosis of schizophrenia, other psychotic disorder, bipolar disorder, organic psychosis, or dementia; 2) a medical or neurological illness of sufficient severity to interfere with the evaluations and interviews for the study; and 3) pregnant or breastfeeding women. Although not used to determine inclusion in the CRESCEND study, 1) baseline Hamilton Depression Rating Scale (HAM-D) score ≥14 (above moderate severity of depression), 2) baseline Beck Scale for Suicide Ideation (SSI-B) score ≥6 (significant suicidal ideation), and 3) ≥13 years of age were additional criteria for our study objectives.
This study was approved by all relevant university and/or hospital institutional review boards. All participants reviewed the consent form and written informed consent was obtained by research staff before participation in the study. Written consent was obtained from the parent or legal guardian and from the participant for those aged <16 years. The nature and purpose of the study were explained to those who were very old or physically ill, and written informed consent was obtained from the person or their caregiver, as appropriate.
Evaluations and measurements
The CRESCEND research protocol recommended assessments at baseline, 1, 2, 4, 8, 12, 24, and 52 weeks and every year thereafter. The analysis described here was restricted to data obtained up to 12 weeks after admission to focus on acute treatment.
Baseline assessments included diagnostic evaluations and retrospective reports of histories of medical and/or psychiatric illnesses and treatments. Data on sociodemographic characteristics including age, sex, formal education, marital status, cohabitation status, religious affiliation, current occupation, and monthly income were also gathered. Historical information was collected with the structured CRF to obtain detailed data on previous suicide attempts and current suicidal ideation.
The SSI-B is a structured self-administered scale designed to measure three dimensions of suicidal ideation: active suicide desire, specific plans for suicide, and passive suicide desire [27]. The SSI-B contains 21 items on a 3-point Likert scale ranging from 0 to 2, and the severity of suicidal ideation is calculated by summing the ratings for the first 19 items. Higher scores reflect higher suicidal ideation and risk. A score ≥6 has been used as a cutoff threshold for clinically significant suicidal ideation and the resolution of suicidality was defined as suicidality improved to an SSI-B score <6 [28,29].
Other instruments included in this analysis were the HAM-D [30], the Hamilton Anxiety Rating Scale (HAM-A) [31], the Clinical Global Impression Scale–Severity (CGI-S) [32], and the Social and Occupational Functioning Assessment Scale (SOFAS) [33]. Adverse events during the study period were recorded using the UKU side-effect rating scale [34].
Statistical analysis
As in the meta-analysis of Stone et al. [17], participants were divided into two groups; the younger group (<25 years of age) and the older group (≥25 years of age). As described above, an SSI-B score of 6 was determined as a cutoff score for clinically significant suicidal ideation. SSI-B remission was defined as suicidality improved to an SSI-B score <6 and was maintained until the 12-week study endpoint or to the last follow-up examination if they withdrew from the study. HAM-D remission and response were defined as an HAM-D score ≤7 and a reduction of ≥50% compared with the baseline HAM-D scores, respectively and they maintained to the 12-week study endpoint or to the last follow-up examination if they withdrew earlier.
Summary statistics are presented as means and standard deviations for continuous variables and as numbers and percentages for discrete variables. The sociodemographic, clinical, and treatment characteristics of the younger and older groups were compared using a t-test, chi-square test, or Mann–Whitney U-test, as appropriate. Log-rank tests in Kaplan–Meier models were conducted to compare the cumulative proportions of participants with resolution of suicidality between the two groups. Repeated-measures analysis of variance (ANOVA) was performed to evaluate differences between the younger and the older groups according to changes in the SSI-B, HAM-D, and HAM-A scores using the Last Observation Carried Forward method. The proportion of subjects who achieved HAM-D remission or response but did not achieve SSI-B remission was compared between the two groups using the chi-square test. Statistical significance for all tests was set at p<0.05 (two-tailed). All statistical analyses were conducted using Statistical Analysis System version 9.1 (SAS Institute Inc., Cary, NC, USA).
RESULTS
Demographic and clinical characteristics
Of the initial 1,183 patients screened for the CRESCEND study, a total of 565 had HAM-D scores ≥14 and SSI-B scores ≥6 at baseline. Of the 565 patients, 82 (14.5%) were included in the younger group (age <25 years) and 483 (85.4%) in the older group (age ≥25 years) (Table 1). In the younger group, 20 patients (24.3%) were younger than 18 years (13–17 years). The older adult group included 70 elderly patients (age ≥65 years, 14.5%). Subjects in the younger group were more likely to be male, have a history of suicide attempt, a family history of depression, and a shorter duration of illness. Compared with the older group, the younger group had lower mean HAM-D scores (21.0 vs. 22.2; p=0.028), but higher mean SSI-B scores (19.4 vs. 15.6; p<0.001). The HAM-A, CGI-S, or SOFAS scores were not significantly different between the groups.
Treatment characteristics
The type of antidepressants prescribed to subjects differed significantly between the two groups (χ2=13.561, p=0.004) (Table 2). Compared with newer antidepressants, selective serotonin reuptake inhibitors were more frequently used by the younger patients than by the older patients (63.4% vs. 41.6%). Monotherapy was more frequent than switching or using a combination of antidepressants in both groups. Concomitant medications, particularly anxiolytics/hypnotics and antipsychotics, were also frequently used in both groups. However, no significant differences were observed regarding antidepressant regimens or concomitant medications between the two groups. The mean (standard deviation) number of visits, including the baseline visit, was 3.9 (1.9) in the younger group and 4.3 (1.9) in the older group. Of the 565 participants, 280 (49.6%) completed 12 weeks of assessments.
Cumulative probability of suicidal ideation resolution
Figure 1 displays the cumulative probability of suicidal ideation resolution according to the definition in the current study. The overall 12-week proportion of patients with resolved suicidality was 44.1% in the younger group and 69.2% in the older group. The younger group achieved SSI-B resolution later than the older group (log-rank statistics=6.978, p=0.008).
Changes in depression, anxiety, and suicidal ideation during treatment
The mean assessment scale scores of the patients over the 12 weeks of treatment are shown in Figure 2. The relationship between the time courses of SSI-B, HAM-D, and HAM-A was quite distinct between the two groups. Examination using a repeated measures ANOVA with baseline scale scores, sex, and type of antidepressants as covariates revealed no significant group differences for the changes in the HAM-D and HAM-A scores (p=0.470 and p=0.503, respectively). However, the changes in SSI-B scores differed significantly over time between the groups (p=0.020).
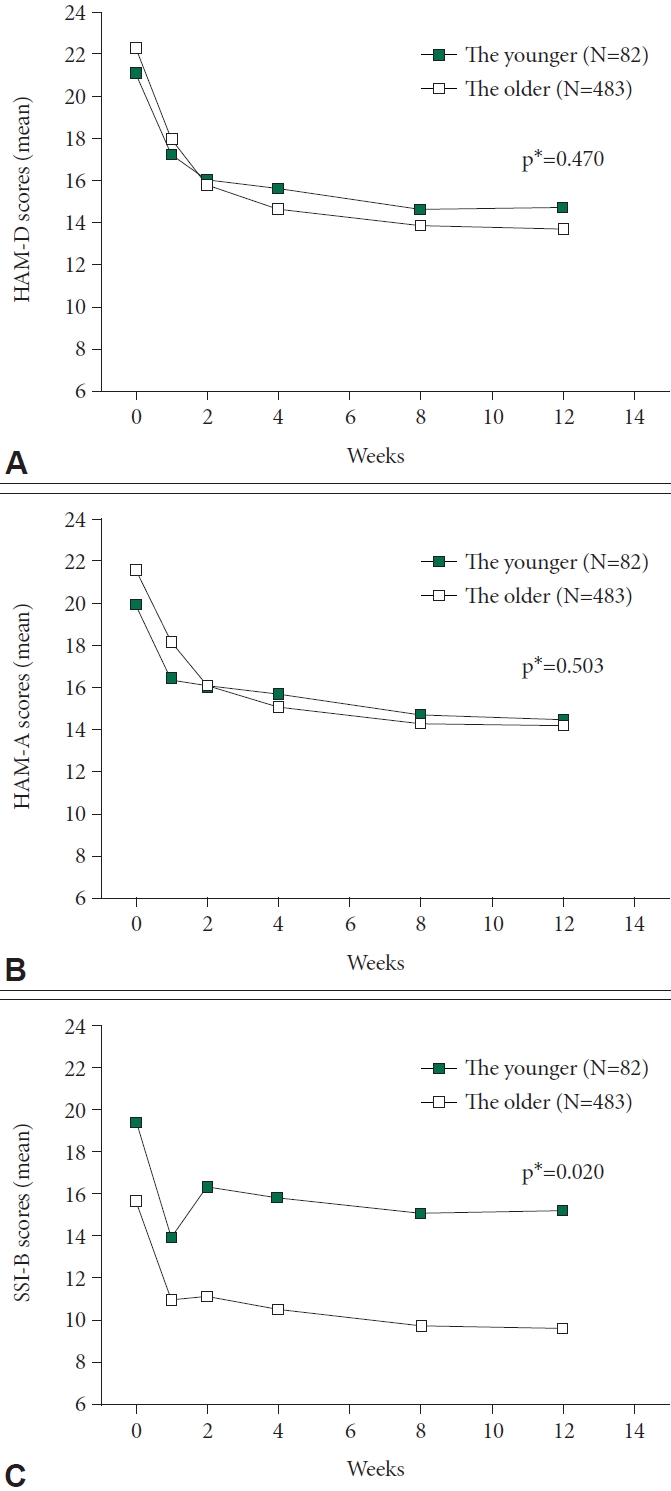
Changes in HAM-D (A), HAM-A (B), and SSI-B (C) total scores over time. *repeated-measures analysis of variance of overall changes between 2 groups; change from baseline is dependent variable, groups and visits are factors, and baseline scale scores, sex, type of antidepressants are covariates. HAM-D, Hamilton Depression Rating Scale; HAM-A, Hamilton Anxiety Rating Scale; SSI-B, Beck Scale for Suicide Ideation.
Association of suicidal ideation with treatment outcomes
Table 3 presents treatment outcomes and suicidal ideation over the 12 weeks of treatment. Significant differences were not observed in HAM-D remission and response rates between the two groups. However, the ratio of the subjects who achieved HAM-D remission but did not achieve SSI-B remission was significantly higher in the younger group than in the older group (50.0% vs. 21.6%, p=0.014). A similar trend was found in the ratio of subjects who achieved HAM-D response but did not achieve SSI-B remission (60.0% vs. 30.5%, p=0.003).
Incidence of suicide events
Suicide attempts were rare in both groups during the 12- week study period. Only three patients in the younger group (3.6%) and four in the older group (0.8%) attempted suicide during this interval. No participant completed suicide.
Incidence of akathisia
Of the 334 participants with UKU data, only 21 (6.3%) had akathisia scores ≥1 at some point during the 12-week treatment. Severe akathisia did not occur during the study period. A significant difference in the occurrence of akathisia was not observed between the younger and older groups (5.7% vs. 6.3%, p=0.873).
DISCUSSION
In this study, we examined differences in suicidality between young people and older adults with depression during antidepressant treatments in an environment similar to naturalistic clinical settings. We selected participants who had significant suicidal ideation at the entrance of the treatment and observed their course of suicidal ideation with the changes in depression and anxiety severity over the 12 weeks of treatment.
At baseline assessment, although both groups included only the subjects with SSI-B scores ≥6, the mean SSI-B score in the younger group was significantly higher than in the older group. This result is notable because the HAM-A scores between the two groups were not different, and HAM-D scores in the younger group were even lower than those in the older group. During the treatment, a clear difference was observed in the course of suicidality while similar courses of reduction in depression and anxiety symptoms were found in both groups. Following the substantial improvement of suicidal ideation at week 1, which may reflect a well-known placebo response to the unusual amount of time and attention given by clinicians or research staff [35], suicidal ideation relapsed more severely in the younger group than in the older group and remained over the rest of 12 weeks. Few studies have directly focused on the differences in suicidality between young people and older adults with depression. However, our findings are in agreement with a meta-analysis by Gibbons et al. [36], which included data from 41 randomized controlled trials of antidepressants. In the study, suicidal thoughts decreased over time with a reduction in depressive symptoms for adult and geriatric patients randomized to antidepressants compared with placebo. In young patients, however, statistically significant effects of treatment on suicidal thoughts or behavior were not found compared with placebo, despite a large overall reduction in depressive symptoms in the treatment group.
Our finding on the association between suicidal ideation and treatment outcome is also consistent with this result. The proportion of participants who achieved HAM-D remission or response but showed persistent suicidal ideation was higher in the younger group than in the older group. Contrary to the older group, more than half of the young patients who achieved HAM-D remission remained significantly suicidal. Relatively low remission and response rates in the current study compared with previous studies might reflect severe pathology of the study participants, resulted from selection criteria of having significant suicidal ideation [37]. Survival analysis also revealed that more time is needed for the young people to resolve their suicidal ideation compared to the older adults. Our findings suggest that the risk of suicide might be more severe in depressed young people than in older adults with similar depression severity and this persists throughout the course of acute treatment even with an overall improvement of depression.
These findings do not support the previous concept that the risk of suicide is a serious concern especially immediately after the start of treatment [38-40]. Reportedly, the vulnerability of young people to antidepressant-induced behavioral activation might facilitate suicidal ideation and behavior [18]. If that is the case, the risk of suicide would be highest at the beginning of antidepressant treatment [38]. However, we found that suicidal ideation in the younger group continued to be severe over 12 weeks except for the temporary improvement at week 2. The UKU data also showed that the difference in suicidality between the two groups did not result from drug-associated behavioral activation. In agreement with our findings, a study on the treatment for adolescents with depression (TADS) showed that the time to the suicidal event among depressed adolescents varied from 1 week to 6 months after the start of treatment [41]. Although the authors concluded that suicidal events occurred in a context of insufficient improvement, the overall depressive symptoms of adolescents with suicide events continued to decline after the start of treatment. Among participants with suicide events during treatments, only 6.6% of patients experienced worse depressive symptoms prior to suicidal events compared with the beginning of treatment, whereas 26.7% were assessed as improved or significantly improved prior to suicidal events.
In the current study, the reason why the improvement in depressive symptoms in young people did not ensure immediate resolution of risk of suicide as much as in older adults is unclear. However, significant emphasis has been placed on the role of maladaptive cognitive/emotional responses to stress and poor problem-solving skills in the suicidal behavior of adolescents because these are thought to exert an impact beyond depression [7,42,43]. These factors are associated with prolonged persistent negative emotional states that accompany stressful events and partially account for the relationship between negative life events and the risk of suicidal ideation [44,45]. A large proportion of child and adolescent suicide attempters have also exhibited impulsive and aggressive traits independent of depression [46,47]. Risk of suicide is strongly associated with the severity of depression in adults, whereas in young people suicidality appears more related to contextual factors such as family issues or peer conflicts [36,48]. In the TADS study, 72.7% of the patients with a suicidal event reported conflicts with parents or peers prior to suicidal events [41]. Although the current study could not prospectively evaluate environmental stressors, the majority of participants were treated in outpatient settings and would be under daily stress. Even when depression improves to mild or moderate, suicidality might occur more easily in young people. Recent epidemiological data revealed that most suicidal adolescents receive some form of treatment before the onset of suicidal behavior, but this fails to prevent such behaviors [11]. Our findings suggest that in depressed youths, the risk of suicide should be a serious concern throughout the course of depression and close attention should be paid even when favorable treatment outcomes are obtained.
In this context, it is also notable that the younger group exhibited more severe suicidal ideation even with lower HAM-D scores compared to the older group at baseline. While it might reflect clinical manifestations of depression among different age groups, it might also reflect the heterogeneity of the study population. Most of all, there is the likelihood of misdiagnosis of bipolar depression, particularly in the younger group. Approximately 60% of patients with bipolar disorder experience their first episode before the age of 18 years and the first episode is depression in 50%–60% of patients [49]. Bipolar disorder is also associated with severe suicidal risk and 70% of those suicides occur during depressive episodes [50]. Moreover, two-thirds of young people with depression also have other mental disorders, such as anxiety disorder, attention-deficit/hyperactivity disorder, oppositional defiant disorder, and substance use disorder [51]. They are in themselves risk factors for both adolescent depression and adolescent suicidality [51,52]. Suicidality of young people also gets impacted substantially by interpersonal stressors, such as conflicts with peers or romantic partners, bullying, and violence as well [53]. Primary diagnoses other than depression could be overlooked under the diagnosis of depression. This is an important issue to keep in mind to understand our findings.
This study had several notable strengths. First, as a naturalistic study, we could observe the change in suicidal ideation during the treatment, which was similar to actual clinical settings. Second, in this context, a relatively large number of subjects with baseline suicidality were included compared with controlled trials which have strict inclusion criteria. Third, separate measures for suicidality were used at each time point. Because suicidal ideation may range widely from fleeting thoughts of being better off dead to persistent, ruminative thoughts regarding suicide, dichotomous questions or a single ‘suicide’ item from a depression scale may not be valid to capture the potential ongoing suicidal processes [48]. Furthermore, youths appear more likely to report clinically relevant suicidal ideation when completing an assessment questionnaire themselves rather than to share these thoughts in a direct interview with a clinician [19,41].
This study also had several limitations. Besides the issue of heterogeneity described above, the current data do not necessarily represent epidemiological data because almost all participants were selected from university hospitals. Moreover, the enrollment was determined primarily by the clinicians at each site using convenience sampling. The current results could not be generalized to severe forms of suicide behaviors such as suicide attempts and completions. Although we examined suicide attempts prospectively observed during treatment, the sample size was too small to allow adequate exploration.
Despite these limitations, the present study provides valuable information regarding the relationships between depression and suicidality among young people. Our findings indicated that depressed youths who manifest suicidal ideation at the start of treatment are at more severe risk of suicide throughout treatment than older adults. Further longitudinal studies with long-term follow-up are necessary to confirm this finding.
Notes
Availability of Data and Material
Due to privacy and ethical concerns, neither the data nor the source of the data can be made available.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Tae-Youn Jun, Young Sup Woo, Hyeon Woo Yim, Jung-Bum Kim, Ho-Jun Seo. Data curation: Young-Eun Jung. Formal analysis: Hyeon Woo Yim, Jung-Bum Kim, Jae-Min Kim, Ho-Jun Seo. Project administration: Tae-Youn Jun. Supervision: Tae-Youn Jun. Writing—original draft: Young-Eun Jung. Writing—review & editing: Young Sup Woo, Hyeon Woo Yim, Ho-Jun Seo.
Funding Statement
This study was supported by a grant of the Korea Healthcare technology R&D Project, Ministry of Health and Welfare, Republic of Korea (HI10C2020). The Ministry of Health and Welfare had no further role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.




