One-year Cohort Follow-up on the Diagnosis and Posttraumatic Symptoms in Child Sexual Assault Victims in Korea
Article information
Abstract
Objective
The victims and their families of child sexual abuse (CSA) may confront persistent psychological sequela. We aimed to investigate the psychological symptoms, diagnosis, and family functions in children and adolescents with CSA.
Methods
We assessed the symptom scales at 6-month intervals, and conducted diagnostic re-assessments at 1-year intervals. Trauma Symptom Checklist for Children (TSCC), Trauma Symptom Checklist for Young Children (TSCYC), Family Adaptability and Cohesion Evaluation Scales IV (FACES-IV), and Family Communication Scale (FCS) scores were reported by children or parents.
Results
We found in parent-reported TSCYC, that posttraumatic stress symptoms domain scores significantly decreased with time progression. The scores decreased more in the evidence-based treatment group over time in anxiety and posttraumatic stress symptom domains of TSCC. In FACES-IV and FCS scores, indices of family function have been gradually increasing both after 6 months and after 1 year compared to the initial evaluation. Further, about 64% of the children diagnosed with psychiatric diseases, including posttraumatic stress disorder (PTSD) at the initial assessment maintained the same diagnosis at follow-up.
Conclusion
We observed changes in psychological symptoms and family functioning in sexually abused children with time progression during 1 year. It is postulated that PTSD may be a persistent major mental illness in the victims of CSA.
INTRODUCTION
Childhood sexual abuse (CSA) refers to unwanted sexual contact directed toward a child or an adolescent. According to the US Centers for Disease Control and Prevention (CDC), the definition is “any completed or attempted (noncompleted) sexual act, sexual contact with, or exploitation of child by a caregiver.” [1] The World Health Organization (WHO) defines CSA as “any sexual activity that they do not fully comprehend, for which they are unable to provide informed consent, or for which they are not developmentally prepared.” [2]
Traumatic experiences during childhood can have a wide range of adverse effects on children’s behavior, emotional, social, physical, and cognitive areas, because of their socio-psychological immaturity [3-5]. Studies have shown that children who are victims of childhood sexual violence receive mental health services at an approximately three times higher rate than children who are not victims of sexual violence until they reach adulthood [6,7].
Psychopathology has been reported after CSA as an immediate or short-term sequela, including fearfulness, anxiety-related symptoms, dissociation, and depression [8-10]. Further, victimized adolescents have been reported to exhibit increased multiple psychiatric problems [11], such as depression [12], anxiety [13], suicidal ideations or behavior [14-16], sexual dissatisfaction, uncontrolled sexual behaviors [17], aggression [18], and illegal drug or substance use [19,20], as well as an elevated risk of re-victimization [8,16,21,22]. Gomes-Schwartz et al. [23] conducted a study on the impacts of CSA by assessing the emotional distress in sexually abused children assessed after 2 years. They reported that 40% and 24% of children and adolescents, respectively, showed significant sequelae, including psychological, physical, and social development deficits. Moreover, there is a high likelihood of long-term psychological problems, including low selfesteem [24], maladaptive coping skills [24,25], as well as poor interpersonal skills26 and social support [27,28]. In addition, even in adulthood, the risk of multiple psychiatric diseases (especially depressive disorder [29,30] or anxiety disorder [30,31]) is increased [7,11,32-34]. And the victims may experience more life problems such as interpersonal relational problems, conflicts with spouses [34], and sexual dysfunctions [33-37].
As described above, the psychological changes that occur after CSA have the wide, long-term effects. Some studies report that improvements of these changes by treatments [38]; but there have been reports of treatment resistance regarding externalized problems and sexual concerns, also [39].
The harm caused by CSA is not limited to individual children, but also strongly affects other family members. There have been reports of parents experiencing serious disturbance and breakdown in family relationships [40]. In Anggraini’s qualitative study of six family groups affected by CSA, physical changes, such as changes of diet and sleep patterns, psychological changes, such as self-blame, being afraid, and increased emotional expression, and social changes were observed [41]. In a study by Stern et al. [24], various difficulties in family communication, family rules, effective involvement, and general functioning were observed among sexually abused children and their families. However, other studies have shown that there is no significant difference when examining changes in family function of victims by the Family Adaptability and Cohesion Evaluation Scales III scale [42,43]. Unfortunately, as there are few studies on family changes of victims, we attempted to observe changes in family functioning after CSA. Appropriate support from the primary support system after a CSA incident is important in the development and later recovery from psychiatric disease in victims [44-46]; therefore, there is a need to consider family functional changes to allow an understanding of the child’s progression. Proper exchange of dialogue between the primary support group, such as family, are important factors; thus, it is necessary to monitor the progress of changes in family communication. Particularly, since there are differences according to Eastern and Western cultures in the actual communication in the family and the dialogue between parents and children, we tried to determine the family changes after the incident in a Korean society [47].
Sexual assault is known to increase the risk of posttraumatic stress disorder (PTSD), and in a cross-sectional study conducted in the United States, 46% of adult sexual assault victims were diagnosed with PTSD [48]. The PTSD prevalence rate after CSA is 37%–53% [49]. Although some studies have shown that PTSD symptoms resolve within a few months [50,51], a study in Germany observed the course of PTSD in 2,548 adolescents and young adults, with only about 50% recovery [52]. In some cases, PTSD symptoms do not appear immediately after the trauma but may develop months or years after [22,39]. Since the development and persistence of PTSD have varying influences on victims, there is a need to consistently monitor their recovery.
In this article, we aim to verify the following hypotheses. First, the victims will continue to experience the trauma related psychological symptoms after CSA. Second, the victims’ families will experience functionally negative changes, after CSA. Third, the victims diagnosed with PTSD after CSA will have a difficult recovery. A prospective cohort study is a good method to reduce recall errors and confirm continuous changes. But there are few prospective cohort studies on this subject in Korea. Therefore, we performed a prospective follow-up study on a cohort of CSA victims.
METHODS
Participants
The Sunflower Center was established by the Ministry of Gender Equality and Family help CSA victims in South Korea and provide them with comprehensive care (e.g., clinical diagnosis, treatment, psycho-education, socio-legal supports). We enrolled children or adolescents receiving care at the Seoul Sunflower Center for children. Prior to registration in the study, we obtained informed consent and assent from children and caregivers willing to participate.
The inclusion criteria were as follows: 1) aged <19 years and 2) consent to participate in the study. The exclusion criteria were: 1) having severe brain injury or central nervous system dysfunction and 2) limited legal competence of both parents due to being assailants. We analyzed data from 28 participants who completed the first year of follow-up after registration in the cohort. This study was approved by the Institutional Review Board of Severance Hospital (IRB No. 4-2014-0876).
Evaluation
Assessments
We investigated sociodemographic and abuse-related data of the CSA victims and confirmed the psychopathology and Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) diagnoses of the CSA victims. Certified child and adolescent psychiatrists, as well as certified clinical psychologists, conducted individual interviews with the children and caregivers using the Korean Kiddie-Schedule for Affective Disorders and Schizophrenia-Present and Lifetime Version (K-SADS-PL) [53].
After the initial assessment, we performed follow-up assessments at 6-month intervals. Regarding the diagnostic process, each participant underwent the K-SADS-PL interview at 1-year intervals (Figure 1). Participants aged <6 years or with an intelligence quotient (IQ) <70 underwent clinical diagnosis based on the DSM-IV through a psychiatrist’s interview, clinical chart review, and diagnostic conference.

Flow chart of evaluations. K-SADS-PL, Korean Kiddie-Schedule for Affective Disorders and Schizophrenia-Present and Lifetime Version; TSCC, Trauma Symptom Checklist for Children; TSCYC, Trauma Symptom Checklist for Young Children; FACESIV, Family Adaptability and Cohesion Evaluation Scales IV; FCS, Family Communication Scale.
Intelligence
The Korean-Wechsler Preschool and Primary Scale of Intelligence-Fourth edition was used for participants aged 3–5 years, the Korean-Wechsler Intelligence Scale for Children-Fourth edition for participants aged 6–16 years, and the Korean-Wechsler Adult Intelligence Scale-Fourth edition for participants aged 17 years and above.
Instruments for trauma symptoms and family functions
Trauma Symptom Checklist for Young Children
This questionnaire was for children aged 3–13 years, parents report their child’s trauma-related symptoms observed for the last a month. It consists of two validity scales (atypical response and response level) and nine clinical scales (anxiety, depression, anger/aggression, post-traumatic stress-intrusion, post-traumatic stress-avoidance, post-traumatic stress-arousal, post-traumatic stress-total, sexual concerns, and dissociation). It has a total of 90 items with each scored on a 4-point Likert scale (1 [not at all] to 4 [very often]) [54]. Higher scores mean more trauma-related symptoms observed. The clinical cutoff score is 70. A T-score above 70 is interpreted as clinically significant [54]. A psychiatrist and a psychologist fluent in both Korean and English faithfully translated the original scale, and then another psychologist who was fluent in both languages used the reverse translation scale.
Trauma Symptom Checklist for Children
This is a self-report scale of posttraumatic symptomatology for participants aged 8–16 years. It consists of two validity scales (under-response and hyper-response) and six clinical scales (anxiety, depression, anger, posttraumatic stress, dissociation [with 2 subscales], and sexual concerns). The checklist consists of a total of 54 items with each scored on a 4-point scale (0 [never] to 3 [almost all the time]) [55]. Higher scores mean more trauma-related symptoms experienced. The clinical cutoff score is 65. A T-score above 65 is interpreted as clinically significant. The sexual concerns domain cutoff score is 70 [55]. A psychiatrist and a psychologist fluent in both Korean and English faithfully translated the original scale, and then another psychologist who was fluent in both languages used the reverse translation scale [56].
Family Adaptability and Cohesion Evaluation Scales IV
The Family Adaptability and Cohesion Evaluation Scales IV (FACES-IV) is an appraisal scale developed by Olson to evaluate family cohesion and flexibility [57,58]; in this study, we used the Korean version to evaluate parent-reported family functioning [59]. It comprises 42 items with each scored on a 5-point scale. Family functioning was assessed using six subscales divided into balance (cohesion and flexibility) and unbalance (disengaged, enmeshed, rigid, and chaotic). Each subscale score can be used to calculate the family cohesion, flexibility, and total circumplex ratios with a value greater than 1 indicating balanced family functioning and higher values indicating more balanced function [58].
Family Communication Scale
The Family Communication Scale (FCS) which measures the degree of positive communication between family members is a parent-reported scale as a 5-point Likert scale. We used the Korean version, which was adapted and validated by Kim et al. [60] Higher FCS scores indicate good quality and extent of family communications.
Treatment conditions
On the first visit to the Sunflower center, all participants and their caregivers were interviewed by a psychiatrist to check their psychological status and received a brief intervention to help stabilized after CSA. Afterward, treatment was provided by a psychiatrist or a psychologist in the center according to the initial condition of the victim and the consent of the caregiver. And in some cases, they were treated individually in institutions outside the center by their decision.
Because trauma-focused cognitive behavior therapy (TFCBT), eye movement desensitization and reprocessing (EMDR), supportive to psychodynamic psychotherapy and medications (selective serotonin reuptake inhibitors, antipsychotics adjuvant, serotonin and norepinephrine reuptake inhibitor, tricyclic antidepressants, mood stabilizers) are recommended for the treatment in the guideline for PTSD in Korea [61], the participants who have received at least one treatment among TF-CBT, supportive to psychodynamic psychotherapy, and EMDR, or pharmacotherapy with the drugs above for more than a week were defined as an evidence-based treatment (EBT) group. Participants who have no treatments or nonconventional treatment for PTSD such as art and music therapy was performed were considered as a no evidencebased treatment (non-EBT) group.
Data analysis
We examined the following sociodemographic data of the participants: sex, age at study enrolled, age at the time of the first CSA incident and IQ. We compared the Trauma Symptom Checklist for Young Children (TSCYC), Trauma Symptom Checklist for Children (TSCC), FACES-IV, and FCS scores at evaluation-periods (baseline, after 6 months, after 1 year), including treatment option as a covariant. To adjust for missing data, we analyzed by linear mixed model and we used the Bonferroni method for post hoc test between each evaluation-periods. We performed the chi-square test to compare the diagnostic changes after 1 year between groups with and without PTSD. All statistical analyses were performed using SPSS (Statistical Package for the Social Science) 25.0 version (IBM Corp., Armonk, NY, USA).
RESULTS
We included data from 28 participants (4 boys and 24 girls) in the analysis. The mean age of the participants at baseline was 12.00±4.40 years, whereas that at the time of the first CSA incident was 10.04±4.14 years. The mean IQ was 86.25± 16.71 with 6 participants presenting an IQ <70.
Among the participating 28 CSA victims, nine received no treatment and two received only art therapy (non-EBT group). The other 17 participants received trauma-focused EBT (EBT group). Information on demographics by treatment options was added as a Supplementary Table 1 (in the online-only Data Supplement).
Trauma Symptom Checklist for Young Children
TSCYC scores were analyzed in 15 subjects who appropriate age range (3–13 years old) during evaluation period. In the parent-reported TSCYC, posttraumatic stress (PTS)-intrusion, PTS-avoidance, PTS-arousal, and PTS-total domain scores showed significant changes based on assessment time. Comparison of the scores of each domain across the three time points (initial vs. after 6 months vs. after 1 year) indicated the following, respectively: PTS-intrusion (66.00±3.70 vs. 55.24±4.18 vs. 49.41±4.65), PTS-avoidance (76.42±4.93 vs. 65.96±5.59 vs. 52.40±6.26), PTS-arousal (55.22±3.14 vs. 61.35±3.40 vs. 51.64±3.64), and PTS-total (67.50±3.57 vs. 62.28±3.98 vs. 48.92±4.37). Other symptom domain scores are listed in the Supplementary Table 2 (in in the online-only Data Supplement). In the post hoc comparison, there were significant differences between the initial PTS-intrusion, PTS-avoidance, and PTS-total domain scores and those 1 year later. Further, there was significant difference between the 6-month and 1-year scores of PTS-arousal domain (Figure 2). These results of decreased scores in the PTS domains suggest that the trauma-related symptoms in the child observed by the caregiver decreased over time after the CSA. In particular, the avoidance domain had a clinically meaningful level with a T-score of 70 or higher in the initial evaluation, but the status appeared to have improved in the evaluation 1 year later. Although most of the PTS-related domain scores were not above the clinically significant level at the initial, the reported scores decreased over time. These results indicate the children’s psychological states get better. In addition, PTSarousal domain scores decreased at the time of evaluation between after 6 months and at the time after 1 year. Considering this aspect, it is thought that the recovery course will be different depending on the symptom domain. No significant interaction between treatment conditions and time progression was observed in TSCYC.
Trauma Symptom Checklist for Children
TSCC scores were analyzed in 16 subjects who appropriate age range (8–16 years old) during evaluation period. In the child-reported TSCC, none of the domains showed a difference based on assessment time (Supplementary Table 3 in the online-only Data Supplement).
Although no progressive change with time was observed in TSCC, an interaction between treatment condition and time progression was significantly observed. In anxiety and posttraumatic stress symptom domains, the symptom scores decreased more in the EBT group over time. The estimated mean values (±standard error) for the anxiety domain score were 63.60±4.99 (initial), 50.90±5.97 (after 6 months), and 57.64±6.93 (after 1 year) in the EBT group; and 41.00±6.44 (initial), 52.84±6.81 (after 6 months), and 51.17±6.44 (after 1 year) in the non-EBT group. Those of the posttraumatic stress symptom domain scores were 60.40±3.44 (initial), 50.03± 4.29 (after 6 months), and 47.56±5.11 (after 1 year) in the EBTgroup; and 40.00±4.44 (initial), 49.35±4.78 (after 6 months), and 46.17±4.44 (after 1 year) in the non-EBT group (Table 1). This means that the EBT group showed a greater improvement in posttraumatic symptoms for 1 year.
Family Adaptability and Cohesion Evaluation Scales IV
Regarding the FACES-IV findings, the flexibility and total circumplex ratio significantly increased with time progression. The flexibility ratios were 1.63±0.18 (initial), 2.06±0.19 (after 6 months), and 2.34±0.19 (after 1 year), whereas the respective total circumplex ratios were 1.55±0.20 (initial), 1.93± 0.20 (after 6 months), and 2.08±0.20 (after 1 year) (p<0.05). The cohesion ratios were 1.59±0.27 (initial), 1.88±0.27 (after 6 months), and 1.89±0.27 (after 1 year). There were significant differences in the post hoc comparison, also (Table 2). Indices of family function have been gradually increasing both after 6 months and after 1 year compared to the initial evaluation, suggesting progressive improvement in family functioning.
Family Communication Scale
In the FCS, there were significant differences in the total communication scores obtained at initial, after 6 months, and after 1-year assessments (Table 2). The total communication scores were 34.38±1.52 (initial), 36.36±1.53 (after 6 months), and 36.06±1.53 (after 1 year). Especially, in FCS there was a significant difference between the initial and 6-months later in the post hoc comparison, which means that family dialogue and communication increased during the early recovery period after the CSA.
Diagnostic data
Regarding initial diagnostic evaluation based on the KSADS-PL, five participants had no psychiatric illness, 14 had PTSD with or without depression, five had depressive disorder not otherwise specified (NOS), two had adjustment disorder, one had anxiety disorder, and one had enuresis. Regarding diagnostic re-evaluation after the first year, 17 participants had no psychiatric illness, nine had PTSD with or without depression, one had depressive disorder NOS, and one had attention-deficit/hyperactivity disorder.
Among the 14 participants diagnosed with PTSD at the initial diagnostic evaluation, five (35.7%) showed improvement or resolution of the symptoms, nine maintained their PTSD diagnosis. Whereas among the nine participants with a psychiatric diagnosis other than PTSD at initial assessment, eight (88.9%) were not diagnosed with any psychiatric illness after 1 year (p<0.05) (Figure 3). All diagnostic changes are listed in the supplement (Supplementary Table 4 in the online-only Data Supplement).
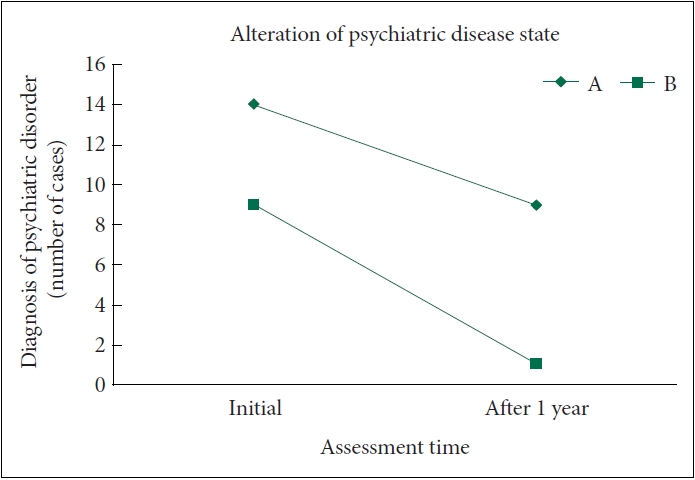
Alteration of the psychiatric disease state (PTSD vs. non-PTSD) of the participants in the first year. A: PTSD with/without depressive disorder at initial assessment (N=14); B: non-PTSD (depressive disorder not otherwise specified, adjustment disorder, enuresis) at initial assessment (N=9). 64.3% of group A (nine cases), and 11.1% of group B (one case) remained in the disease state after a year. χ2 test, p=0.029. PTSD, posttraumatic stress disorder.
DISCUSSION
We examined changes in the symptoms scale scores over time by obtaining repeated measurements of child and caregiver self-report scales at different evaluation-periods. Contrary to the hypothesis that various psychological symptoms will continue after CSA, most of the symptoms reported in TSCYC and TSCC were below the clinical cut-off value (Tscore 65), and no change over time. But, in some domains (dissociation in TSCYC, dissociation-fantasy, and sexual distress in TSCC), the estimated mean scores slightly increased in the evaluation 6 months after the initial assessment, although the difference over time was not significant. It means a possibility that the change in symptoms is not significant enough.
Instead, score changes were observed in PTS-related symptom domains that were above the clinical cutoff score. Most of the PTS-related symptoms of TSCYC showed a progressive decrease, and in the post hoc test PTS-intrusion and PTSavoidance symptoms scores showed a significant decrease 1 year after, and PTS-arousal symptoms showed a significant change between 6 months to 1 year after. Unlike our hypothesis, PTS-related symptoms were observed to gradually improve over time, but since each symptom domain shows different recovery patterns, it seems that management and monitoring plans for victims should be considered these results. Because significant differences in this study were observed after a 1-year follow-up, recovery of trauma-related symptoms seems to require at least a year. Therefore, it is thought that care plans to help the child’s recovery will need more than a year period.
In addition, although below the clinical cutoff level, it is necessary to consider also that the sexual preoccupation domain score is high during the initial evaluation in TSCC. TSCC is a good measure of the subjectively felt sexual discomfort of children, which cannot be observed by parents, and it is sensitive to the evaluation of sexual symptoms related to sexual abuse [56]. A previous study of Korean children showed that the response score tended to be somewhat lower than that of the United States [56]. Therefore, even if the high score observed in the initial evaluation is lower than the clinical cutoff, it needs to be considered. Furthermore, the sexual concerns domain scores of TSCYC have little changes until 6 months, either. So, the persistence of the symptoms should be considered. If the child’s discomfort related to sexual concerns persists, healthy socio-psychological development is difficult [62,63], so it is thought that active intervention and management for these aspects are needed.
Moreover, we observed interesting changes in the child-reported TSCC scores. There were significant interactions between time progression and treatment condition in the anxiety and PTS-symptom domains in the TSCC. The significant improvements in these domains can be interpreted as the EBTs being useful to help recovery. Although the EBT group in this study had a limitation that various treatment methods were mixed, the changes observed in the study support the effect that EBT reduces trauma-related symptoms such as PTS symptoms and anxiety [64-66]. Therefore, when choosing a treatment plan for victimized children, the EBTs should be considered primary options of treatments.
To investigate familial changes after CSA, we used the FACEIV and FCS. We found a continual increase in the flexibility and total circumplex ratio at each time point, these results indicate progressive improvement in family functioning. Flexibility refers to the ability to restructure their family systems in response to situational stress [58]. The increased flexibility ratio observed in this study implies that the family’s relationships become more flexible and seek appropriate adaptation after CSA. The total circumplex ratio also shows a steady increase over time, indicating an improving balance of family functions [58]. In the FCS, a significant increase was observed it means increasing positive communication between their members.
In this study, the family showed positive changes gradually, in contrast to the hypothesis that CSA would cause negative changes in the family. Anggraini et al. [41] reported changes in parenting patterns, including problem handling skills, awareness of their child’s emotions, and communication in CSA victim families. Anggraini et al. [41]’s study also showed that the family’s ability to deal with problems after CSA damage improved. The positive changes in the family observed in this study can also be interpreted as improved problem-solving skills through family members experiencing a common crisis, which indicates the resilience of the family.
Because proper support of primary caregivers is important for the prevention of PTSD among children after CSA [67], it is encouraging that the early changes in FCS were meaningful. A typical family therapy session was not provided in all cases in this study, but we briefly provided guidance on communication to help stabilize the victims of all children and families visiting the Sunflower center for children. Therefore, it is also possible that the current results were influenced by this initial psychoeducation. Thus, we believe that strategies to restore the function of the family are actively needed from the start of the intervention.
We observed that 23 of our participants showed at least one psychiatric disease at the initial assessment. The most common disorder was PTSD with or without depression, which was diagnosed in 14 victims with about 64.3% of them retaining the diagnosis at the 1-year follow up. This demonstrated that PTSD was more persistent than non-PTSD diagnoses, such as depressive disorder NOS and adjustment disorder (Figure 3). Unlike changes in PTSD symptom-related scales observed in TSCYC, PTSD diagnosis tends to persist over 1 year. A cohort study on 480 CSA survivors conducted by Elklit68 reported that 78% of participants were diagnosed with PTSD at baseline with 40% retaining the diagnosis after 12 months. Although there is considerable variation in the PTSD recovery course after CSA, the aforementioned findings demonstrate the persistence of PTSD diagnosis. This is consistent with our findings of greater persistence of PTSD diagnosis after 1 year than that of other diseases. Therefore, additional long-term management plans are needed for victims who have sufficient symptoms to be diagnosed with PTSD.
We did not observe any new PTSD diagnoses within 1 year, which was unrelated to whether or not the victim received a therapeutic intervention. Some studies on late-onset PTSD have reported changes in the diagnoses 12–18 months after the incident;38 therefore, it is necessary to continually monitor the recovery course and re-assess diagnoses beyond 1 year.
Limitations
This study has several limitations. First, we had a small sample size. Although the investigators applied active effort during cohort recruitment, recruiting a large cohort was difficult due to the cautious and defensive attitude of CSA victims and their caregivers. However, despite the small sample size, we conducted a follow-up study on changes in symptoms over time in the same children. Further, we accounted for missing data due to input error, omission, or caregiver absence in the statistical analysis. Second, this was a single-center study conducted at The Seoul Sunflower Center for children. Thus, the participants were largely restricted to the residents in Seoul metropolitan city, which limited the generalizability of our results. Future multi-centered studies could provide a broader perspective on the management and progression of CSA victims in South Korea. Fourth, the treatments provided to the participants in this study were non-structured treatments. Since this study is not intended to compare the effects of each treatment method, the EBT group was defined when satisfied with the minimum conditions. Therefore, it is necessary to conduct a more controlled design study in the future to compare the direct effects of each treatment. Finally, we applied a relatively short follow-up duration of 1 year. Follow-up assessment of this cohort is currently underway and we plan to report on long-term changes in further studies.
Supplementary Materials
The online-only Data Supplement is available with this article at https://doi.org/10.30773/pi.2022.0065.
Characteristics of the participants by treatment condition
Changes in the parent-reported Trauma Symptom Checklist for Young Children scores with time progression
Changes in the child-reported Trauma Symptom Checklist for Children scores with time progression
Diagnostic changes of all participants
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: all authors. Data curation: Na-Hyun Lee, Kyungyoon Kim, Dong-Ho Song. Formal analysis: Na-Hyun Lee, Junghan Lee, Kyung-yoon Kim. Funding acquisition: Dong-Ho Song. Investigation: Na-Hyun Lee, Kyung-yoon Kim. Methodology: all authors. Project administration: Kuen-Ah Cheon, Dong-Ho Song. Resources: all authors. Supervision: Kuen-Ah Cheon, Dong-Ho Song. Validation: all authors. Writing—original draft: Na-Hyun Lee, Kyung-yoon Kim. Writing—review & editing: all authors.
Funding Statement
This study was supported by a grant of the Korea Mental Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (HM14C2611).



