1. Moffitt TE, Caspi A, Taylor A, Kokaua J, Milne BJ, Polanczyk G, et al. How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychol Med 2010;40:899-909.


2. McGlashan TH. The borderline syndrome. II. Is it a variant of schizophrenia or affective disorder? Arch Gen Psychiatry 1983;40:1319-1323.


3. Pope HG Jr, Jonas JM, Hudson JI, Cohen BM, Gunderson JG. The validity of DSM-III borderline personality disorder. A phenomenologic, family history, treatment response, and long-term follow-up study. Arch Gen Psychiatry 1983;40:23-30.


4. Frances A, Clarkin JF, Gilmore M, Hurt SW, Brown R. Reliability of criteria for borderline personality disorder: a comparison of DSM-III and the diagnostic interview for borderline patients. Am J Psychiatry 1984;141:1080-1084.


5. Perry JC. Depression in borderline personality disorder: lifetime prevalence at interview and longitudinal course of symptoms. Am J Psychiatry 1985;142:15-21.


6. Zanarini MC, Frankenburg FR, Dubo ED, Sickel AE, Trikha A, Levin A, et al. Axis I comorbidity of borderline personality disorder. Am J Psychiatry 1998;155:1733-1739.


7. Chanen AM, Berk M, Thompson K. Integrating early intervention for borderline personality disorder and mood disorders. Harv Rev Psychiatry 2016;24:330-341.


9. Stringer B, van Meijel B, Eikelenboom M, Koekkoek B, Licht CM, Kerkhof AJ, et al. Recurrent suicide attempts in patients with depressive and anxiety disorders: the role of borderline personality traits. J Affect Disord 2013;151:23-30.


11. Hurt SW, Clarkin JF. Borderline personality disorder: prototypic typology and the development of treatment manuals. Psychiatr Ann 1990;20:13-18.

12. Morey LC. The personality assessment inventory professional manual. Odessa: Psychological Assessment Resources; 1991.
13. Kernberg OF, Yeomans FE. Borderline personality disorder, bipolar disorder, depression, attention deficit/hyperactivity disorder, and narcissistic personality disorder: practical differential diagnosis. Bull Menninger Clin 2013;77:1-22.


14. Ruggero CJ, Zimmerman M, Chelminski I, Young D. Borderline personality disorder and the misdiagnosis of bipolar disorder. J Psychiatr Res 2010;44:405-408.


15. Zeng R, Cohen LJ, Tanis T, Qizilbash A, Lopatyuk Y, Yaseen ZS, et al. Assessing the contribution of borderline personality disorder and features to suicide risk in psychiatric inpatients with bipolar disorder, major depression and schizoaffective disorder. Psychiatry Res 2015;226:361-367.


17. Bremne JD, Vermetten E. Stress and development: behavioral and biological consequences. Dev Psychopathol 2001;13:473-489.


18. Mello MF, Faria AA, Mello AF, Carpenter LL, Tyrka AR, Price LH. Childhood maltreatment and adult psychopathology: pathways to hypothalamic-pituitary-adrenal axis dysfunction. Braz J Psychiatry 2009;31 Suppl 2:S41-S48.

19. Middlebrooks JS, Audage NC. The effects of childhood stress on health across the lifespan. Atlanta: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2008.
20. Cicchetti D. Socioemotional, personality, and biological development: illustrations from a multilevel developmental psychopathology perspective on child maltreatment. Annu Rev Psychol 2016;67:187-211.


21. Zanarini MC, Williams AA, Lewis RE, Reich RB, Vera SC, Marino MF, et al. Reported pathological childhood experiences associated with the development of borderline personality disorder. Am J Psychiatry 1997;154:1101-1106.


22. Lobbestael J, Arntz A, Bernstein DP. Disentangling the relationship between different types of childhood maltreatment and personality disorders. J Pers Disord 2010;24:285-295.


24. Aaltonen KI, Rosenström T, Baryshnikov I, Karpov B, Melartin T, Suominen K, et al. Mediating role of borderline personality disorder traits in the effects of childhood maltreatment on suicidal behaviour among mood disorder patients. Eur Psychiatry 2017;44:53-60.


25. Carr CP, Martins CM, Stingel AM, Lemgruber VB, Juruena MF. The role of early life stress in adult psychiatric disorders: a systematic review according to childhood trauma subtypes. J Nerv Ment Dis 2013;201:1007-1020.

26. Jaworska-Andryszewska P, Rybakowski JK. Childhood trauma in mood disorders: neurobiological mechanisms and implications for treatment. Pharmacol Rep 2019;71:112-120.


27. Güleç MY, Altintaş M, İnanç L, Bezgin CH, Koca EK, Güleç H. Effects of childhood trauma on somatization in major depressive disorder: the role of alexithymia. J Affect Disord 2013;146:137-141.


28. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed). Arlington: American Psychiatric Association; 2013.
29. Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998;59 Suppl 20:22-33.

30. Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, et al. Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse Negl 2003;27:169-190.


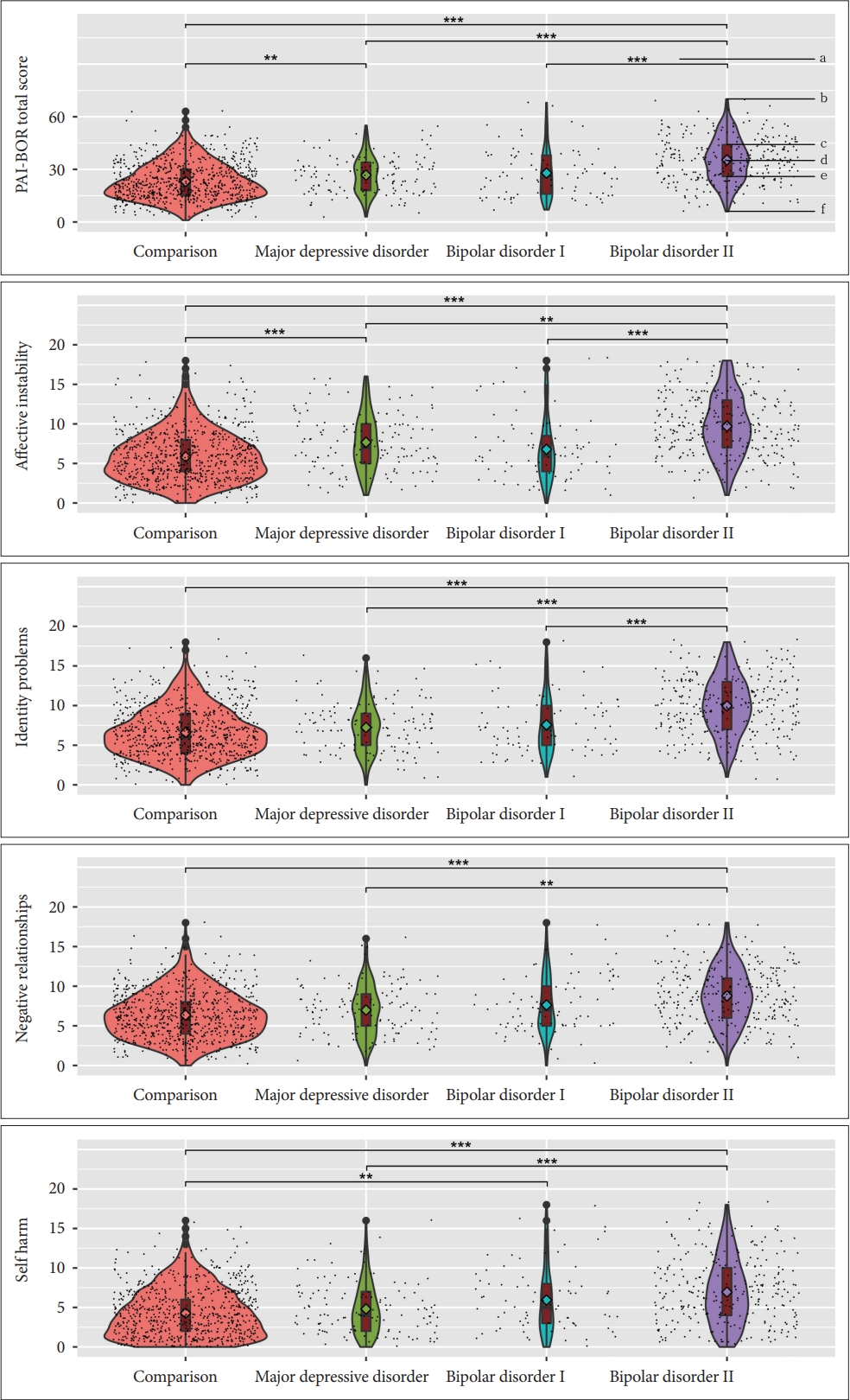
31. Socada JL, Söderholm JJ, Rosenström T, Ekelund J, Isometsä E. Presence and overlap of bipolar symptoms and borderline features during major depressive episodes. J Affect Disord 2021;280(Pt A):467-477.


33. Paris J, Gunderson J, Weinberg I. The interface between borderline personality disorder and bipolar spectrum disorders. Compr Psychiatry 2007;48:145-154.


34. Herman JL, Perry JC, van der Kolk BA. Childhood trauma in borderline personality disorder. Am J Psychiatry 1989;146:490-495.


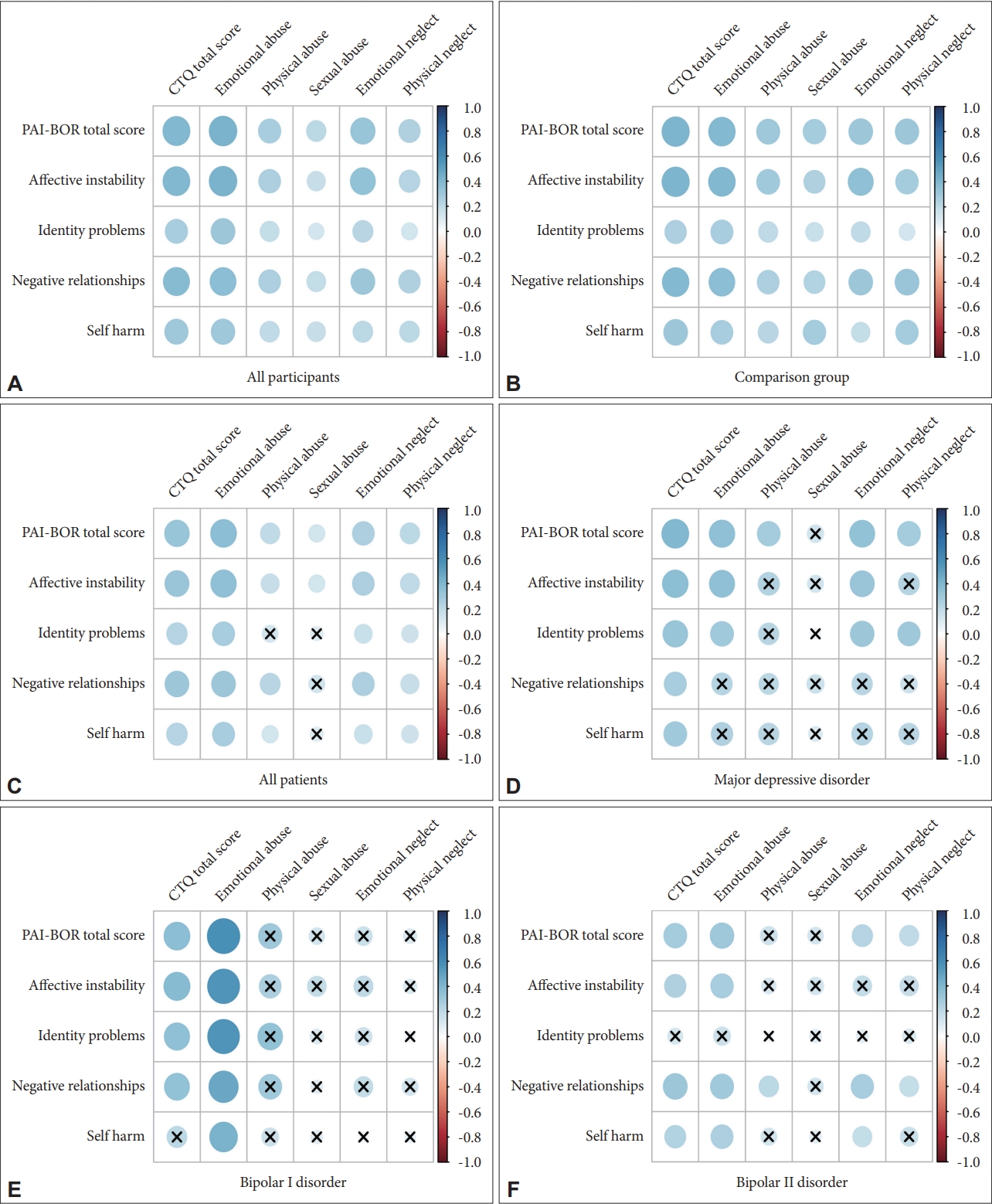
35. Baryshnikov I, Joffe G, Koivisto M, Melartin T, Aaltonen K, Suominen K, et al. Relationships between self-reported childhood traumatic experiences, attachment style, neuroticism and features of borderline personality disorders in patients with mood disorders. J Affect Disord 2017;210:82-89.


37. Martín-Blanco A, Ferrer M, Soler J, Salazar J, Vega D, Andión O, et al. Association between methylation of the glucocorticoid receptor gene, childhood maltreatment, and clinical severity in borderline personality disorder. J Psychiatr Res 2014;57:34-40.


38. Perroud N, Zewdie S, Stenz L, Adouan W, Bavamian S, Prada P, et al. Methylation of serotonin receptor 3A in ADHD, borderline personality, and bipolar disorders: link with severity of the disorders and childhood maltreatment. Depress Anxiety 2016;33:45-55.


39. Dammann G, Teschler S, Haag T, Altmüller F, Tuczek F, Dammann RH. Increased DNA methylation of neuropsychiatric genes occurs in borderline personality disorder. Epigenetics 2011;6:1454-1462.


41. Thaler L, Gauvin L, Joober R, Groleau P, de Guzman R, Ambalavanan A, et al. Methylation of BDNF in women with bulimic eating syndromes: associations with childhood abuse and borderline personality disorder. Prog Neuropsychopharmacol Biol Psychiatry 2014;54:43-49.


42. Battle CL, Shea MT, Johnson DM, Yen S, Zlotnick C, Zanarini MC, et al. Childhood maltreatment associated with adult personality disorders: findings from the Collaborative Longitudinal Personality Disorders Study. J Pers Disord 2004;18:193-211.


43. Johnson JG, Smailes EM, Cohen P, Brown J, Bernstein DP. Associations between four types of childhood neglect and personality disorder symptoms during adolescence and early adulthood: findings of a community-based longitudinal study. J Pers Disord 2000;14:171-187.


44. de Aquino Ferreira LF, Queiroz Pereira FH, Neri Benevides AML, Aguiar Melo MC. Borderline personality disorder and sexual abuse: a systematic review. Psychiatry Res 2018;262:70-77.


46. Goodman M, Weiss DS, Koenigsberg H, Kotlyarevsky V, New AS, Mitropoulou V, et al. The role of childhood trauma in differences in affective instability in those with personality disorders. CNS Spectr 2003;8:763-770.


49. Beck AT, Davis DD, Freeman A. Cognitive therapy of personality disorders (3rd ed). New York: Guilford Press; 2015.
50. Lu W, Mueser KT, Rosenberg SD, Jankowski MK. Correlates of adverse childhood experiences among adults with severe mood disorders. Psychiatr Serv 2008;59:1018-1026.


52. Jaworska-Andryszewska P, Rybakowski JK. Childhood adversity and clinical features of bipolar mood disorder. Arch Psychiatry Psychother 2018;20:13-19.


54. Merza K, Papp G, Kuritárné Szabó I. The role of childhood traumatization in the development of borderline personality disorder in Hungary. Eur J Psychiatry 2015;29:105-118.