Risk and Protective Factors for Childhood Physical Abuse and Suicidal Ideation: The Effect of Brain-Derived Neurotrophic Factor Polymorphism and Social Support
Article information
Abstract
Objective
This study aimed to explore the relationship between childhood physical abuse and suicidal ideation considering the effects of genetic and environmental factors in patients with post-traumatic stress disorder (PTSD) by focusing on brain-derived neurotrophic factor (BDNF) polymorphism and social support, respectively.
Methods
One-hundred fourteen patients with PTSD and 94 healthy controls (HCs) were genotyped with respect to BDNF Val66Met polymorphism. All participants underwent psychological assessments. The hierarchical regression analysis and the simple slope analysis were conducted.
Results
As for patients with PTSD, the moderation effect of BDNF polymorphism was significant but not for social support. Specifically, the BDNF Val/Val genotype worked as a risk factor and strengthens the relationship between childhood physical abuse and suicidal ideation. As for the HCs, the significant moderation effect was found only in social support, but not for BDNF polymorphism. The relationship between childhood physical abuse and suicidal ideation was weakened for the HCs with high social support.
Conclusion
This study demonstrated a significant BDNF genetic vulnerability for suicide in patients with PTSD who experienced childhood physical abuse. Our results suggested that social support provided a mitigating effect on the relationship between childhood physical abuse and suicidal ideation only in the HCs.
INTRODUCTION
Post-traumatic stress disorder (PTSD) is a mental illness caused by exposure to stressful life events, which is influenced by both genetic and environmental factors [1]. Among various traumatic life events, childhood physical abuse is a major risk factor for suicidal behavior [2-8]. Continued physical abuse could make children feel that their safety is threatened and conclude that the repeated abuse is inevitable [9], which may lead to hopelessness [10] and a sense of isolation that could increase the risks of suicide [11]. Moreover, repeated physical abuse can lead to the habituation of fear and pain from physical injury, resulting in more serious and frequent suicide attempts [6].
Brain-derived neurotrophic factor (BDNF) is one of the strong candidate genes associated with suicide [12-14] as well as a biomarker of suicidal behavior [15-17]. In particular, the BDNF plays a role in regulating various neurological systems and recovering neural networks [18,19]. The BDNF is also linked to several neuro-biochemical systems; thus, it could be an important marker in understanding complex suicidal behavior.
The risk genotype (or allele) of the BDNF gene is not wellestablished. Previous studies indicated that Met allele [20-23] of BDNF gene had shown negative effects on suicidal behavior, whereas others reported the Val allele of BDNF gene as a risk factor for suicidal behavior [14,24]. Provided that, it is less likely that a specific genotype could be conceptualized as either simply “good” or “bad” [25]. Rather, it could be understood as more responsive (plasticity) or less responsive (static) to certain stressful environments [26]. Interestingly, the interaction between BDNF gene and early life environmental factors have been significantly related to suicidal behavior [21,22,27].
Social support is an environmental protective factor that alleviates the risk of suicide [28]. Social support is directly related to lower suicidal ideation [29] and is indirectly protective against suicidal behavior as a booster for other protective factors, including self-esteem [30] and sense of belonging [31]. In addition, social support is thought to buffer against developing the psychiatric symptoms in adulthood among individuals who were exposed to childhood abuse [32].
However, the protective effects of social support on psychiatric symptoms might be inapplicable to individuals who experienced severe child abuse. Social support seems to play an insignificant role as a prophylactic among those who had suffered severe physical abuse [33]. The attempts to understand the protective effects of social support have been through factoring in other genetic factors or interactions as well as environmental factors. Specifically, individuals with high biochemical response sensitivity to stress are more likely to develop PTSD and attempt suicide [34], suggesting the heritability of such tendencies [35].
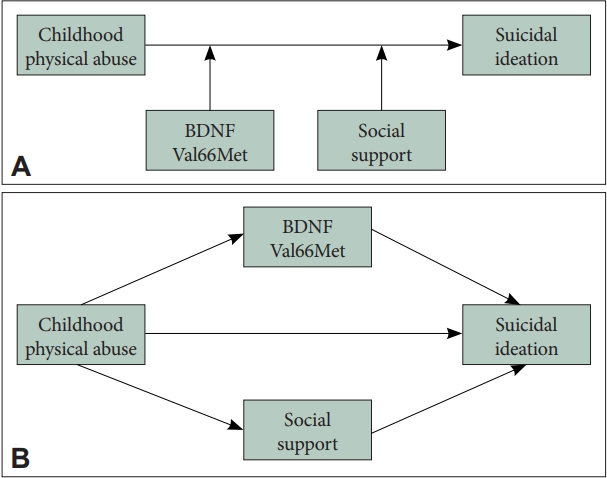
This study aimed to explore the influence of childhood physical abuse on suicide behavior concerning BDNF polymorphism and social support as risk and protective factors in patients with PTSD and healthy controls (HCs). Given the studies suggesting various factors influencing suicidal behavior, it seems valid to comprehensively evaluate the relative effects of genetic and environmental factors [36]. To demonstrate the possible effect of social support and BDNF polymorphism on the relationship between physical abuse and suicidal ideation: one hypothesized its moderation effect and the other its mediation (Figure 1).
METHODS
Participants
Patients with PTSD were recruited from the Psychiatry Department of the Inje University Ilsan Paik Hospital in Goyang, Republic of Korea. The diagnosis of PTSD was based on the Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) by a board-certified psychiatrist [37]. Patients were excluded if they had a history of any psychiatric and/or neurological illness other than PTSD, such as schizophrenia, bipolar disorder, anorexia nervosa, intellectual disability, epilepsy, etc. Healthy individuals were recruited from the general population through flyers and posters as a control group. The inclusion criteria required participants to have neither history of major trauma (e.g., a serious car accident, combat experience, sexual assault, or serious physical injury) nor medications due to any psychological disorders. A total of 253 participants (patients with PTSD=n, HCs=n) were enrolled in the study. A total of 45 individuals were excluded for the following reasons: 13 individuals for not attempting or completing the psychological scale, 18 individuals with high scores for denial on the Childhood Trauma Questionnaire (CTQ), 12 individuals with severe brain damage, and 2 individuals with missing genetic data. Consequently, 114 patients with PTSD and 94 HCs were included in the analysis. The patients with PTSD were composed of 36 men (31.6%) and 78 women (68.4%), with an average age of 44.36 years (standard deviation [SD]=12.77) and average education of 12.78 years (SD=3.21). The participants in the HCs consisted of 27 men (28.7%) and 67 women (71.3%), with an average age of 47.21 years (SD=13.81) and average education of 13.81 years (SD=3.14). Each participant signed an informed consent form and a separate genetic informed consent form approved by the Institutional Review Board at Inje University Ilsan Paik Hospital before participating (IRB No. 2015-07-025).
Psychological measures
Childhood Trauma Questionnaire
The Korean validated version of the CTQ was used to evaluate childhood physical abuse [38]. The CTQ is a retrospective self-report questionnaire of childhood trauma [39] using five subscales– emotional abuse, physical abuse, sexual abuse, emotional neglect, and physical neglect, as well as another scale for detecting minimization and denial [40]. The CTQ consists of 28 items and is assessed with a 5-point Likert scale ranging from 1 (“never true”) to 5 (“very often true”). The coefficient alpha of the CTQ was 0.79 and the coefficient alpha of the childhood physical abuse subscales was 0.90 in patients with PTSD. The coefficient alpha of the CTQ was 0.72 and the coefficient alpha of the childhood physical abuse subscales was 0.84 in HCs.
Scale for Suicidal Ideation
The Korean validated version of the Scale for Suicidal Ideation (SSI) was used to evaluate suicidality [41]. The scale consists of 19 items and is assessed using a 3-point Likert scale ranging from 0 to 2. The coefficient alpha of the scale was 0.91 in patients with PTSD and 0.89 in the HCs.
Clinician-Administered PTSD Scale for DSM-5
The CAPS-5 is a structured diagnostic interview by a psychiatrist based on the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition diagnosis for PTSD. It was used to evaluate the frequency and severity of PTSD symptoms [37]. The CAPS-5 consists of 30 items and is assessed by standardizing and simplifying the conversion of symptom frequency and intensity on a 5-point Likert scale ranging from 0 (“Absent”) to 4 (“Extreme/incapacitating”) as well as dichotomous scores (“Yes” or “No”). It showed good internal consistency, interrater reliability, and test-retest reliability [37]. The coefficient alpha of the CAPS-5 severity score was 0.80 in patients with PTSD and 0.83 in the HCs.
DUKE-UNC Functional Social Support Questionnaire
The Korean validated version of the self-reported DUKEUNC Functional Social Support Questionnaire was used to evaluate the level of social support [42]. The scale consists of a total of 13 questions rated on a Likert scale ranging from 1 (“much less than desired”) to 5 (“as much as desired”). Higher scores indicate that higher social support is perceived by the respondent. The coefficient alpha of the scale was 0.93 in patients with PTSD and 0.90 in the HCs.
Brain-derived neurotrophic factor genotyping
The BDNF rs6265 (Val66Met) single nucleotide polymorphism (SNP) has been suggested as a relevant predictor of suicidal behavior [23,43,44] and a risk factor for suicidal behavior in the adult population for candidate gene analyses [21,22,27]. Genomic DNA was extracted from peripheral blood provided by participants and quality was checked using NanoDrop® ND-1000 UV-Vis Spectrophotometer (NanoDrpo Technologies, Wilmington, DE, USA). Genotyping was conducted with polymerase chain reaction amplification and allelic discrimination using TaqMan® SNP Genotyping Assays obtained from Applied Biosystems (Foster City, CA, USA) and ABI PRISM 7900HT Real-Time PCR system (Applied Biosystems) [45].
Three positive and one negative control samples were present for each plate, and we confirmed positive controls with a clustering image. Intra-genomic DNA (gDNA) samples of known genotypes were used for positive control. Genotype frequencies for each polymorphism were calculated and evaluated by the Hardy–Weinberg equilibrium to check the data quality and genotype error. All statistical tests and visualization of genes were conducted using R version 3.3.3 (R Foundation for Statistical Computing, Vienna, Austria).
Statistical analysis
The genotypic distributions of the BDNF polymorphism were evaluated by the Hardy–Weinberg equilibrium. Normality was tested using skewness and kurtosis. Skewness less than 3.0 and kurtosis less than 7.0 were considered acceptable for moderate normal distribution [46]. All variables in our results were normally distributed. After checking for normality, regression analysis was performed to examine the moderation and mediation effects of BDNF Val66Met SNP and social support on the path between childhood physical abuse and suicidal ideation using SPSS (IBM Corp., Armonk, NY, USA) and the SPSS Macro PROCESS for SPSS 4.0.0 [47]. Age, sex, and years of education were controlled as covariates. Subsequently, the simple slope analysis [48] was performed to prove interaction. This analysis estimates the effects of the predictor variable (i.e., childhood physical abuse) on the outcome variable (i.e., suicidal ideation) at low (one SD below the mean), moderate (sample mean), and high (one SD above the mean) values of the moderator (i.e., BDNF Val66Met and social support). All significant levels were set at p<0.05 (two-tailed).
RESULTS
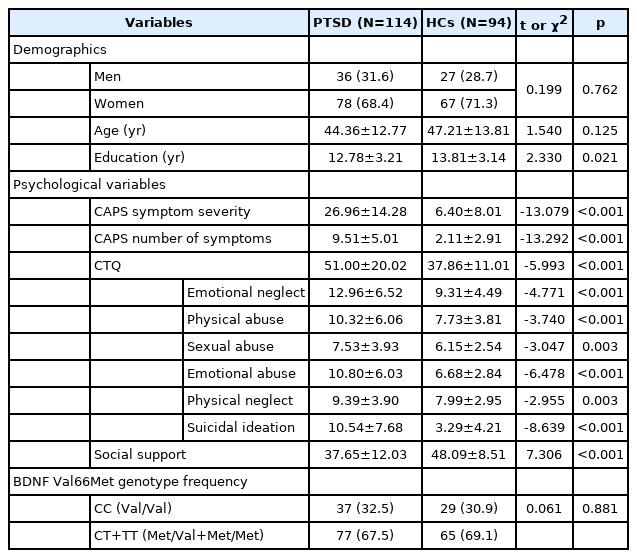
Descriptive statistics
Demographics, psychological characteristics, and the genotype frequencies of the BDNF Val66Met in PTSD and HCs groups are presented in Table 1. Years of education of patients with PTSD were significantly lower than HCs (12.78±3.21 versus 13.81±3.14, p=0.021, respectively). The scores of CAPS symptom severity was significantly higher in the patients with PTSD than HCs (26.96±14.28 versus 6.40±8.01, p<0.001). The CTQ and scale for suicidal ideation were also significantly higher in the patients with PTSD than the HCs (51.00± 20.02 versus 37.86±11.01, p<0.001; 10.54±7.68 versus 3.29±4.21, p<0.001, respectively). Additionally, social support was significantly lower in patients with PTSD (37.65±12.03 versus 48.09± 8.51, p<0.001, respectively). There was no significant difference in genotype frequency of BDNF Val66Met between the two groups. The genotypic distributions of the BDNF Val66Met did not deviate from the Hardy-Weinberg equilibrium (p>0.05) [49].
Moderation and mediation effects
In moderation analyses, there was a significant moderation effect of BDNF Val66Met on the relationship between childhood physical abuse and suicidal ideation in patients with PTSD (Table 2 and Figure 2). More specifically, the moderation model was significant in patients with PTSD (R2=0.258, p<0.001). The main effect of childhood physical abuse and interaction effect of childhood physical abuse and BDNF Val66Met predicted the suicidal ideation (B=1.267, t=2.372, p=0.020; B=-0.640, t=-2.886, p=0.005, respectively). However, the other two main effects of BDNF Val66Met and social support were not significant. Additionally, the interaction effect of childhood physical abuse and social support did not predict suicidal ideation.

Moderation analysis examining effects of BDNF Val66Met polymorphism and social support on the relationship between childhood physical abuse and suicidal ideation
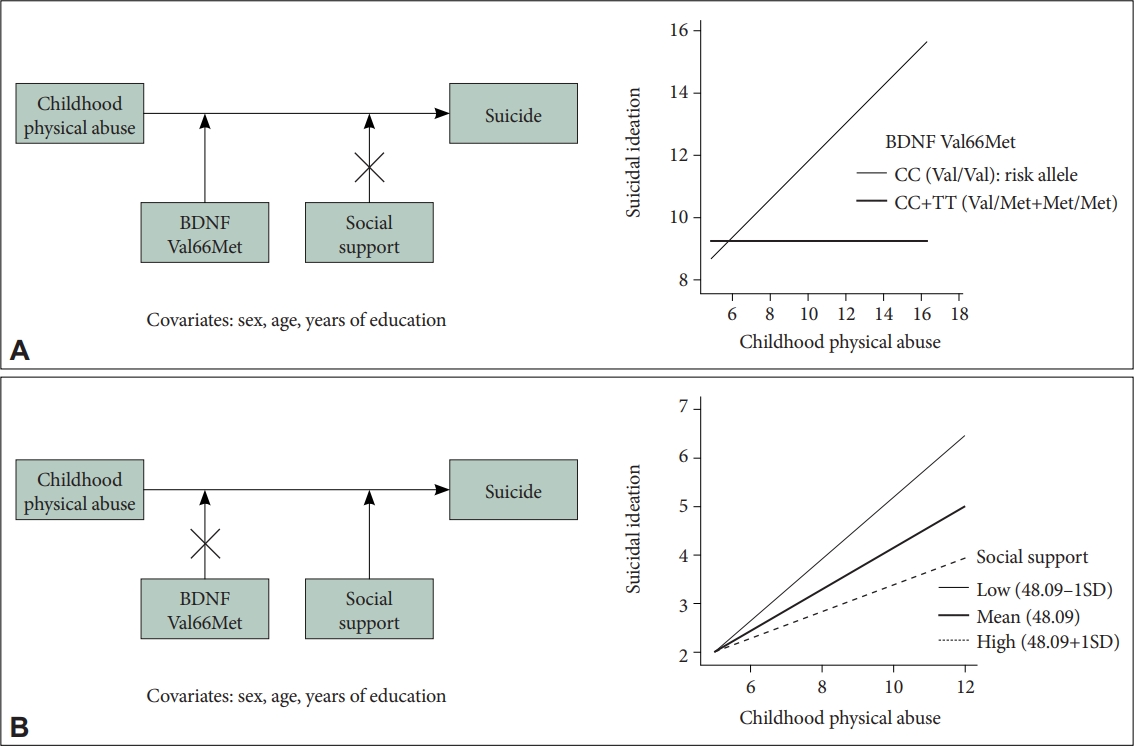
The moderation effect of BDNF Val66Met and social support on the relationship between childhood physical abuse and suicidal ideation. A: Post-traumatic stress disorder group (N=114). B: Healthy controls group (N=94). BDNF, brain-derived neurotrophic factor; SD, standard deviation.
In addition, there was a significant moderation effect of social support on the relationship between childhood physical abuse and suicidal ideation in HCs (Table 2 and Figure 2). More specifically, the moderation model was significant in the HCs (R2=0.319, p<0.001). The main effect of childhood physical abuse and interaction effect of childhood physical abuse and social support predicted suicidal ideation (B=2.315, t=3.098, p=0.003; B=-0.023, t=-2.151, p=0.034, respectively). However, the other two main effects of BDNF Val66Met and social support were not significant. Additionally, the main effect of BDNF Val66Met and the interaction effect of childhood physical abuse and BDNF Val66Met did not predict suicidal ideation.
In mediation analyses, there were no significant effects of social support and BDNF polymorphism on the association between childhood physical abuse and suicidal ideation (Supplementary Table 1 in the online-only Data Supplement).
Probing an interaction
The results from the simple slope analysis indicated that there was a significant positive relationship between childhood physical abuse and suicidal ideation in PTSD patients with Val/Val genotype at all levels (i.e., low, average, high) of social support (B=0.604, t=2.909, p=0.004; B=0.593, t=3.417, p=0.001; B=0.582, t=2.600, p=0.011). In contrast, this relationship was not identified in PTSD patients with Met carriers (Figure 2A and Supplementary Table 2 in the online-only Data Supplement).
As for the HCs group, the positive relationship between childhood physical abuse and suicidal ideation was significant in HCs with Val/Val genotype at all levels (i.e., low, average, high) of social support (B=0.948, t=3.929, p<0.001; B=0.751, t=3.433, p=0.001; B=0.553, t=2.376, p=0.020). This relationship was also significant in the HCs with Met carriers at one SD below (i.e., lower social support) the mean social support and at average (B=0.498, t=4.114, p<0.001; B=0.301, t=2.341, p=0.022) (Figure 2B and Supplementary Table 2 in the online-only Data Supplement).
DISCUSSION
This study investigated the effects of childhood physical abuse on suicidal ideation regarding BDNF polymorphism and social support as risk and protective factors in patients with PTSD and the HCs. Our results demonstrated the significant moderation effect of BDNF Val66Met in the relationship between childhood physical abuse and suicidal ideation in patients with PTSD. More specifically, PTSD patients with BDNF Val/Val genotype showed significant increases in suicidal ideation when they were exposed to more severe childhood physical abuse. In the HCs, the moderation effect of social support was significant in the relationship between childhood physical abuse and suicidal ideation. More specifically, the HCs with low social support showed significant increases in suicidal ideation when they were exposed to more severe childhood physical abuse.
First, there was a significant moderation effect of BDNF Val66Met on the relationship between childhood physical abuse and suicidal ideation in patients with PTSD. Our results implicate that the patients with PTSD may have a genetic vulnerability to suicidal ideation, regarding the BDNF polymorphism [14,21,23]. There have been several studies on the relationship between BDNF polymorphism and suicide in patients with various psychiatric disorders, which have indicated genetic risk factors for suicidal ideation [12,50-52]. Our study also confirmed that the BDNF polymorphism could be a strong candidate gene related to suicide in Korean patients with PTSD.
More specifically, PTSD patients with BDNF Val/Val genotype showed significant increases in suicidal ideation when they were exposed to more severe physical abuse during childhood. In contrast, PTSD patients with BDNF Met carriers genotype did not show any association between childhood physical abuse and suicidal ideation. These results indicated that BDNF Val/Val genotype could act as a risk factor for suicide in patients with PTSD, which is consistent with other studies [27,52]. It suggests that PTSD patients with Val/Val genotype could be vulnerable and likely to display suicidal behavior. However, previous studies showed mixed results regarding which genotype acts as the risk factor. Some studies indicated that the Met allele is risky [20,22,53], while others proposed the Val/Val genotype to be risky [24]. These inconsistent results could be explained by a genetic-ethnic dependency [54]. Specifically, several studies have reported that the Val/Val genotype was associated with suicidal behavior among Asians [43]. Additionally, different allele frequencies were found between Europeans and Asians [44]. For example, the Met allele frequency of the Korean participants was relatively higher than other races [55]. The allele frequency in our study (PTSD, 67.5%; HCs, 69.1%) was like previous studies conducted on Korean participants (63.64%– 71.64%) [56].
Second, the moderation effect of social support was significant in the relationship between childhood physical abuse and suicidal ideation in the HCs. Social support has been known as an important protective factor that prevents suicide in the Korean HCs [57-59]. Furthermore, social support has a significant effect on subsequent adaptation in adulthood who experienced physical and sexual abuse in childhood [60]. For example, individuals with childhood trauma tend to achieve good relationships, stable jobs, and healthy personalities in adulthood when they are provided with continual support [61].
However, the HCs with lower social support showed a significant increase in suicidal ideation when they were exposed to more severe childhood physical abuse. This result suggests that the impact of childhood physical abuse on suicidal behavior was not mitigated by social support when it is low in the HCs. A previous study showed that individuals with low perceived social support were more likely to feel depressed and believed they could not solve their personal problems [62]. Given these different characteristics of quantitative and qualitative social support, it is important to consider both aspects of social support [63] to prevent the suicide of individuals who were physically abused in childhood.
Lastly, the moderation effect of social support in the relationship between childhood physical abuse and suicidal ideation was not significant in patients with PTSD. It was also consistent with a previous finding that the mitigating effects of social support may decrease in PTSD patients with a severe level of childhood abuse [33]. These results could be explained by several reasons. First, victims of physical abuse and survivors of trauma may receive less actual or perceived social support [64,65], possibly because the traumatic experience overloads their social supporting networks, hindering the availability of social support [33]. Second, some types of social support may bring negative consequences including intentional or unintentional blame on or disbelief of the victim [66]. Given these, within patients with PTSD, situational factors may impact the mitigating effect of social support, suggesting the involvement of other predispositions as risk or protective factors for PTSD.
There are some limitations to this study. First, the sample size was relatively small for an association study. Therefore, replication studies with a larger sample size would be necessary to re-examine the current results. Second, it is difficult to confirm the strong causality between the variables in the current cross-sectional study. Additional longitudinal studies would be helpful to support the findings from this study.
In conclusion, our study was one of the few studies that examined the gene and environment interaction on suicidal ideation in patients with PTSD and HCs. Our results suggested that patients with PTSD showed a genetic predisposition, such as the BDNF polymorphism, to suicidal ideation. This vulnerability to suicide could be increased in the Val/Val genotype of BDNF Val66Met among patients with PTSD. Moreover, social support seems to act as a protective factor against suicide, especially in the HCs. This mitigating effect of social support was determined by the level of perceived social support. Our study indicated that the suicidality of PTSD patients seems to be more influenced by genetic risk factors rather than environmental protective factors.
Supplementary Materials
The online-only Data Supplement is available with this article at https://doi.org/10.30773/pi.2022.0189.
Mediation analysis examining effects of BDNF Val66Met polymorphism and social support on the relationship between childhood physical abuse and suicidal ideation
Simple slope analysis for proving interaction effects
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Seung-Hwan Lee, Chaeyeon Yang. Data curation: Aeran Kwon, Chaeyeon Yang. Formal analysis: Aeran Kwon, Chaeyeon Yang. Fund acquisition: Seung-Hwan Lee. Investigation: Aeran Kwon, Hyun Seo Lee, Chaeyeon Yang, Bori Jung. Methdology: Aeran Kwon, Bori Jung, Chaeyeon Yang. Project administration: Seung-Hwan Lee. Resources: Seung-Hwan Lee. Software: Aeran Kwon, Chaeyeon Yang. Supervision: Seung-Hwan Lee. Hyang Sook Kim. Validation: all authors. Visualization: Chaeyeon Yang, Aeran Kwon. Writing—original draft: Chaeyeon Yang, Aeran Kwon, Bori Jung. Writing—review & editing: Chaeyeon Yang, Seung-Hwan Lee, Hyang Sook Kim, Hyun Seo Lee.
Funding Statement
This work was supported by the Brain Research Program through the National Research Foundation of Korea from the Ministry of Science, ICT & Future Planning (NRF-2015M3C7A1028252) and the Korea Medical Device Development Fund grant funded by the Korean government (the Ministry of Science and ICT, the Ministry of Trade, Industry and Energy, the Ministry of Health & Welfare, Republic of Korea, the Ministry of Food and Drug Safety) (1711138348, KMDF_PR_20200901_0169).