Examining the Psychometric Properties and Clinical Correlates of the Korean Version of the Family Accommodation Scale-Self-Rated Version for Obsessive-Compulsive Disorder
Article information
Abstract
Objective
We aimed to develop a Korean version of the Family Accommodation Scale-Self-Rated (FAS-SR), to investigate its reliability and validity and to study the clinical correlates of family accommodation in families with obsessive compulsive disorder (OCD) patient.
Methods
The FAS-SR was translated into Korean under the original author’s supervision. Forty-two patients with OCD and their closest relatives participated. The internal consistency was estimated using Cronbach’s alpha and the split half method. Convergent and divergent validity were identified by measuring with other clinical variables. Test-retest reliability was also calculated.
Results
The reliability analyses showed that Korean version of the FAS-SR demonstrated excellent internal consistency (Cronbach’s alpha=0.91) and test-retest reliability (Intraclass correlation coefficient=0.93). It showed good convergent validity when simultaneously assessed OCD symptom severity, global functioning and relative’s psychological distress.
Conclusion
The findings suggest that Korean version of the FAS-SR is a reliable and valid tool for assessing family accommodation in Korean patients with OCD in both research and clinical settings.
INTRODUCTION
Obsessive-compulsive disorder (OCD) is a chronic disorder characterized by unwanted repetitive thoughts (obsessions) and/or behaviors (compulsion) [1], affecting approximately 1%–3% of the adult population [2,3]. Obsessive-compulsive symptoms are highly distressing and hard to ignore, worsening the quality of life of patients [4-6]. OCD patients experience significant interference in various aspects of their lives, including social, occupational impairment [7,8]. Families of OCD patients also experience higher distress, compared with families with other psychiatric illnesses patients, since OCD symptoms are often related to or dependent on family members [9,10].
Family accommodation (FA) refers to a phenomenon in which family members adjust their lifestyle according to the patient’s obsessive-compulsive symptoms. In particular, family members often participate in the patients’ rituals or modify their routines to avoid triggering the patients’ symptoms [11]. FA is highly prevalent in families of patients with OCD, with up to 97% of family members reporting that they accommodate symptoms in a significant way [12,13]. Although, it may temporarily relieve a patient’s anxiety, paradoxically, it contributes to destroying the family’s quality of life [14] and reducing the effectiveness of the patient’s treatment by preventing them from exposure to obsession [13,15].
Growing body of researches focus on clinical correlates with family accommodation. For example, higher symptom severity, lower general functioning and specific OCD symptom dimensions (such as cleaning and comorbid mood symptoms) were associated with higher family accommodation [16-19]. Regarding relatives’ factors, higher family conflict, familial aggression, and feelings of anger and anxiety demonstrate higher family accommodation [19]. However, most of researches have been carried out in American and Western-European societies, and there has been a lack of cross-cultural studies examining family accommodation in OCD family.
The interviewer-rated Family Accommodation Scale for Obsessive-compulsive Disorder (FAS-IR), an instrument that assesses 12 accommodating behaviors, has been considered the gold standard for assessing the types and severity of FA [11]. However, FAS-IR has some disadvantage using in clinical practice because significant time spent in interviewer training/administrating. Further, it may miss some accommodating behaviors, as family members may feel less willing to disclose the patient’s OCD symptoms when asked directly by a clinician [20]. The self-rated version of the Family Accommodation Scale for Obsessive-compulsive Disorder (FAS-SR) is a modified version of the FAS-IR to compensate for the latter’s shortcomings by Pinto et al. [16]. The FAS-SR is a self-report measure assessing accommodating behaviors in the past week, completed by the relatives of patients with OCD. The FAS-SR has already been translated in Japan and India and demonstrated excellent internal consistency and good convergent validity with related constructs (e.g., OCD symptom severity, overall psychosocial functioning, family functioning, and distress experienced by patients’ relatives) [21,22]. Thus, the FAS-SR can be considered a practical alternative to the FAS-IR and has sufficient potential to be widely applied [13].
Patterns of caregiving and beliefs about disease vary widely across cultures and could lead to substantially different responses to patients’ obsessive-compulsive symptoms [23]. In Korea, to the best of authors’ knowledge, there exists no tools assessing FA in OCD family. Therefore, this study aimed to standardize the Korean version of the FAS-SR and explore the characteristics of family accommodation behavior in Korea.
METHODS
Development of the Korean version of the FAS-SR
With the original author’s permission, the FAS-SR was translated into Korean this paper’s first author. Back-translation into English was performed by a bilingual translator with a medical background who was familiar with the original FAS-SR. The back-translated version was sent to Dr. Calvocoressi, one of the developers of the original FAS-SR. The first author then revised the Korean translation according to the feedback received. After repeating this procedure, the equivalence of the original version and Korean version of the FAS-SR was confirmed.
Participants and procedures
All participants and their relatives gave their informed written consent after the study procedure was fully described to them. This study was approved by the Severance Clinical Review Committee (2017-3250-001). We enrolled OCD patients who could read and respond to the questionnaires, as well as understand the explanations of the researcher or assistant researcher. Participants were individuals aged over 19 years who met the DSM-5 criteria for OCD. They were recruited from the Severance Hospital between May 2018 and January 2021. We defined relatives as individuals who routinely lived with patients and/or had substantial contact with them. Participating relatives were those who reported that they were most intimately involved in caring for the patient with OCD. The study participants included 42 outpatients and 42 relatives. We asked 12 relatives to complete the FAS-SR again within 1 month after we received all questionnaires.
Measures administered only to patients
The Global Assessment of Functioning Scale (GAF)
The Global Assessment of Functioning Scale (GAF) is a single interviewer’s assessment, scored from 1 to 100, that is used to examine the overall severity of psychopathology and dysfunction in the worst week of the past month. Higher scores indicating better overall adjustment and higher functionality.
Measures administered only to relatives
Korean version of the Family Accommodation Scale for OCD-Self-Rated
The FAS-SR is a 19-item self-rated questionnaire that measures the level of family accommodation in response to obsessive-compulsive symptoms. According to the first section of the original FAS-SR, relatives were initially asked to identify the patient’s current OCD symptoms based on a modified Yale-Brown Obsessive-Compulsive Scale (Y-BOCS-SC) symptom checklist. In the second section, relatives were asked to assess the frequency of 19 accommodation behaviors using a 5-point Likert scale ranging from 0 (never) to 4 (every day). The original version of the FAS-SR has excellent internal consistency (Cronbach’s alpha=0.90) as well as good convergent and discriminant validity [13].
Family Assessment Device (FAD) [24]
The Family Assessment Device (FAD) is a self-reported list of 60 items for assessing family functioning using a 4-point Likert scale ranging from 1 (strongly agree) to 4 (strongly disagree). Based on the McMaster Model of Family Functioning, the FAD measures six dimensions: affective involvement, affective responsiveness, behavioral control, communication, problem-solving, and role. The FAD also measures general family functioning. We used the validated Korean version of the FAD to examine the convergent validity of Korean version of the FAS-SR [25]. Of the original 60 questions, 51 were used in this study, excluding nine questions with low correlation. A higher score indicates more effective family functioning. The Cronbach’s alpha of the Korean version of the FAD was between 0.74 and 0.92 for each subdimension at the time of the tool development; in this study, its reliability ranged from 0.77 to 0.84.
Measures administered to both patients and relatives
The Yale-Brown Obsessive-Compulsive Scale (Y-BOCS) [26]
The Yale-Brown Obsessive-Compulsive Scale (Y-BOCS) assesses the severity of OCD symptoms through semi-structured interviews. It consists of two parts: the Y-BOCS symptom checklist (Y-BOCS-SC) and the Y-BOCS symptom severity scale (Y-BOCS-SS). The Y-BOCS-SS consists of 10 items that assess the severity of obsessions and compulsions using a 5-point Likert scale ranging from 0 (no symptoms) to 4 (extremely severe symptoms), resulting in a total score ranging from 0 to 40. Within the total Y-BOCS score range of severity, 0–7 is considered “asymptomatic,” 8–15 “mild,” 16–23 “moderate,” 24–31 “severe,” and 32–40 “extreme.” We used the validated Korean self-report version of the Y-BOCS-SS [27] to assess the severity of patients’ compulsion symptoms. The alphas for the Korean self-report version ranged from 0.69 to 0.91. In the relative assessment, we used five items regarding compulsions from the Y-BOCS-SS to examine the convergent validity of the Korean version of the FAS-SR.
Kessler Psychological Distress Scale (K6) [28]
The Kessler Psychological Distress Scale (K6) is a 5-item self-report screening scale for psychological distress using a 5-point Likert scale ranging from 1 (not at all) to 5 (always). A higher score indicates lower psychological distress. We used the validated Korean version of the K6 [29] The reliability coefficient was 0.91, indicating excellent internal consistency.
Barratt Impulsivity Scale II (BIS II) [30]
The Barratt Impulsivity Scale II (BIS II) is a 30-item self-report inventory that assesses the personality/behavioral construct of impulsiveness using a 4-point Likert scale ranging from 1 (never) to 4 (always). We used the validated Korean version of the BIS II to examine the divergent validity of the Korean version of the FAS-SR. Its Cronbach’s alpha of 0.90 indicated it had good internal consistency [31].
Analysis
Descriptive statistics were obtained for clinical and socio-demographic variables. Cronbach’s alpha was used to estimate the internal consistency of the Korean version of the FAS-SR. The Spearman-Brown coefficient and the Guttman split-half coefficient were used to assess the instrument’s split-half reliability. For test-retest reliability, the intra-class correlation coefficient (ICC) was calculated. The correlation coefficient between the FAS-SR and both patient and relative-rated Y-BOCS, FAD, and patient-rated GAF were calculated to identify the convergent and divergent validity. Correlations above 0.8, between 0.6 and 0.8, between 0.4 and 0.6, between 0.2 and 0.4, and below 0.2 were considered very strong, strong, moderate, weak, and very weak, respectively. All statistical analyses were performed using SPSS version 23 software (IBM Corp., Armonk, NY, USA).
RESULTS
Sample characteristics
The demographic profiles of the OCD patients and their relatives are shown in Table 1. A total of 42 OCD patients and their 42 relatives were included in this study. The mean Y-BOCS total score was 21.17 (SD=7.46), indicating moderate OCD symptom severity. Patients of varying symptom severity participated relatively evenly in this study (13 mild cases, 14 moderate cases, and 15 severe to extreme cases). 78% (n=33) of the participating relatives were related to patients as parents.
Regarding the obsession symptom category in the FAS-SR, contamination (50.00%) was the most common, followed by religious (42.85%) and hoarding symptoms (35.71%); in the compulsion symptom category, cleaning/washing (54.76%) was the most prevalent, followed by repeating (42.85%), miscellaneous (42.85%), and checking (35.71%).
Frequency of each type of family accommodation
The frequency data for the Korean version of the FAS-SR are presented in Table 2. The most frequently reported accommodation items were Item 13 (“I did not do anything that could trigger the patient’s obsessive thoughts or compulsive behavior”) (79.0%), item 15, I didn’t do anything to stop unusual OCD-related behaviors by my relative. The least common form of accommodation was “When the patient was absent from work or socially unable to live due to obsessive-compulsive symptoms, I made up excuses or lied for him/her” (27.9%), “I put off my household chores because of the patient’s obsessive-compulsive symptoms” (37.2%).
Reliability
The item-total correlations are presented in Table 2. The overall Cronbach’s alpha of the Korean version of the FAS-SR was 0.91, indicating good internal consistency. The Spearman-Brown coefficient was 0.84, and Guttmann’s split-half coefficient was 0.83 indicating acceptable spilt-half reliability. The test-retest correlation coefficient was 0.93 (p<0.01), indicating that the ICC for each of the 19 items of the Korean version of the FAS-SR was good.
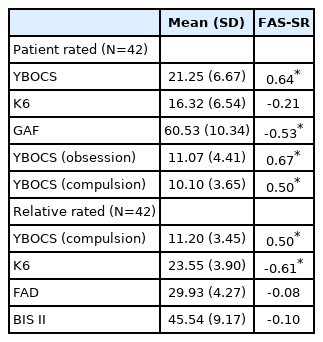
Convergent/divergent validity
Table 3 shows the convergent and divergent validity of the Korean version of the FAS-SR. For convergent validity, the FAS-SR was moderately correlated with the symptom severity (Y-BOCS, r=0.64, p<0.05), patient’s general function (GAF, r=0.64, p<0.05), relative’s distress (K6, r=-0.61, p<0.05). For divergent validity, the FAS-SR was not correlated with the BIS II.
DISCUSSION
We translated the FAS-SR, a representative scale for assessing family accommodation in obsessive-compulsive disorder, into Korean and examined its psychometric properties. The Korean version of FAS-SR showed excellent reliability and acceptable validity and it can be easily completed by relatives at the outpatient clinic setting. As far as our knowledge, this is the first study investigates both OCD patient and their family members from a family accommodation aspect.
Regarding reliability, Korean version of the FAS-SR showed excellent internal consistency (Chronbach’s alpha=0.91). The original version (Chronbach’s alpha=0.90) and the Hindi version (Chronbach’s alpha=0.93) [22] were similar to ours, whereas the Japanese version was lower (0.88) [21]. Further, the Korean version’s Spearman-Brown coefficient was higher than Hindi versions (Spearman-Brown coefficient=0.75, Guttmann’s split-half coefficient=0.71) [22] indicating that the split-half reliability of Korean version of the FAS-SR was acceptable. The ICC for each of the 19 items of the scale was higher than that of the Japanese version (ICC=0.85, p<0.01). Above results support that Korean version of the FAS-SR constitute a reliable measure for consistent symptoms.
The Korean version of FAS-SR was significantly correlated with clinical factors previously known to be related to FA, such as with relative-rated psychological distress, patients rated OC symptom severity and general functioning, indicates good convergent validity. However, contrary to our expectation, there was no correlation between the Korean version of FAS and the relative-rated FAD. Validation studies in Japan and India, the FAS-SR was significantly associated with relative-rated family function [16,21,22]. This discrepancy might come from that the composition of the relatives participating at the study varies among studies. In our study, the proportion of parents among relatives was 79.06%, which is higher than that of the Japan (48.8%) [21], India (31.7%) [22], and United states (37%) [16]. Parents tend to rate their families as more healthy than other family members with FAD.
The most common types of family accommodation in our study were item 13 (“I stopped doing things that could trigger the patient’s OCD” [80.9%]); and item 15 (“I avoided talking about OCD triggers” [78.6%]). For a Japanese study, 21 the most common type of family accommodation was item 12 (“I avoided talking about OCD triggers” [63.4%]), whereas in the original study it was item 1 (“I reassured patient that there were no grounds for OCD concern” [63.4%]). These results demonstrate that in east Asia countries, the relatives of OCD patients usually modified their behavior or routine; by contrast, in the American study, they usually provided reassurance and participated in patients’ compulsions. When implementing family-based Exposure and Response Prevention (ERP) in Korean OCD patients, reducing the tendency of relatives to modify their behavior to avoid symptom triggering might help to achieve good therapeutic effects.
A limitation of the present study is its relatively small sample size (78.57% of relatives were parents), which may limit the power of the statistical analyses and the generalizability of the results. Second, potential for sample bias should be considered, as some of the patients were under-control with treatment, whereas others were acutely ill states. Third, FAS-IR, the gold standard, was not used to confirm convergent validity. Therefore, the clinical utility of the Korean version of the FAS-SR should be further evaluated in more strictly standardized settings and assessment tool.
The results of this study are meaningful because we introduced a tool to assess family accommodation in OCD patients in Korea for the first time. The Korean version of the FAS-SR is useful as a time-efficient and cost-effective tool.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Conflicts of Interest
Chan-Hyung Kim, a contributing editor of the Psychiatry Investigation, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Author Contributions
Conceptualization: Chan-Hyung Kim, Se Joo Kim. Data curation: Jhin Goo Chang. Formal analysis: Jhin Goo Chang. Investigation: all authors. Methodology: all authors. Supervision: Chan-Hyung Kim. Validation: Hye Min Lee. Visualization: Hye Min Lee. Writing—original draft: Jhin Goo Chang. Writing—review & editing: all authors.
Funding Statement
None