A New Acute-At-Home Child and Adolescent Clinical Service: Evaluation of Impact
Article information
Abstract
Objective
An Acute at Home (AAH) clinical service was implemented to reduce emergency and inpatient admissions to the regional tertiary child and adolescent mental health system. This paper examines describes the served the population and impact on emergency and inpatient admissions.
Methods
Analysis of re-admission rates for those enrolled before and after the May 2019 implementation of the AAH service in comparison over the same time period to an unexposed comparison group. In addition the groups were compared on clinical and demographic variables comparing those exposed and those not exposed to the AAH service.
Results
The results indicated that the AAH group experienced reduced rates of readmission and lengths of stay post-exposure. Family composition, sex, seven Adverse Childhood Experience survey items, and nine Western Canada Waitlist Child Mental Health Priority Criteria Score items distinguished those exposed to AAH compared to those who were not. Thirteen of 19 independent variables indicated greater pathology in the AAH group with less likelihood of potential of danger to self.
Conclusion
The present results indicate a substantial benefit of the AAH service via reducing readmissions and lengths of stay. The quantitative measures warrant a careful qualitative examination of the AAH processes along with ongoing monitoring of the program’s effect.
INTRODUCTION
Objective
This paper examines the impact of a new Acute at Home (AAH) clinical service in terms of its effect on on emergency and inpatient admissions.
Background
Inpatient admission for the treatment of acute mental disorder among children and youth has been a long-standing standard of psychiatric care and it comes with a social cost [1-3]. With the rising cost of healthcare and the recognition that separation from home and family life is not necessarily optimal in respect to stabilization and recovery. Further, there has always been some level of social discomfort and stigma [4,5] associated with hospitalizing children for mental disorders [6], hence providing at home service is a step closer to a more recovery-focused treatment and support. At home care to some extent circumvents the transitional difficulties of navigating both admission and discharge from an inpatient unit [7] aligning with aspects of family preservation in relation to child and youth crisis and optimal development [8].
In response, a number of models have been proposed and examined as alternatives to removing children and youth from their home environment in response to the presentation of acute mental disorder serious enough to warrant inpatient admission. However, objective evidence supporting any particular model as an alternative to inpatient admission remains sparse. Where studied, the evidence is promising, especially in respect to per-admission cost reductions [9,10]. For example, a German study of a supported discharge service offering an early discharge followed by 12 weeks of intensive support at home found that the service was both clinically effective and economical [10]. Nevertheless, as with inpatient treatment, at home care comes with its own unique set of considerations [11].
Setting and AAH Model
The Child and Adolescent Addiction and Mental Health and Psychiatry Program (CAAMHPP) in the Alberta Health Services’ Calgary health zone consists of a regionally distributed network of hospital and community-based scheduled, urgent, emergency, and inpatient services. Recently, CAAMHPP implemented an acute at home service (AAH) as an alternative to inpatient admission. The model differs somewhat from other at-home models in that it is an a priori alternative to inpatient admission on presentation to emergency services, rather than a step-down or post-inpatient intervention.
One advantage of the CAAMPP regional system of care is its embedded system of clinical measurement [12-15]. On this basis, it is possible to compare innovations in service delivery at a system level to established standards of care in terms of patients’ clinical profiles and outcomes. In this paper we examined the impact of the AAH service on admission and readmission rates in comparison to emergency and inpatient admissions not enrolled to AAH under the main hypothesis that the admission and readmission rates and lengths of stay for those exposed to AAH will improve (reduce and shorten). Additionally, the clinical profiles of those admitted to AAH are at least equivalent to the comparison groups representing the current standards of care [14,15].
Acute at Home Program Description
The Acute at Home (AAH) program is an AHS and a local contracted agency partnership that commenced in November 2018 and was fully operational by May 31st 2019 after a period of development (staff hiring, training, etc.). The AAH program has been developed to meet an increasing demand for mental health services for children and youth and reliance on emergency services. Ideally, AAH provides an alternative to inpatient admission after crisis presentation to emergency services. This is accomplished by shifting the model of care from facility-based to home-based care. Home-based treatment, including support, crisis intervention, individual and family counselling, helps patients and families manage mental health concerns at home and within their home communities rather than in hospital based services. Additionally, some patients admitted to inpatient or day treatment settings who subsequently settle and express interest may be transferred to the AAH service.
The acute at home model supports patients with somewhat lower, more moderate safety concerns to reside at home, thus reducing emergency room visits with enhanced stabilization at home and transition to outpatient services. Safety assessments are a standard of care in emergency psychiatric screening. While served children and youth presenting to emergency services may require some aspects of acute care, generally rapid response and enhanced services, they do not always require twenty-four hour care in an acute care facility or a residential setting. The vision for the enhanced at home model is to assist patients and their families in the home environment with twelve hour per day coverage to support families in the initially presenting to the emergency department, with increased frequency of home visitation, or phone consultations, or both. The AAH clinicians are an integrated component of a larger interdisciplinary team that provides clinical, psychiatric, and case management support depending on the needs of the families served. The staffing model included nursing, family counselling, mental health and occupational therapy, administration, clinical supervision, case management, and outreach staffing.
Hypothesis
The analysis examines the hypothesis that the AAH service will reduce length of stay and re-admission rates. Additionally, the pre-post implementation clinical profiles of those exposed to the AAH service are compared to a similar unexposed group across comparable time periods.
METHODS
Data
Data for this paper was collected under ethics ID-REB15-1057. The regional access and intake system (RAIS) is the registration system containing all the registration, demographic, clinical profile and outcome information for the CAAMHPP system of care. De-identified information extracted from RAIS included patient clinical information gathered on admission and/or discharge, including the Western Canada Waitlist Child Mental Health Priority Criteria Score (WCWL-CMH-PCS), Adverse Childhood Experience (ACE) Survey, Measureable Treatment Plan (MTP), clinic disposition (emergent, urgent, scheduled), demographic, admission, and discharge dates between January 1st 2018 and December 31st 2020 [12,14-18].
Analysis
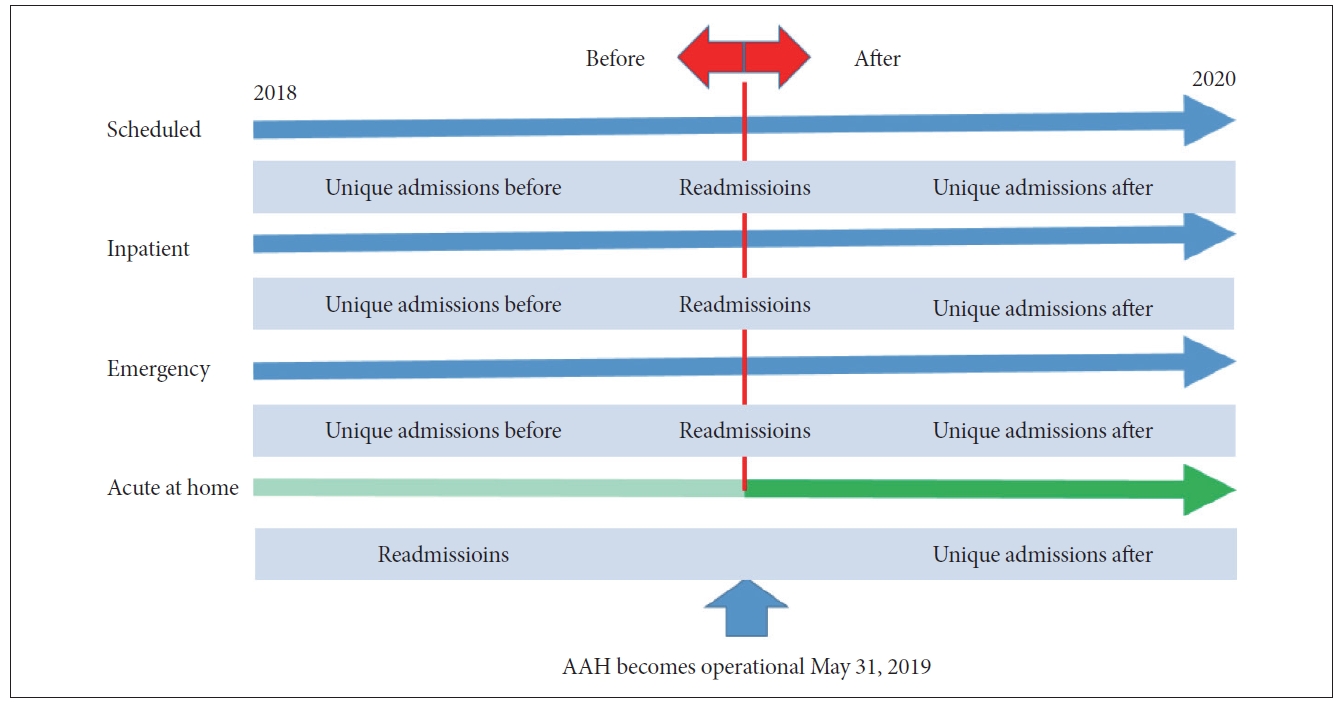
Two natural groups (dependent variable) formed on the basis of index presentation to emergency services (Figure 1): those exposed and unexposed to AAH. Table 1 provides unique individual and admission counts with age and sex. Within the unexposed groups there were three levels of service including emergency, inpatient, and scheduled services. Those exposed to AAH received service based on the AAH model of care, while those unexposed received the usual standard of care. Table 2 shows the reasons for referral for each dependent group.
Both groups on presentation to child mental health emergency services, depending on their presenting complaints, could be admitted to inpatient or scheduled services. Those exposed (admitted) to the novel AAH service could have had previous or subsequent admissions to the full range of service levels, or both. Those unexposed to AAH services who received the usual standard of care on presentation to emergency services could also have had previous admissions to the full range of service levels or admissions subsequent to their presentation to emergency services. For the unexposed group receiving the usual standard of care the date of AAH implementation provided a natural date to create a before and after group on which to base comparisons of the independent variables. The before interval was from January 1 2018 up to May 31st 2019 and the after interval was from June 1st 2019 until December 31st 2020. The AAH before and after group depended on the index admission to the AAH service and these dates would accumulate from the May 31st implementation date over the after interval. For comparison, those with previous admissions that spanned the before and after period were described separately from those who had only unique admissions in either the before or after intervals. An overall comparison of admission frequencies and lengths of stay of AAH exposed and unexposed groups is shown in Table 3 and a similar comparison on the basis of the specific levels of service is shown in Table 4. Non-overlapping 95% confidence intervals provide indication of statistical significance.

Details of length of stay before June 2019 and after May 2019 by service level for those readmitted and those not readmitted across the time interval
Figure 1 shows admission and re-admission distinction within and between the clinical service level and AAH groups on the basis of the before and after time interval. The frequencies and lengths of stay (days) of admissions and readmissions were described separately for each clinical services levels (Tables 3 and 4).
The results of two multinomial logistic regression analyses are shown in Tables 5 and 6.
RESULTS
Table 1 describes the sample, including number of unique individuals, number of registrations, sex and age by service type. Self-defined sex has the highest proportion of unique individuals presenting to emergency services. Older individuals present to inpatient, emergency and acute at home services. All referrals are referrals to emergency services and once presenting to emergency services are assessed and referred to and admitted acute at home services. Table 1 described the first admissions irrespective of time to each service group. Tables 3-5 below reflect service level (scheduled, inpatient and emergency) admissions and subsequent emergency services or acute at home services admissions. Hence, scheduled, inpatient and emergency admission for each service type follow a primary admission to either emergency services or acute at home services and includes the primary referral in each summation.
In Table 2 are shown the reasons for referral for each of the service groups. Note that the highest reason for referral for all groups is “Harmful behavior/thoughts of Self-Harm.” The proportion for acute at home (1.8%) is comparable to the unexposed referrals (1.8%) to emergency services and, as expected, less than those referred to inpatient services (unexposed 7.9%, AAH exposed 4.6%).
Table 3 described the overall reductions within each of the service groups. For within groups differences in length of stay, there was in the after interval a 16% reduction for Scheduled, a 44% reduction for Inpatient a reduction of 22% Emergency, and a 51% reduction in the length of stay for Acute at home services. Endpoints for Acute at Home compared to Scheduled were 63% lower, there was no difference for Inpatient services, and there was a 26% lower length of stay compared to Emergency services.
Table 4 shows the comparison within and between the service level groups for two levels of patients exposed and unexposed to Acute At Home services for those with readmissions and those with unique admissions in the equal time intervals before June 2019 and After May 2019. Note that all recorded admissions were first admitted to emergency or acute at home services before being admitted to the services shown in Table 4, respectively. Admissions to acute at home services (n=42) during the development period (November 1, 2019–May 31, 2019) were not included in the analysis.
While those with readmissions (upper Table 4) in the acute at home services have 16 additional admissions post implementation after May 2019 in the scheduled service, the magnitude in the reduction of length of stay is much greater than in the unexposed group (between group difference). Even though both the non-exposed group and acute at home services groups reduced 18% and 37% respectively in each of their endpoints before and after, the acute at home services group was 25% lower than the unexposed group at the endpoint in the after interval.
Patients admitted to the inpatient setting, whether or not they were first admitted to emergency service or admitted for assessment to the acute at home services were not different in either the readmission or the unique admission groups in the before or after time intervals.
Patients admitted to the emergency setting, whether or not they were first admitted to emergency service or admitted for assessment to the acute at home services were not different in the readmission group. However 33% fewer these patients were admitted to the emergency services in the unique admission groups in the after time interval in the non-exposed group and the magnitude of the value in the acute at home exposed group in the after interval was 17% lower than the endpoint of the non-exposed group.
Table 5 shows the comparison membership in each of the three non-AAH exposed groups to the AAH exposed group. The main highlights of the model is that it validates population served by the AAH exposed group in that inpatients have higher ACE scores and scheduled have lower ACE scores, with no difference from the emergency group. Lengths of stay are shorter with within the AAH exposed groups even though the other groups have few admissions.
Table 6 shows the relationship of the WCWL-CMH-PCS urgency score to each of the three non-AAH exposed groups to the AAH exposed group. The WCWL-CMH-PCS urgency score variable was analyzed separately due to its high correlation with the ACE total score. The regression analysis indicates that the Emergency and AAH groups have comparable WCWL-CMH-PCS values, indicating relative equivalency of these two groups that converge in the emergency department services, and like those that are admitted to inpatients (a step toward stabilization from the emergency department), both are greater than the scheduled group. Note that the WCWL-CMH-PCS form is not completed on every in-system transfer, rather it is generally completed on index referral or presentation from the community.
DISCUSSION
In summary, taken together, the results from Table 2 (proportions of self-harm in AAH equivalent to inpatient and emergency services), as well as Tables 5 and 6 (AAH similar to emergency services and different from scheduled services on key variables) provide support indicating that the AAH exposed group is closest in clinical profile to the emergency service group. Tables 3 and 4 show that exposure to AAH reduces the length of stay in the after interval in scheduled services readmissions (upper Table 4), unique scheduled services admissions (lower Table 4) and unique emergency services (lower Table 4) compared within the exposed groups compared between the nonexposed groups. Based on the similarity of the AAH exposed and unexposed groups, the findings indicate that the main hypothesis may be accepted and AAH reduced both readmission rates and lengths of stay. The clinical ‘space’ created in the system resulting from the observed reduction potentially becomes available to those who may be more clinically affected.
In respect to other studies of this AAH model of care, a number of systematic reviews of AAH service types have been completed [19-22] in addition to reviews of family perceptions and satisfaction with such services [23]. A general conclusion is that there is insufficient evidence on which to base decisions on which model is best for which group of young people [19]. This remains as the current state of affairs. For example, Sheppard et al. [20] identify in conclusion that studies require baseline measurement at admission along with demographic data, and outcomes measured using a few standardized robust instruments. The results of the present study appear to bridge the gaps Sheppard et al. [20] identified in the systematic review of the acute at-home services subject. For example, clinical and demographic measures employed in the present study illustrate the ability to distinguish AAH enrollees specifically, being that these patients are comparable to unexposed emergency services in terms of the proportion of referrals for the reason of self-harm (e.g., suicidality), even though they are equivalent or more severe on a number of independent clinical variables (more frequent presentations to emergency services, higher urgency scores comparable to non-exposed emergency referrals). One AAH effect appears to be the significant reduction of emergency admission length of stay and subsequent lengths of stay to scheduled services. The Acute at Home (AAH) clinical service was implemented to reduce the burden on the regional tertiary child and adolescent mental health system, especially emergency and inpatient services. Inpatient units tend to have the highest per diem costs estimated by regional business analytics to be at minimum about $2,000CDN. It may be that so few AAH admissions come from inpatients that an effect is not yet obvious. A limitation is that this analysis did not take into account the specific AAH referral sources. AAH does reduce length of stay of admissions to emergency and scheduled services, which also have per diem costs.
The present results of this program are most similar to those of a program in Switzerland [24]. While the Swiss program’s focus was different in that the at home service in this Swiss pilot study was to preserve housing and avoid hospitalization in those with severe mental illness who might otherwise have lost their housing, the endpoints were similar to the AAH clinical service, indicating that the at-home service model has potential to translate to other mental health populations.
In conclusion, the AAH service achieved its predicted outcome, being to reduce length of stay and readmission for those presenting to emergency services. The clinical profile description of the AAH-exposed and unexposed groups indicate that the AAH group, wherein observed reductions were observed, were similar to the unexposed group, providing some measure of validity to the main findings.
Future research
Having quantitative results is only a start to understand the AAH service model effect, but one start point currently called for by the literature. These results point to an effect but give little insight into the dynamics underpinning the clinical and relational processes underpinning the AAH service model, a limitation of the present study. While measurement is important, in order for an operational policy to be developed that might guide AAH model implementation, future study warrants careful qualitative examination of the clinical and relational processes involved in AAH that includes both staff and served families, a component of the multi-method approach to evaluating the AAH service that is currently underway.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are not publicly available as such disclosure was not part of the ehtics approval.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: all authors. Formal analysis: David Cawthorpe. Methodology: all authors. Supervision: Noorani Khalfan, Carol Coventry. Validation: Noorani Khalfan, David Cawthorpe. Project administration: Noorani Khalfan, Carol Coventry. Writing—original draft: all authors. Writing—review & editing: all authors.
Funding Statement
None