Mental Health and Related Factors of Adolescent Students During Coronavirus Disease 2019 (COVID-19) Pandemic
Article information
Abstract
Objective
Adolescents are at a special stage of physical and mental development, which is a susceptible period for mental disorders. Since the outbreak of coronavirus pneumonia in December 2019, long term stress may have negative effects on the mental health of the adolescents. In the context of the coronavirus disease 2019 (COVID-19), the study was designed to investigate the mental and psychological health of adolescents in China and its possible related factors.
Methods
A cross-sectional study design was adopted using a structured questionnaire which were distributed through the Internet to measure depression, anxiety, life events and stress related factors. Descriptive statistics and multiple regression analyses were conducted to process the data.
Results
The final sample comprised 795 adolescents. The total detection rate of depression was 76.48% and the total detection rate of anxiety was 33.08%. ANOVA showed that there were significant differences in depression scores in terms of gender, anxiety scores, history of mental disorders, COVID-19 knowledge reserve, family and social contradictions (p<0.05). And there were significant differences in anxiety scores in terms of gender, depression scores, mental health knowledge reserves, family and social contradictions (p<0.05). Multiple regression analysis showed that anxiety score, health status and COVID-19 knowledge reserve were positively associated with depression score (p<0.01), and history of psychosocial disorders was negatively associated with depression score (p<0.05); depression score, family and social contradictions were significantly positively correlated with anxiety score (p<0.01), and history of mental disorders was significantly negatively correlated with SDS score (p<0.01).
Conclusion
During the outbreak of COVID-19, adolescent students with better understanding of the pandemic, more complete knowledge of mental health, and better family and social relationship had less impact on their mental health. Therefore, to ensure a sound social support system, elaborate health instruction, and family communication and mutual understanding are conducive to alleviating the psychological stress caused by the epidemic, and it is positive for adolescent students to maintain a good mental health.
INTRODUCTION
Coronavirus disease 2019 (COVID-19) is a new infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which has swept through the globe quickly and indiscriminately. Due to the impact that brought by the pandemic, COVID-19 has affected the lives of adolescents through several ways, such as the fear of infection, uncertainty, and potential economic problems [1]. On January 27, 2020, in response to the outbreak of COVID-19, and to protect the life safety of teachers and students, the government of China requested citizens to stay home and reduce unnecessary social activity [2,3]. This may lead to the discouragement of adolescents’ development, deprive opportunities for stress regulation, and lead to social isolation [4].
To recognize the importance of the effects of the COVID-19 pandemic on adolescent mental health, one must first understand the pertinent developmental changes that occur during adolescence. Adolescents are in a particular stage of physical and mental development, which is the critical period for exploring and establishing their identity. During this period, their body, brain, cognition and the surrounding social environment will change, their self- consciousness will be enhanced, their internal conflict will increase, they will feel the curiosity of the opposite sex, they will be psychologically sensitivity, mindful of others’ views, emotionally fluctuated, vulnerable to their surrounding influences, and susceptible to mental disorders [5-7]. As adolescents strive to be independent of their parents and spend more time with their peers, instead of parents, friends gradually become the primary source of interaction and influence, and this means that negative peer interactions during this important developmental period can lead to poor self-concept, a low sense of worth, and subsequent increases in symptoms of anxiety and depression [8,9]. Thus, base on the above development characteristics, adolescents can expose to an increased risk of psychological problems during the COVID-19 pandemic.
Plenty of studies over the past decades have shown that major social event including COVID-19 pandemic exists a detrimental impact on the mental health of individuals [10-14]. Early in 2003, during severe acute respiratory syndrome (SARS) pandemic in China, a study focused on medical students reported that compared with national normal model, the detection rate of anxiety and depression of medical students increased significantly [13]. Another study focused on the impact of Hurricane Katrina on mental health status among United States (US) adults also found that the hurricane adversely impacted the mental health of residents in Katrina-affected states, and the impact was tended to be associated with age, gender, income, and physical health [14]. And the latest studies also consistently point to the detrimental impact on the mental health of COVID-19. During the early stage of the pandemic, a research included 1,210 adults found that more than half (53.8%) of the respondents rated the psychological impact as moderate-to-severe, and about one-third reported moderate-to-severe anxiety [15]. A meta-analysis focused on the mental health among clinical workers which included 13 studies reported that, almost a quarter exhibited elevated COVID-19 related symptoms of anxiety (23.2%) and depression (22.8%), and more than a third (38.9%) experienced problems with insomnia [16].
Due to the particularity of the period of physical and mental development of adolescents, the psychological stress caused by the long-term isolation at home during the pandemic and the differences between online teaching and conventional way may have negative effects on their mental health [17,18]. Yet compared with studies concentrated on adults, few studies have evaluated the impact of the pandemic on mental health in adolescents. A study reported that the increases in generalized anxiety associated with COVID-19, were found to be more pronounced in younger people (<35 years) compared to older age groups [19]. A study from India demonstrated a high prevalence of psychological distress in quarantined children and adolescents due to the COVID-19 pandemic, and these individuals have experienced helplessness (66.11%), worry (68.59%) and fear (61.98%) [20]. Meanwhile, it is reported in China that the children and adolescents aged 3–18 years presented symptoms of inattention, worry and irritability during this pandemic [21].
During the current COVID-19 pandemic, people are being affected in multifaceted ways, having their physical, psychological and emotional well-being compromised, along with social and economic problems [22]. Similarly, COVID-19 has an impact on the mental health of adolescents through multiple factors. During the COVID-19 pandemic, parental psychiatric status significantly influenced the mental health of adolescents [23-25], the relationship between family members is one of the most important factors, and there have been reports of a significant increase in domestic violence around the world [4,26-28], putting adolescents exposed to this environment at increased risk for mental health problems. At the same time, isolation measures may have more impact on the mental health of adolescents and their family environment than one might expect. A systematic review of the psychological impact of isolation during a pandemic noted PTSD symptoms in 28%–34% of isolated populations, and adolescents who experienced isolation had an average PTSD score four times compared to those who did not experience [29,30]. And another study found that older adolescents are anxious regarding cancellation of examinations, exchange programs and academic events [31]. Further, the increased use of internet and social media increased the adolescents’ vulnerability to the mental disorders and was associated with increased depression and anxiety [32].
The COVID-19 pandemic affects the adolescents through multiple perspectives, however, consider from another perspective that, in the face of a current crisis, if challenges can be mastered, successfully managing stress with trauma may help with adolescents’ psychological growth and be a protective factor in coping with future stress [33]. Nevertheless, most of the current research focuses on adults or groups with special diseases, while few of them concentrated on the adolescents. In order to fill this gap, the purpose of this study was to estimate the impact of COVID-19 pandemic on adolescents’ wellbeing, and explore the associations among environment, family, and the COVID-19 relative factors on adolescents’ mental health.
METHODS
Study population
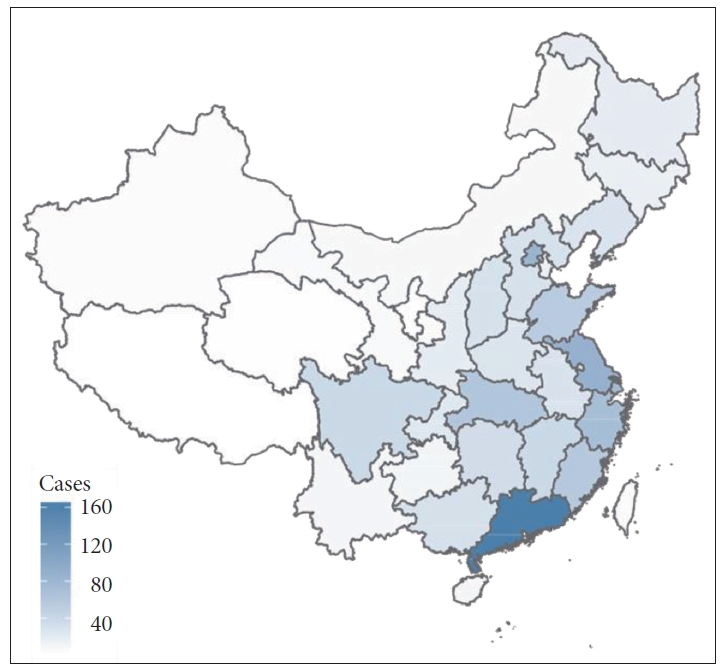
The study adopted a voluntary sampling method after obtaining the students’ informed consent. A structured questionnaire was conducted among 11–19 years old students in China during the period from March 19, 2020 to March 29, 2020 (Figure 1). The inclusion criteria were as follows: those who were 1) full-time student, 2) aged between 11 and 19, 3) willing to cooperate with the investigation, and obtained informed consent online. The exclusion criteria were as follows: those who refused to participate or cooperate (Figure 1).
Design and methods
A cross-sectional study design was adopted using a structured questionnaire to measure depression, anxiety, mental health knowledge, COVID-19 knowledge, and mental health related factors. The questionnaire was divided into 4 sections: 1) self-made general common questionnaire: including general demographic characteristics such as age, sex, school age, origin, health status, current living conditions, mental illness history (according to the participants), etc., and students fill in according to their own conditions; 2) Self-rating Depression Scale (SDS): the self-rating scale includes 20 items, divided into 4-grade rating, and the total score is 80. The standard score <50 is within the normal range, and ≥50 is defined as depression, 50–59 for mild depression, 60–69 for moderate depression, and 70 for severe depression;34,35 3) Self-rating Anxiety Scale (SAS): including 20 items which divides into 4-grade rating, and the total score is 80. The standard score <50 is within the normal range, and ≥50 is defined as anxiety, 50–59 for mild anxiety, 60–69 for moderate anxiety, and 70 for severe anxiety [36,37]; 4) self-made life event questionnaire: composed of 9 items, including the emotion-related factors, emotional impact of online courses, mental health-related knowledge (including understanding and coping with mental disorders, etc.), the understanding of COVID-19 (including the understanding of situation, measures, etc.), as well as the family and social contradictions, and the contradictory factors. Among those items, the emotion-related factors, emotional impact of online courses, family and social contradictory factors were designed as multiple-choice question (2–3 at most). Other items were designed as 5-grade rating question.
The calculation of the simple size was based on the estimation formula Z2
The questionnaires were distributed to major mainstream network platforms in China, such as WeChat, QQ and Microblog, etc. The technology was provided by the WJX platform (A professional online questionnaire survey, evaluation, voting platform). Backstage setting each IP address can only be filled once. Online informed consent was accessed in advance. For those whose response time was less than 120 seconds or more than 900 seconds were classified as invalid responses.
Statistical analysis
R project version 3.6.3 was used for data analysis in this study. Statistical significance was set at the 5% significance level. For demographic data, descriptive statistical analysis was used to summarize the statistical characteristics. Analysis of variance (ANOVA) was adopted to investigate the correlation between the total scores and the potential influencing factors (i.e., sex, age, grade, health status, mental disease history, mental health knowledge reserve, understanding of COVID-19, family and social contradiction). A multiple linear regression analysis was performed to analyze the relationships between the SAS scores and SDS scores and the potential influencing factors, which the dependent variables were SDS scores and SAS scores, and the independent variables were sex, age, grade, health status, mental disease history, mental health knowledge reserve, understanding of COVID-19, and family and social contradiction.
Ethics approval
The study was authorized by IRB of Dongfang Hospital Beijing University of Chinese Medicine (JDF-IRB-2019036101).
RESULTS
Demographic characteristics
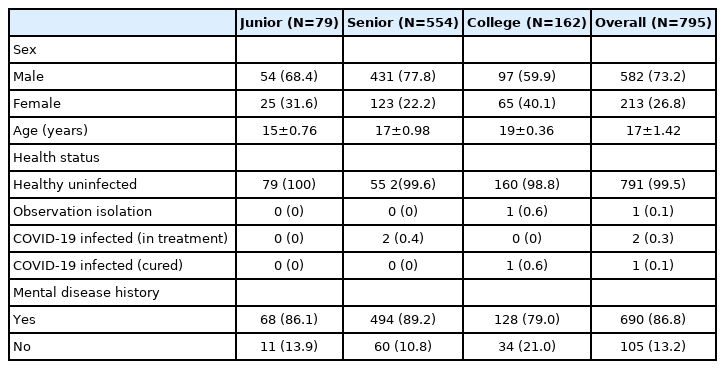
A total of 813 samples were collected from the study, 18 of which were excluded due to the answer time. Ultimately, 795 cases were included in the study, and the sample efficiency was 97.79%. As shown in Table 1, among the 795 participants at the age of 11–19 in China, 582 were male (73.2%), 213 were female (26.8%), with an average age of 17 (±1.42) years, and the oldest aged 19, the youngest aged 13. Seventy-nine were junior high school students, 554 (69.7%) were senior high school students, and 162 (20.4%) were college students. As of the time of investigation, 791 subjects (99.5%) were healthy uninfected, 1 subject (0.1%) was observed and quarantined, 2 subjects (0.3%) were confirmed COVID-19 and being treated, and 1 subject (0.1%) with COVID-19 was cured. Furthermore, 105 participants had a history of mental diseases such as anxiety and depression (13.2%) (Table 1).
Results of Depression Self Rating Scale (SDS)
As shown in Table 2, of 795 participants, 608 were found to be depressed, with a detection rate of 76.48%, of which 441 were mild (72.53%), 157 were moderate (25.82%) and 10 were severe (1.64%). The results of ANOVA showed that age, grade (education) and mental health knowledge reserve had no statistical difference on the SDS score (p>0.05); gender had a statistical difference on the SDS score (p<0.05); SAS scores, history of psychosocial diseases, the understanding of COVID-19, and family and social contradiction had significant statistical difference on SDS scores (p<0.01).
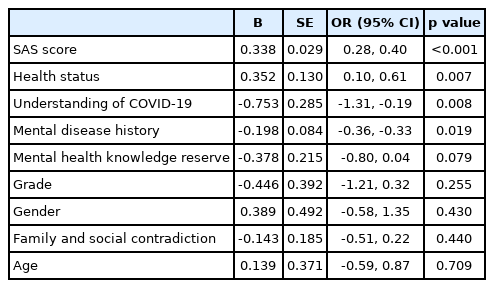
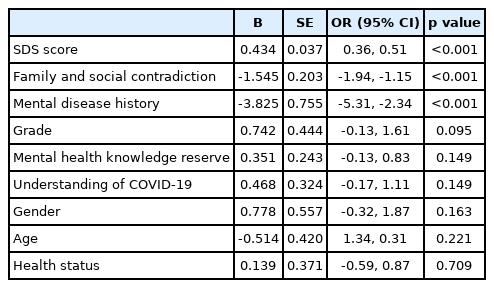
In the multiple linear regression analysis, the SDS scores of the participants were used as the dependent variable, and the independent variables included age, sex, grade, SAS score, health status, the understanding of COVID-19, mental disease history, mental health knowledge reserve, and family and social contradictions. The results of regression analysis are presented in Table 3, which revealed that SAS score, health status and the understanding of COVID-19 were significantly positively correlated with the SDS score (p<0.01), and the history of psychosocial disorders was negatively correlated with the SDS score (p<0.05).
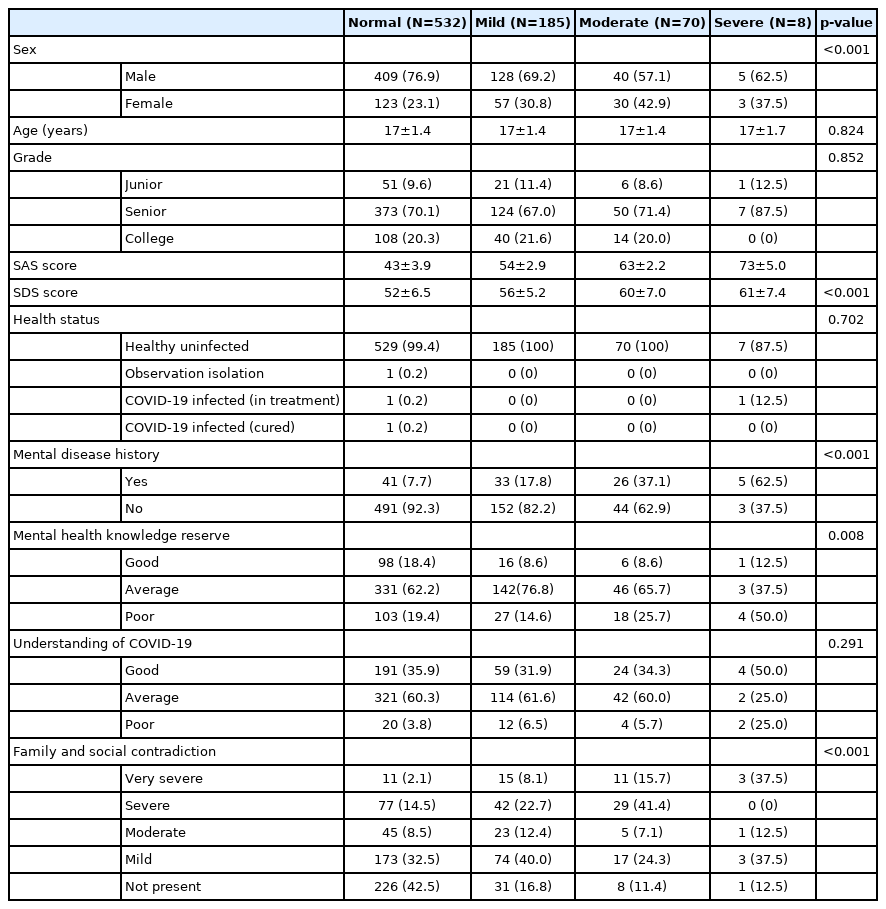
Results of Anxiety Self Rating Scale (SAS)
As shown in Table 4, the results of Self-rating Anxiety Scale showed that there were 263 participants with anxiety, and the detection rate was 33.08%. Among them, 185 were mild (70.34%), 70 were moderate (26.62%) and 8 were severe (3.04%). ANOVA results showed that age, grade (education), health status, and the understanding of COVID-19 had no statistical difference on the SAS score (p>0.05); gender, the SDS score, mental health knowledge reserve, and family and social contradiction had significant statistical differences on the SAS score (p<0.01).
The results of multiple linear regression analysis are presented in Table 5. The SAS Self-rating Anxiety Scale scores of the participants were taken as dependent variables, and the independent variables included age, sex, grade, the SDS score, health status, the understanding of COVID-19, history of mental disease, mental health knowledge reserve, and family and social contradiction. Regression analysis showed that the SDS score, and family and social contradiction were significantly positively correlated with the SAS score (p<0.01), and the history of mental disorders was significantly negatively correlated with the SDS score (p<0.01).
Results of self-made life event questionnaire
The study collected stress factors that may affect the psychological and emotional status of the participants during the epidemic. The main contents are as follows: 1) emotional changes during the pandemic; 2) the main causes of contradiction between family and friends; 3) the most worrying things at present; and 4) the influence of online teaching on oneself and its influencing factors. The results are as follows.
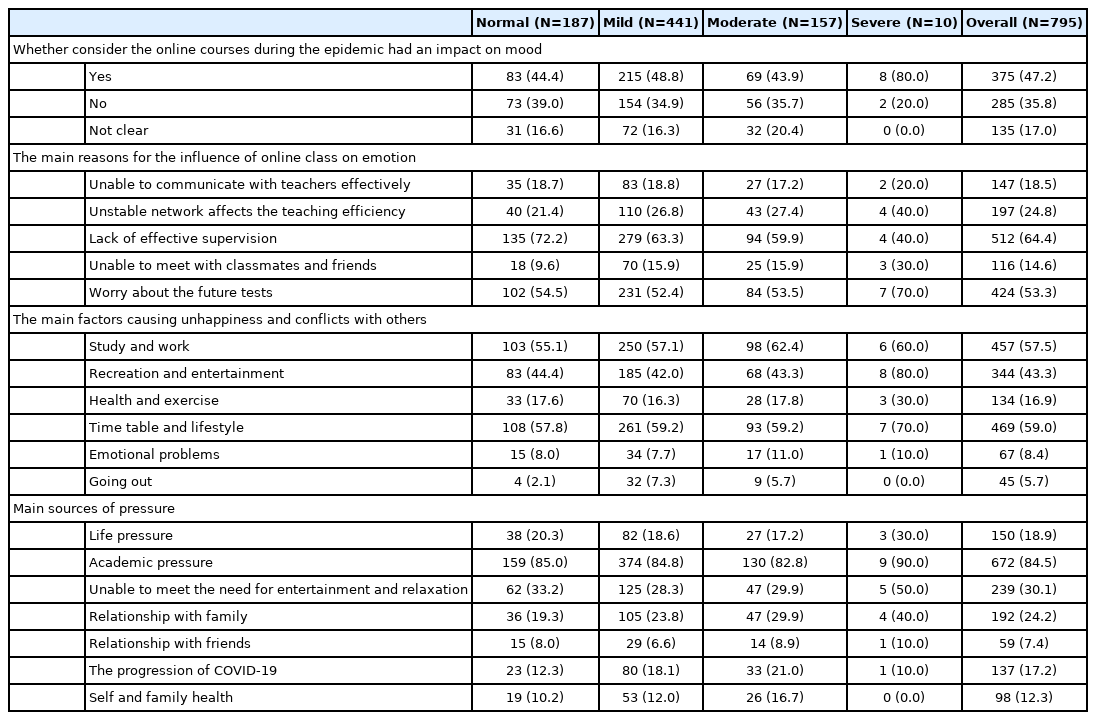
Regarding the emotional change, 3.77% of 795 participants felt that their emotions had changed significantly during the pandemic, 17.36% of the participants had changed moderately, 31.32% of the participants thought that the emotional change was mild, 30.31% of the participants felt that their emotions were unaffected, and 17.23% of the participants were not clear about their emotional changes. Meanwhile, 30.44% of the participants believed that their emotional changes might be related to the COVID-19 pandemic and related prevention measures, and 42.77% of the participants believed that they were not related to the above factors (Figure 2A).
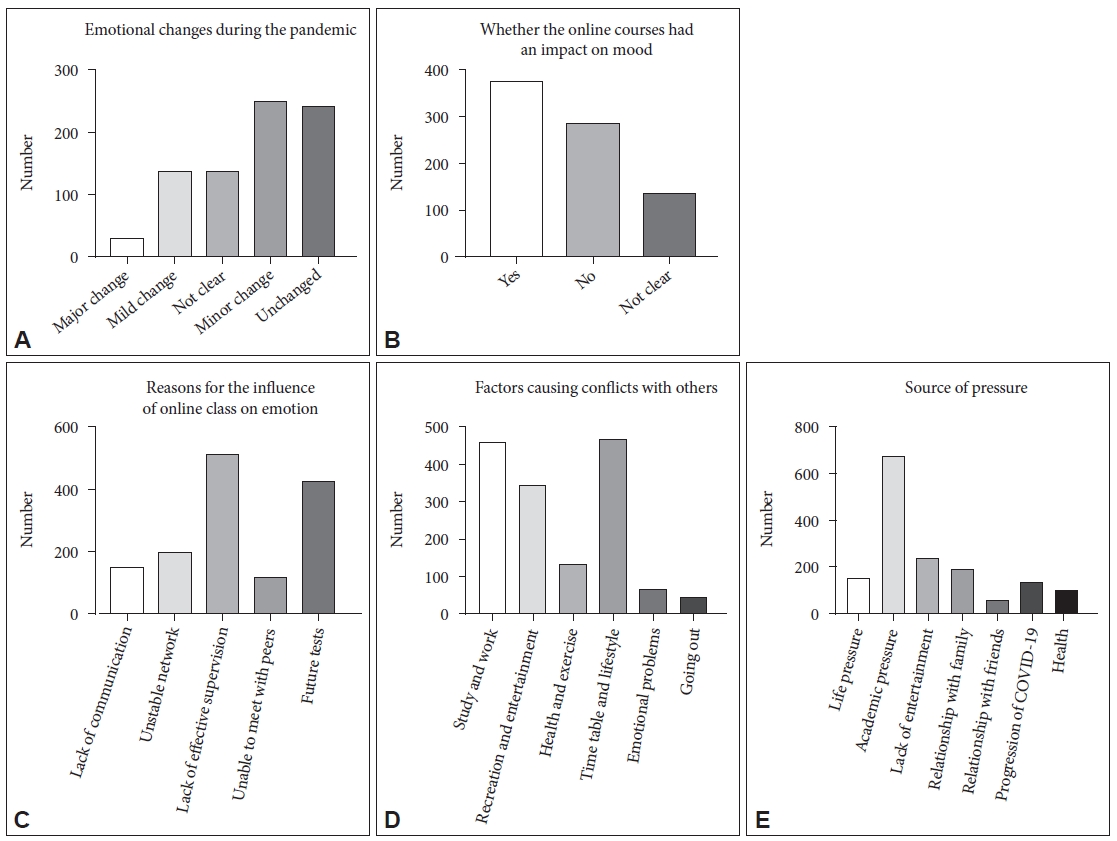
Results of self-made life event questionnaire Link text: A: The emotional changes during the pandemic. B: Whether the online courses had an impact on mood during the pandemic. C: The main reasons for the influence of online class on emotion. D: The main factors causing unhappiness and conflicts with others. E: Main sources of pressure.
As for the causes of the contradiction with family and friends (study, recreation, health, lifestyle, emotion, going out, others; multiple choice questions, and three choices at most), the three most common choices are lifestyle (58.99%), study (57.48%), and recreation (43.27%) (Figure 2D).
When talking about the most concerning things at present (life, academic, recreation, family, friends, the development of COVID-19, health, other, multiple choice question, up to three options), the top three were academic pressure (84.53%), inability to meet recreation needs (30.06%), and family relationships (24.15%) (Tables 6, 7, and Figure 2E).
Online courses are one of the greatest changes that the pandemic has brought to the participants daily life. As shown in Figure 2C, 47.17% of the participants considered that the change brought by online coursing has affected their daily mood, and 35.85% of the participants thought that online teaching has no impact on their mood. In the investigation of the reasons of online courses affecting emotions (unable to communicate with teachers efficiently, network instability, self-discipline, unable to see classmates, concern for the examinations, and others; multiple choice questions, and up to two options), the most common reasons are lack of supervision, poor self-discipline (64.4%) and concern for the future examinations (53.33%). Furthermore, we took the score of SAS and SDS as the dependent variable and the item option as the factor for ANOVA, the result showed that the different reasons for the influence of online class on emotion had a significant statistical difference on both SDS and SAS score (p<0.05) (Tables 6 and 7).
DISCUSSION
Since the outbreak of COVID-19, there has been persistent panic and psychological pressure. At the same time, due to the relevant national policies and the needs of pandemic prevention, the impact on the daily life of the student is much greater than that on the general population. Among them, the adolescent students who are in a special stage of physical and mental development are exposed to triple the stress of suspending classes, changes brought on by online teaching and the entrance examinations. In such an environment, the physical, mental, and behavioral health of the adolescent students has become the focus of attention of schools and colleges. In our study, we find that the pandemic had a practical impact on the adolescents’ mental health, both of the rate of anxiety and depression was higher than usual. The gender, living conditions, relationship with family and friends, mental disease history and knowledge of mental health and COVID-19 plays an important role in adolescent mental health during the epidemic. Besides, we find that, those adolescents who had a certain understanding of mental disorders and COVID-19 pandemic showed a lower rate of depression and anxiety. Furthermore, the life event questionnaire showed that online courses did have an impact on the adolescents’ emotion, mainly for the reason of lack of self-discipline. And the main sources of contradiction and pressure are closely related to study.
Of this study, the total detection rate of depression in adolescent students was 76.48%, 74.91% for males and 80.75% for females, including 441 mild (72.53%), 157 moderate (25.82%) and 10 severe (1.64%); the total detection rate of anxiety symptoms was 33.08%, 29.73% for males and 42.25% for females, including 185 mild (70.34%), 70 moderate (26.62%) and 8 severe (3.04%). Compared with a previous study on depression and anxiety among medical students during the COVID-19 pandemic with the detection rate of 35.53% and 15.41%, the detection rate of our study is relatively high [38]. Our results are similar to another study with the detection rate of 88.6%, which measured the impact of natural disasters on the psychological status of adolescents at school [40]. The differences with the former may mainly because of the immature states of physical and mental development of the adolescent students and the gap in the understanding of the pandemic situation between medical students and ordinary adolescent students. In addition, the adolescent students are also facing the pressures brought on by the entrance examinations, and during the pandemic, the school suspended classes and turned to teaching online, which has few precedents to follow. Therefore, the academic pressure brought on by the entrance examinations may have a more severe impact on the adolescent students’ mood than usual.
Our study found that there was a significant correlation between gender and the scores of anxiety and depression scales, and the detection rate of anxiety and depression in females was higher than that in males. Through the analysis of the entries of SDS and SAS, it can be discovered that most psychosocial symptoms (such as melancholy, crying, dread, panic, anxiety, irritability, and worthlessness) and somatic symptoms (such as insomnia, weight loss, astriction, palpitation, physical pain, and nightmare) are generally higher in women than in men. The prevailing consensus belief is that females are more vulnerable to environmental stressors than males [41], which is consistent with the conclusions of our study. In addition, we found that among the respondents with severe depression assessed by the SDS, symptoms were mostly concentrated in somatic disorders (temporality, abnormal appetite, weight loss, astriction, palpitation, and restless), while those with severe anxiety assessed by the SAS, symptoms were mostly concentrated in anxiety mood (anxiety, dread, madness, and nightmares) (Figures 3 and 4).

Heatmap of Symptom Distribution on SDS. Link text: In the compare of the entries of the SDS, most of psychosocial symptoms (such as melancholy, easy to cry, worthless) and somatic symptoms (such as sleep disorders, weight loss, astriction, palpitation, fatigue) are generally higher in Females than in males. In terms of decreased sexual interest, ability decline, difficulty thinking, despair, males scored higher than female. And among the respondents assessed as severe depression, symptoms were more likely to concentrated in somatic disorders (temporality, abnormal appetite, weight loss, astriction, palpitation, and restless). SDS, Selfrating Depression Scale.

Heatmap of Symptom Distribution on SAS. Link text: For the entries of the SAS, most of psychosocial symptoms (anxiety, dread, panic, madness) and somatic symptoms (physical pain, fatigue, palpitation, dizziness, syncope, numbness, stomachache or indigestion, flush, limbs shaking) are generally higher in Females than in males. In terms of akathisia, sweat, sleep disorders, presentiment, males scored higher than female. Among the respondents assessed as severe anxiety, symptoms were more likely to concentrated in anxiety mood (anxiety, dread, madness, and nightmares). SAS, Self-rating Anxiety Scale.
At the same time, we observed that family and social contradictions were both significantly correlated with anxiety and depression symptoms of adolescent students, and based on the results of regression analysis, they were significantly negatively correlated with SAS scores. A previous study on the related factors of anxiety and depression in adolescents with congenital dorsal vertebral insufficiency, the family environment was negatively correlated with the depression [42], which was consistent with the conclusion of our study, but the participants in this study had specific characteristics, and their family environment was also different from those respondents who were included in our study, so the bias may be exist compared with the reality. Adolescents are in the period of psychological development, and their antagonistic mentality has an important impact on their mental health. During this period of suspended education and home isolation, the adolescents’ individual freedom was restricted and threatened, which may lead to the aggravation of the antagonistic mentality, thus intensifying the family and social contradiction, and then having a greater negative impact on the mood, thus falling into a vicious circle [43-45].
According to the results of data analysis, it can be found that the knowledge of COVID-19 pandemic and mental health is closely related to the anxiety and depression symptoms of adolescents, and the more abundant the relevant knowledge reserve, the corresponding detection rate of anxiety and depression will also decrease. The results of multiple linear regression analysis proved that the knowledge reserve of COVID-19 was significantly negatively correlated with the SDS score. The above results indicate that it is necessary to popularize COVID-19 and mental health-related knowledge to adolescents during the pandemic so as to enable them to recognize the occurrence of the pandemic and their own emotional changes correctly, establish a positive concept of prevention and treatment, and reduce unnecessary excessive stress reactions.
Meanwhile, the history of mental and psychological diseases is also one of the most important influencing factors in the group mood of adolescent students. As shown in the results, history of psychiatric disorders was significantly associated with anxiety and depressive symptoms. The results of regression analysis showed that it was significantly negatively correlated with SDS and SAS scores, that is, subjects with a history of psychosocial disorders had lower SDS and SAS scores than normal subjects.
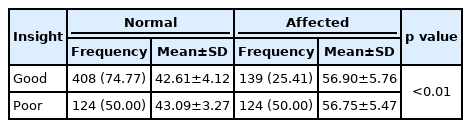
In addition, the study investigated subjects’ perceptions of their own emotional changes (significant change, moderate change, unclear, mild change, or no change), and correlated the results with the scores of SDS and SAS. We classified the subjects into those who 1) picked ‘significant change’ or ‘moderate change’ option and with anxiety, depression, or either; 2) picked ‘unclear’ or ‘mild change’ or ‘no change’ option and without anxiety and depression into the category of ‘good insight’. As for subjects who picked ‘significant change’ or ‘moderate change’ without anxiety and depression, and those who picked ‘unclear’ or ‘mild change’ or ‘no change’ with anxiety, depression, or either, they were classified into the category of ‘poor insight’. In this way, the subjects’ insight was roughly estimated. As shown in Tables 8 and 9, anxiety and depression scores of subjects with good insight were lower than those of subjects with poor insight, and the detection rate also decreased significantly. In previous studies on the correlation between different mental disorders and insight, it was found that patients with different mental disorders and various degrees of mental disorders had varying degrees of self-knowledge impairment [46,47]. Another study on the association between depression and insight showed that insight was significantly correlated with depression, and the recovery of insight was synchronized with the improvement of depressive symptoms [48], which is basically consistent with our results of rough estimates of insight.
In the investigation of life events, we found that the main stressors of adolescent students during the period of the COVID-19 pandemic came from the stresses brought on by study, examination and further education, as well as family contradictions which caused by lifestyle, recreation, study and work. Meanwhile, we found that online courses are also one of the factors affecting the emotions of most adolescent students. It focuses on the lack of effective supervision, students’ lack of self-control, and worries about future examinations due to the unstable efficiency of online teaching. Compared with a study on the efficiency of online teaching and classroom teaching of an immunity course which showed that there are no differences between the two [49], the majority of the subjects in our study believed that the efficiency of online teaching is lower than that of classroom teaching. One possible reason may be that the respondents have different ages and learning abilities, and the group of adolescent students in the middle school still need to face the entrance examination, which has a heavier burden than that of the college students. Besides, the differences between the teaching concepts of universities and middle schools may also be the reason for the different result.
In order to deal with the threat that adolescent mental health facing during the COVID-19 pandemic, support from both family and community is necessary. First, it is important for relevant departments to spread clear and correct information about the COVID-19 pandemic to parents and adolescents, including the risks and possible changes in daily life. At the same time, parents and adolescents should be educated on mental health to recognize their emotional changes during the pandemic objectively and reasonable methods of catharsis should be taught to manage their negative sentiment. Second, the communities and schools should provide better online learning and interaction platforms to adolescents in order to meet their needs of education and the needs of communication between their peers [50]. Parents should try to maintain their children’s life rhythm, keep a balance between work and rest, exercise regularly, meanwhile, regular meals, balanced nutrition and adequate sleep should also be ensured. Final, emerging technologies such as remote consultation and diagnosis which are more suitable than face-to-face care should also be widely used, which can help support adolescents’ psychological and behavioral health during the pandemic.
Limitations
In addition to the observed findings above, some study limitations which may be addressed by future research should be taken in consider. The first limitation concerns the sampling error. Due to the limitation during the pandemic, our study was based on the internet platform. Though the internet penetration rate reached 70.4% by the end of December 2020 according to the Statistical report on the development of Internet in China from China Internet Network Information Center (CNNIC), there are still some parts of populations that were not covered by our study [51]. The second limitation concerns the absence of a direct assessment and observation of adolescents. The sole use of the self-rate scales is confine to participants’ capabilities to evaluate themselves and may biased by semantic understanding of the scales [52]. Third, though a primary study confirmed that the difference in children’s symptoms between areas identified by different levels of pandemic risk was not statistically significant [21], our sample mostly lived in eastern provinces of China, thus, we cannot assume that our findings can be generalized to the whole China national population.
In conclusion, this study investigated the mental and psychological health of the adolescent students during the period of the COVID-19 pandemic and their possible related factors. Due to limitations during the epidemic, the authenticity of the questionnaire may be biased by using the online questionnaire as the medium of choice for the questionnaire. Although random sampling was adopted in this study, due to the different populations using different networks and social software, specific bias may exist in gender, and further follow-up studies are needed to expand the sample size.
Notes
Availability of Data and Material
All data, models generated or used during the study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Rongjuan Guo. Data curation: Tian’ge Lu. Formal analysis: Yao Yu. Investigation: Tian’ge Lu, Yao Yu, Zhonghui Zhao. Methodology: Tian’ge Lu, Yao Yu, Zhonghui Zhao. Project administration: Tian’ge Lu. Resources: Rongjuan Guo, Tian’ge Lu. Supervision: Rongjuan Guo. Validation: Zhonghui Zhao. Visualization: Tian’ge Lu. Writing—original draft: Tian’ge Lu. Writing—review & editing: all authors.
Funding Statement
None
Acknowledgements
We are grateful for Tianyi Lu’s great help in data collection. And we are also very appreciative of Jin Zhao and Hejing Lu who provided the linguistic assistance during the preparation of this manuscript. Besides, we thank Lianhan Shang and Yuze Liu for their suggestions on the submitting process.