INTRODUCTION
In the Diagnostic and Statistical Manual, 5th edition (DSM-5), adjustment disorder is defined by the development of emotional or behavioral symptoms in response to an identifiable stressor occurring within 3 months of the onset [
1]. These symptoms or behaviors are clinically significant with marked distress that is out of proportion to the severity or the intensity of stressor and with significant impairment in social, occupational, or other important areas of functioning. Subtypes of adjustment disorder may include depressed mood, anxiety, disturbance of conduct, and any combinations of such symptoms. Since adjustment disorder was included in the Diagnostic and Statistical Manual, 3rd edition (DSM-III) in 1980 and International Classification of Disease, 10th edition (ICD-10) in 1993 [
2,
3], it has been regarded as one of the most frequently diagnosed mental disorders in clinical practice [
4]. However, it has not received enough academic attention, which would cause the exact nature of adjustment disorder to be remained unknown. In addition, it has been known that adjustment was often unrecognized [
5].
In general, adjustment disorder seemed to be very prevalent in primary care settings where the long-term impact of illness and related psychosocial problems were common. In a population-based study in old age groups, a point prevalence of adjustment disorder was 2.3% [
6]. In a recent study which was performed to develop a diagnostic instrument for adjustment disorder in 323 individuals claiming disability benefit after 2 years of sickness absence due to any medical conditions, the prevalence of adjustment disorder was 7.4% [
7]. In addition, a point prevalence of adjustment disorder was found in 15.4% of patients in palliative care settings and in 19.4% of patients in hemato-oncological care settings, respectively [
8]. However, none of previous major epidemiological studies including the Epidemiologic Catchment Area (ECA) study, the National Comorbidity Survey, and the Household Survey have included adjustment disorders [
9-
11], although it was already suggested that adjustment disorders are common in general population since formal criteria of adjustment disorder were established [
2,
3].
Thus, there were only a few studies regarding the prevalence of adjustment disorder in general population. Using the Schedule for Clinical Assessment in Neuropsychiatry (SCAN), Casey et al. [
12] estimated the prevalence of adjustment disorder was 0.3%. Using a questionnaire including a life events checklist and self-rating items regarding symptoms of adjustment disorder and symptom duration, Maercker et al. [
13] reported that the prevalence of adjustment disorder ranged from 0.9% to 1.4% according to clinical impairment. To our best of knowledge, there have been no studies regarding the annual incidence and direct medical costs of adjustment disorder in general population. As adjustment disorder is common diagnosis in a primary care setting and can be best treated by members of multidisciplinary team in psychiatric clinic with appropriate skills [
14], there would be a need for comprehensive information regarding adjustment disorder across primary care settings.
The National Health Insurance Database (NHID) which is a public database operated by the Korean National Health Insurance Service (NHIS) was founded in 2012 and have contained almost all medical claims data in Korea [
15]. NHID have provided information on not only health care utilization but also health screening, socio-demographics, dates of death, and Korean Standard Classification of Diseases (KCD) diagnostic codes, which has been based on ICD-10 [
3]. Given the scarcity of previous reports regarding the incidence, the prevalence, and the economic burden of adjustment disorder, NHID would be an important resource for examining the epidemiology of adjustment disorder. The current study was performed in order to ascertain the number of people who were newly diagnosed with adjustment disorder annually from 2011 to 2017, and to estimate direct medical cost in people with adjustment disorder.
RESULTS
From 2011 to 2017, total number of patients with adjustment disorder and the incidence of adjustment disorder were increased consistently. The number of newly diagnosed patients were 11,029 in 2011 and reached to 18,850 in 2017. In addition, the annual incidence of adjustment disorder was 22.0 per 100,000 persons in 2011 and 36.8 per 100,000 persons in 2017. During this period, the number of patients and the annual incidence in female were higher than those in male (
Table 1).
The incidence of adjustment disorder according to age groups was presented in
Table 2. The highest number of newly diagnosed patients were found in 50-59 years of age group. However, considering cumulative number of population from 2011 to 2017 in each age group, the incidence was highest in 70-79 years of age group.
The incidence of adjustment disorder according to insurance types was presented in
Table 3. The highest number of newly diagnosed patients were found in self-employed individuals group. However, the incidence of adjustment disorder was highest in medical aid beneficiaries group, as the number of patients was divided by cumulative number of population from 2011 to 2017 in each group.
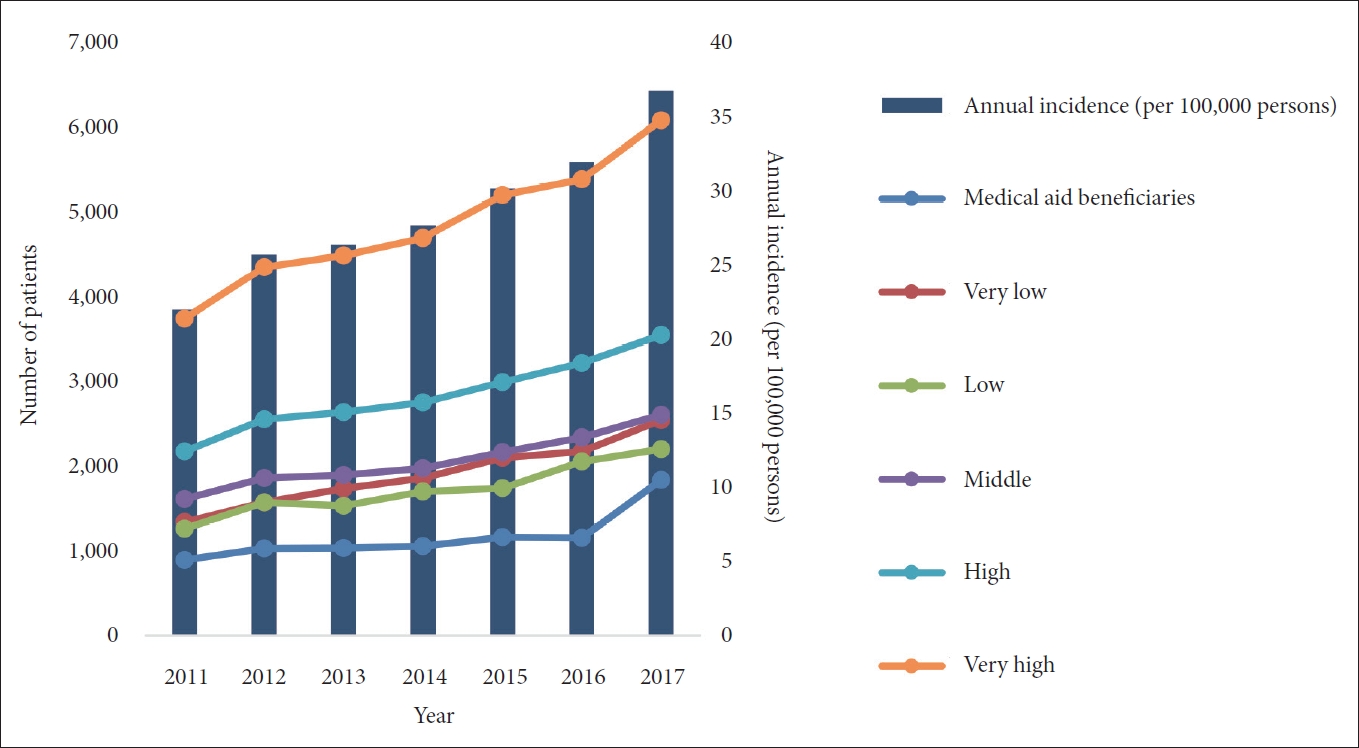
When we divided patients with adjustment disorder into 6 groups by income (i.e., very high, high, middle, low, very low, and medical aid beneficiaries group), the number of patients was highest in very high income group and lowest in medical aid beneficiaries group (
Figure 1). Although the order of the number of patients by year seemed to be mixed in part, high number of patients was found in order of very high income group, high income group, middle income group, very low income group, low income group, and medical aid beneficiaries group in 2017 (
Figure 1). As the exact number of population in any groups by years was not available, the changes in the incidence of adjustment disorder in each 6 group could not be calculated.
We also estimated prevalence and direct medical cost of patients with adjustment disorder from 2011 to 2017. The number of all patients with adjustment disorder and the prevalence of adjustment disorder in 2017 were higher than those in 2011. In addition, annual prevalence of adjustment disorder was in the range from 95.4 to 116.4 per 100,000 persons. Higher number of all patients and higher prevalence were found in order of 2017, 2016, 2012, 2011, 2015, 2013, and 2014, respectively. Total direct medical cost of adjustment disorder was continuously increased except 2015 and the total direct medical cost per person was 231.4 USD in 2017. Most direct medical cost was claimed by outpatient clinics and inpatient unit from psychiatric department (
Table 4).
DISCUSSION
To our best of knowledge, the current study is the first one reporting the annual incidence of adjustment disorder in general population. From 2011 to 2017, the annual incidence of adjustment disorder in Korea was in the range from 22.0 to 36.8 per 100,000 persons and increased continuously. During the same period, the annual prevalence rate of adjustment disorder was 106.4 per persons in 2011 and reached to 116.4 per 100,000 persons. These increases may be partly explained by increased perception of stress as common one that should be managed properly in Korea [
17], although social stigma towards mental illness has been still present [
18]. The annual prevalence of adjustment disorder in general population in the current study is lower than expected from the results of previous study in general population [
12,
13]. This difference might be caused by study methods and biased sample. Because the results in the current study was derived from claims data, only those who intended to be diagnosed and treated would be included as patients in NHID. Considering remained social stigma towards mental illness [
18], it seemed that most patients those experience significant stress should tolerate and would remain untreated. In addition, some patients would be treated by psychosocial treatment outside medical settings (e.g., work-related counselling centers in their workplaces, private counselling centers, public counselling centers, etc.).
There has been no previous studies regarding annual incidence of adjustment disorder, although the prevalence of adjustment disorder in general population has been estimated in a few studies. In Casey et al.âs study [
12], 14,387 adults aged between 18 and 64 from 5 countries including Ireland, Britain, Norway, Finland, Spain were screened by Beck Depression Inventory (BDI) with the cut-off score of 13. Those scoring 13 and more in BDI were interviewed using the Schedule for Clinical Assessment in Neuropsychiatry (SCAN) in which ICD-10 diagnosis of adjustment disorder could be made. After these 2 stage screening method was administered, in approximately 6,800 individuals, the overall weighted prevalence of adjustment disorder was 0.3%. In this study, it seemed that adjustment disorder was found more in rural area, female, not single, and aged 30 and more groups, respectively. In Maercker et al.âs [
13] study, 2,511 participants aged between 14 and 93 in Germany were evaluated using questionnaires including life-events checklist in which 7 types of acute stressful events (e.g., divorce, moving, etc.) and 10 types of chronic stressors (e.g., conflict with neighbors, serious illness, etc.) could be assessed and self-rating items regarding symptoms of adjustment disorder and symptom duration, and impairment. They reported that 0.9% of the sample could be diagnosed with adjustment disorder with the impairment criteria and that 1.4% was diagnosed with adjustment disorder unfulfilling the impairment criteria. In this study, adjustment disorder was found more in female. In addition, higher prevalence rates were found in order of middle-aged adults, older adults, and young adults, respectively.
In partial accordance with these results [
12,
13], the number of patients and the incidence rate in female was higher than those in male in the current study. While the number of newly diagnosed was highest in 50-59 years of age group, actual incidence rate was highest in 70-79 years of age group in the current study when we took into account the cumulative number of population in each group. As the number of elderly population has been increased rapidly in last decades in Korea, it was expected that it would take 18 years to be changed from an aging society to an aged society from 2000 to 2018 [
19,
20]. In addition, the economic poverty despite of increase in economic activity participation and separation from original family members in elderly population has been increased recently [
21]. All these change seemed to be significant stressors which were related to the increase in the annual incidence of adjustment disorder in elderly population.
Similarly, although the highest number of newly diagnosed patients with adjustment disorder were also found in self-employed individuals, highest incidence rate was also found in medical beneficiaries group, taking into account the cumulative number of population. When we divided patients with adjustment disorder into 6 groups by income for detailed analyses, while the number of patients was highest in very high income group and lowest in medical aid beneficiaries group consistently, higher number of patients was found in order of very high income group, high income group, middle income group, very low income group, low income group, and medical aid beneficiaries group in 2017. Considering the number of population in each 5 income quintile groups was approximately 7 times more than that in medical beneficiaries group, we could speculate that actual incidence of adjustment in medical beneficiaries group was also highest among 6 groups.
These results seemed to be in partial accordance with results from a recent study using the 11th revision of the International Classification of Disease (ICD-11) [
22] criteria of adjustment disorder. In 330 individuals who had job loss with involuntary causes, the unsatisfactory financial situation of the household of the participants was associated with a full adjustment diagnosis [
23]. This may be partly explained by the nature of stressors in adjustment disorder, as financial adversities were also one of significant stressor which could cause adjustment disorder in those who had vulnerabilities [
22].
In the current study, annual direct medical cost of adjustment disorder was continuously increased except 2015 and annual direct medical cost per person was reached 231.4 US dollars in 2017. Most direct medical cost was claimed by outpatient clinics and inpatient unit from psychiatric department. To our best of knowledge, this is the first study estimating the direct medical cost in adjustment disorder in general population.
There were a few limitations in the current study. As the current study used claims data from hospitals, patients who began treatment outside of a hospital were not included. The results of the current study would not reflect the precise incidence of adjustment disorder. In addition, as the current study was based on rather diagnostic codes recorded in claims data than standard interviews, diagnostic scales, and laboratory data, the diagnostic validity could be low and biased. Nevertheless, considering relatively lack of evidences in adjustment disorder in general population, the current study has the strength to examine the diagnosed incidence for adjustment disorder using data recorded by physician in representative of the national population.
As global interest in stressor and related symptoms has been growing recently, proper information on adjustment disorder will not only allows us to accumulate more knowledge about these disorders themselves but also lead to more appropriate therapeutic interventions by improving the ability to cope with stressor-related symptoms and adversities. As the incidence and direct medical cost of adjustment were increased despite of social stigma, public education regarding identification and management of stress and its related sequelae as well as evidence-based treatment in medical settings should be provided.