Advanced Cognitive-Behavioral Treatment Model with Exposure-Response Prevention for Treating Obsessive-Compulsive Disorder
Article information
INTRODUCTION
Obsessive-compulsive disorder (OCD) is characterized by recurrent obsessions and compulsions, which are significantly associated with psychic distress and functional impairment [1]. Meanwhile the treatment modality and clinical outcomes for patients with OCD are also highly complex leading to decimating clinical course in naturalistic treatment setting [2,3]. Exposure-response prevention (ERP) therapy entails learning how to reduce fear (habituation) without engaging in the compulsive behavior after experiencing the anxiety-producing stimulus [conditioned stimuli (CS)]. Foa et al. discussed habituation based on emotional processing theory (EPT) and argued that between-session habituation was the most important treatment [4-6]. Although ERP therapy is effective for many patients with OCD, not all patients respond to the treatment, as 25–50% of patients discontinue the therapy or experience recurrence [7]. Some researchers have argued that habituation, which is generally understood to be the most important aspect of ERP therapy, may not be the key for treatment [8]. Craske et al. proposed inhibitory learning theory (ILT) as an alternative to EPT [8-10]. Based on fear extinction research, they proposed a framework for exposure in which inhibitory learning is optimized to enhance long-term outcomes. In fact, both EPT and ILT use learning theory (i.e., classical and operant conditioning) to understand and treat patients. This article examines limitations of applying learning theory (Supplementary Materials in the online-only Data Supplement) that we identified during ERP therapy in patients with OCD. Based on this understanding, we propose an advanced cognitive-behavioral theory (CBT) model of OCD by combining learning theory and Beck’s cognitive model to better apply ERP therapy to OCD.
ADVANCED MODEL FOR OCD CBT WITH ERP
In this article, we propose an advanced CBT model with ERP for treatment of OCD by applying Beck’s cognitive model to learning theory [11]. Beck’s cognitive model states that thoughts, emotions, and behaviors are mutually influenced by each other. Shifting cognition is seen as the main mechanism by which lasting emotional and behavioral changes take place. We illustrate the combination of Beck’s cognitive model and learning theory in Supplementary Figure 1 (in the online-only Data Supplement).
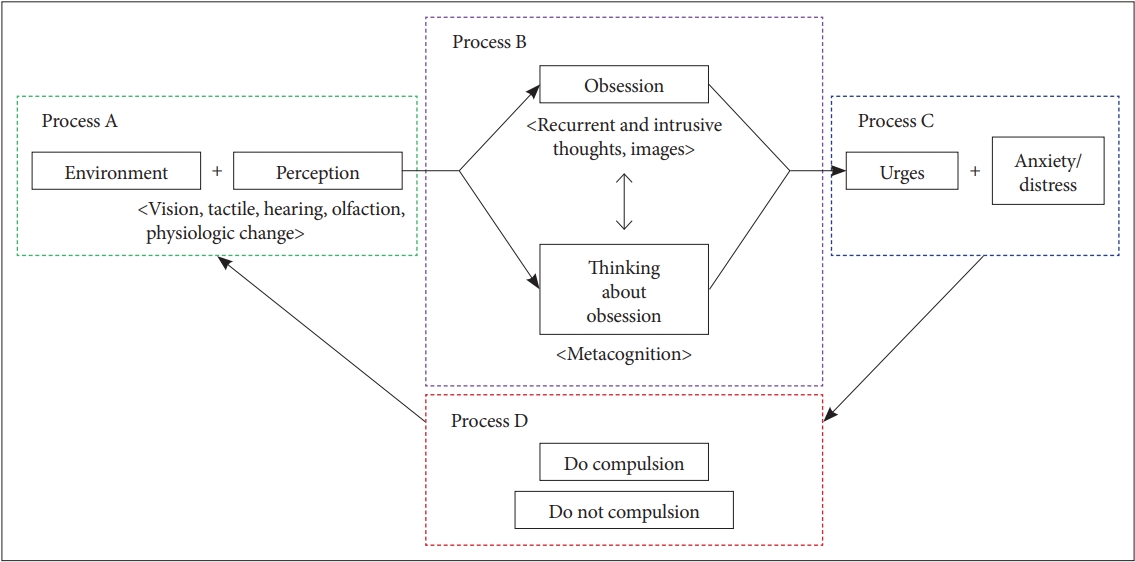
The newly proposed CBT model for OCD is shown in Figure 1. For this CBT model, we identified four elements of ERP therapy (Figure 1) to explain the difference between ILT and EPT. For easy application in a clinical situation, the terminology used are the words used for OCD in the DSM-5. The reasons for dividing each step into four processes are as follows.
Process A consists of an environmental factor and perception. This step suggests the stimulus that causes the obsession, as described in classical conditioning, and the pathway by which patients receive the external situmulus. For example, external environments (e.g., waste and handles) are important to OCD patients who engage in excessive washing behavior, but they perceive these objects as contaminated, so they become obsessed with them. We named this process perception. People can sense tactically, and the handle of a door may feel different for each person. It may feel smooth to one, while it may feel sticky to another person. In other words, objective facts are received differently by each person, and such perceptions are fundamental to the cognitive model. By using this concept, it is possible to account for the greater frequency and longer duration of compulsion, which are not explained by existing learning theory. Patients may wash their hands for 20 minutes or longer after gripping a door handle to remove the stickiness they feel on their hands. However, they may still feel sticky for longer than 20 minutes. Moreover, another environmental stimulus, water may also feel sticky. Hence more compulsive washing may be performed to remove the stickiness. Process A may help to clarify why patients experience obsessions and compulsions. Instead of just identifying the stimuli that cause the obsession and compulsion, a therapist will perform ERP therapy better when they know how the patient is perceiving the stimulus.
Process B consists of obsession and thinking about the obsession. The key at this step is the notion of “thinking about the obsession,” i.e., the concept of metacognition. Metacognition, or thinking about thinking, helps people to develop their problem-solving ability by learning what works, and it serves as a core part of self-regulated learning [12,13]. After process A, the patient experiences an obsession, and their metacognition finds a way to solve this problem of obsession (i.e., they think about their obsession). By presenting this process, we can more easily explain the differences between EPT and ILT in ERP therapy. The exposure therapy on which ILT focuses encourages patients to understand the intention of the therapy and increase their motivation for participating in therapy, educating them about the useful aspects of not acting compulsively, though they experience unpleasant perceptions, obsessions, urges, and anxiety/distress. The patients then go through an ERP session to learn inhibition. After process A, they may understand that they can actively select one of two learning types: 1) excitatory learning, in which they undergo the previous compulsion, or 2) inhibitory learning, acquired during therapy. Repeated ERP sessions involve the process of training the patient to choose the latter. At this time, if the patient experiences habituation while doing ERP sessions, the treatment effect may be increased.
Process C consists of managing urges, anxiety/distress, and habituation, as it is important in ERP therapy to apply EPT at this stage. Process D focuses on the compulsion and not enacting the compulsion. After this step, the patient repeats the steps by returning to process A.
The advantages of applying Beck’s cognitive model to learning theory are as follows. First, considering the limitations of the aforementioned learning theory, Beck’s cognitive model is more applicable to OCD because it has been used to treat depressive disorder. Furthemore, rumination, which is frequently found in patients with depression, is similar to obsession in OCD. Second, the frequency and duration of the compulsion can be explained. The key to Beck’s cognitive therapy is to identify and correct how the patient’s inner psyche accepts what has happened. If this is explained based on criterion B for OCD in the DSM-5, patients’ compulsive behavior, which is intended to relieve anxiety, is inadequate, so they repeatedly and continuously experience the compulsion. Finally, it is useful for describing ERP treatment with ILT. In the proposed model, the application of ERP to ILT focuses on process B and D rather than the habituation experience (process C).
We present two cases in which ILT was applied using the above model (Supplementary Materials in the online-only Data Supplement). To show the differences between this and EPT treatment, one case is a treatment case with habituation and inhibitory learning, and the other is a case of inhibitory learning treatment without habituation.
DISCUSSION
A recently published article found that difficulty with inhibiting OCD behaviors may result from a more intense initiation of responses [14]. The authors asserted that OCD patients demonstrated compulsive behavior and impaired inhibitory control under conditions of conflict. ILT can be used to help CBT therapists teach patients to suppress urges during behavioral therapy. ILT suggests that two kinds of learning occur due to the obsession triggered by the CS: 1) excitatory learning acquired during previous fear acquisition (conditioned stimulus–unconditioned stimulus) and 2) new inhibitory learning acquired during ERP (conditioned stimulus–no unconditioned stimulus) [8]. Expectancy violation during exposure helps to establish an inhibitory association with a CS that had previously been associated with an excitatory response [9]. However, the empirical literature evaluating hypotheses derived from the inhibitory learning approach to exposure is lacking. We have suggested some limitations of learning theory to elucidate existing OCD theory (Supplementary Materials in the online-only Data Supplement), and have provided an advanced CBT model for overcoming such limits.
The most important difference between EPT and ILT is the cognitive approach to obsession and compulsion. The cognitive approach focused on EPT aims to allow patients to learn that their obsessional anxiety is not permanent and that, until habituation is effective, they should resist the urge to perfrom the compulsive behavior to avoid discomfort [15]. Unfortunately, only a few patients experience habituation during treatment. It is very difficult to force patients who visit a hospital due to distress derived from an obsession to withstand discomfort that is not easily alleviated, which often leads to treatment failure. On the other hand, habituation is not a treatment goal in ILT, but a part of the treatment process. We believe that increasing the patient’s tolerance for anxiety, distress, and urges has important clinical value in treating OCD and complements the goal of inhibitory learning. The patient is repeatedly exposed to the CS to learn to not perform the compulsion in response to a given obsession, with or without habituation. In this regard, ERP using ILT is expected to contribute to enhancing patient compliance with the therapy.
When we apply this advanced CBT model, the patients who did not experience habituation but was more confident in controlling themselves through the process D of ‘Do not compulsion.’ We focused on the fact that the ILT approach could allow patients to more actively participate in the therapy. Encouraging patients to recognize their ability to actively control obsessions while participating in ERP is very important for the therapy. Olatunji et al. [16] found that the core of OCD is a negative appraisal of intrusive thoughts, with thoughts such as “I am out of control” and “I am a terrible person.” Since these metacognitons were identified after the development of classical and operant learning, learning theory cannot be applied perfectly to them. The term “thinking about obsession” in our CBT model is useful to make up for the shortcomings of these learning theories. When we use this model in a cognitive approach, we focus on patients’ thinking about their obsessions, not on patients’ obsessions.
However, the present model also has some limitations. It was somewhat difficult to explain mental compulsion using this model. Perhaps the reason for this is that the proposed model involves patient behavior during process D, as mental compulsion is the act of thinking about the obsession (process B) rather than an active behavior itself. These concepts need to be modified or supplemented through further discussion.
The goal of this article was to present an approach to optimizing the inhibitory learning component of ERP. Although we offer an advanced model for facilitating this goal, therapists should exercise some flexibility when applying this model.
Supplementary Materials
The online-only Data Supplement is available with this article at https://doi.org/10.30773/pi.2020.0340.
Acknowledgements
This study was supported by a grant (B2020-0208) Chonnam National University Hospital Biomedical Research Institute to J-MK.
Notes
The authors have no potential conflicts of interest to disclose.
Authors’ contribution
Conceptualization: Ju-Wan Kim. Data curation: Ju-Wan Kim. Funding acquisition: Jae-Min Kim. Investigation: Ju-Wan Kim. Methodology: JuWan Kim. Project administration: Sung-Wan Kim, Il-Seon Shin, Jae-Min Kim. Supervision: Jae-Min Kim. Visualization: Ju-Wan Kim, Hee-Ju Kang, Ju-Yeon Lee, Il-Seon Shin. Writing—original draft: Ju-Wan Kim. Writing—review & editing: Ju-Wan Kim, Sung-Wan Kim, Jae-Min Kim.