A Descriptive Study on the Civil Lawsuits of Medical Malpractice Occurred during Psychiatric Ward Treatment
Article information
Abstract
Objective
Medical accidents have resulted in actual harm for patients, been costly for health care system, and diminished trust for both patients and practitioners. The present study analyzed malpractice claims related to accidents in psychiatric inpatient units.
Methods
This study analyzed defendants, cases and plaintiffs or patients characteristics, degrees of injury, and types of accidents in 85 civil malpractice suits filed from 2005 to 2015 with a focus on the methods and locations of suicides.
Results
Most defendants were psychiatrists (n=43). Of the 85 cases, 56 (65.9%) were decided in favor of the plaintiff, most commonly on the grounds of negligence and violation of sound facility management principles. The most common diagnosis of patients was schizophrenia (n=31). The damages were deaths in 52 cases and injuries or other damages in the remaining 33 cases. The most common accident was suicide (n=28), followed by escape attempts (n=15). The most common suicide method was hanging (n=21), which was usually committed in the private room using objects like door handles.
Conclusion
To reduce medical accidents, medical staff should monitor high-risk patients closely and constantly. Sufficient numbers of well-trained personnel are required to meet this standard. Reducing environmental hazards such as removing anchor points and installing door locking systems will improve patient safety.
INTRODUCTION
There has recently been a significant increase in public awareness of medical error, since an important report on preventable medical errors had been published [1]. Medical accidents have resulted in actual harm for patients, been costly for health care system, and diminished trust for both patients and practitioners.
More than half of medical error disputes are settled through mediation and arbitration, but the rest are litigated [2]. Malpractice claims place a significant financial burden, time demands, emotional distress and moral pressure on the physicians who face them [3,4]. Physicians often order more tests for patients than is likely necessary, so this so-called defensive medicine trend drives up the cost of medical care [5]. Psychiatrists also experience emotional distress after medical accident which may cause feelings of failure or morbid symptoms [6]. Some psychiatrists even stop practicing altogether [7].
This study analyzed malpractice lawsuit data to better understand the characteristics of accidents that occurred in psychiatric wards resulting in patient injury. Data about concluded lawsuit is a useful resource for studying medical accidents resulting in severe injuries. This study focused on ward environments of patient with suicide, because inpatient suicide can occur even when the patient is in under observation and only has access to limited materials and areas [8]. This study also examined the characteristics of the defendants and case. This paper will suggest strategies for individual practitioner and institutions for preventing suicide and other accident that cause patient injuries in psychiatric ward.
METHODS
The databases of judgment search system of South Korea Supreme Court library were retrieved for the case number that had reached final judgment between January 2005 and December 2015, using the search terms “compensation for medical litigation,” “neuropsychiatry,” “psychiatry,” “mental patient,” and “psychiatric.”
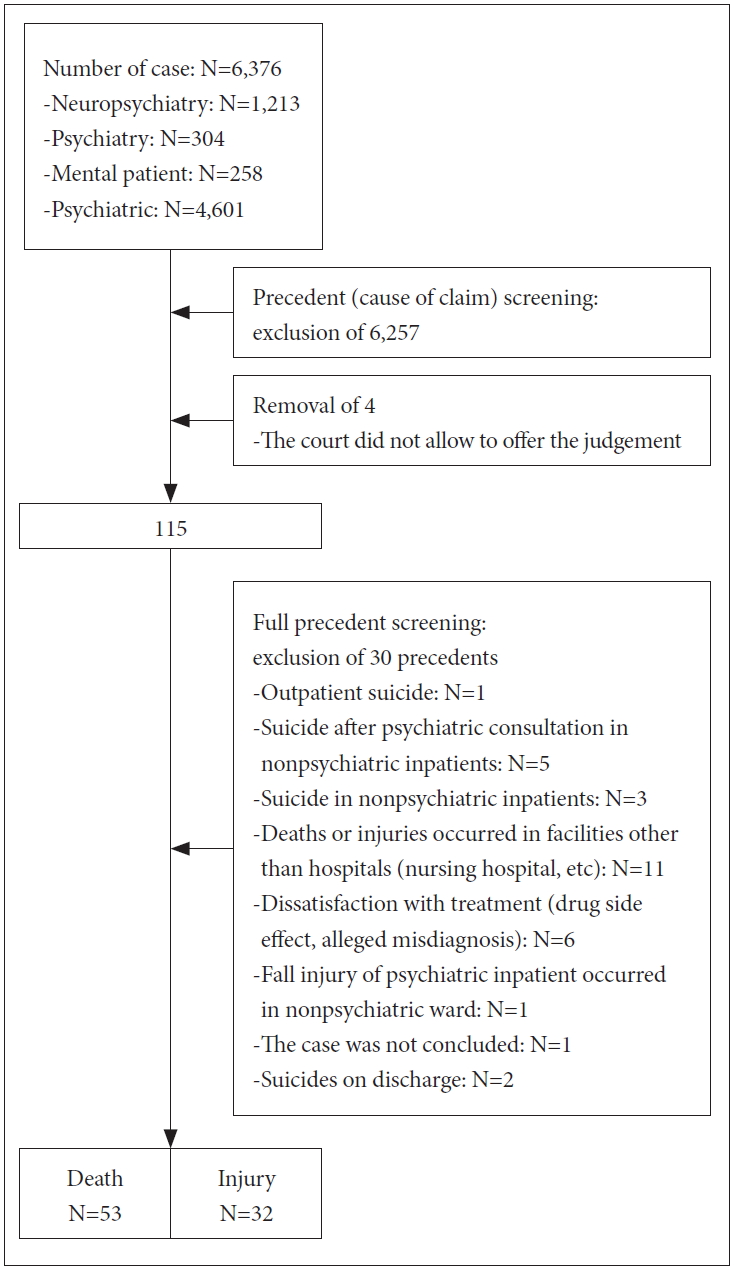
The initial search yielded 6,376 cases, of which 6,257 were excluded during the initial screening. The following were excluded from the study: 1) those alleging malpractice that occurred in outpatient clinic, nursing care center, oriental medicine hospital or residential facility; 2) those in which the alleged malpractice occurred during a consultation; and 3) those alleging the violation of involuntary admission rules. And 4 cases were excluded due to being not available and further 30 precedents were excluded after full text screening for the following reasons: outpatient suicide (n=1), suicide after psychiatric consultation in nonpsychiatric inpatients (n=5), suicide in nonpsychiatric inpatients (n=3), deaths or injuries occurred in facilities other than hospitals (n=11), dissatisfaction with treatment such as drug side effect and alleged misdiagnosis (n=6), fall injury of psychiatric inpatient occurred in nonpsychiatric ward (n=1), not concluded case (n=1), suicide on the day of discharge (n=2); 85 could be included for analysis (Figure 1).
Patient outcomes were categorized as either death or nonmortal injury. The International Classification for Patient Safety (“ICPS”) classified degree of harm in increasing order of severity as none, mild, moderate, severe, and death. In order for the injury to qualify as death, the patient’s death had to have been caused by and occurred shortly after the accident which was alleged to have caused the patient’s injury [9]. Due to limited precedent, death was defined as having occurred when the dead patient was discovered and after cardiopulmonary resuscitation and surgical treatment failed to revive them or if death occurred within six months of the accident in question due to complication caused by the accident, such as pneumonia. All other harm was defined as injury to define the severity. Accidents were categorized according to the standards followed in other studies and the ICPS [9-12]. Jumpings from a height were classified as suicides, escape attempts, or jumps of unknown causes in accordance with patient’s intent and the judge’s rulings.
The time at which the accidents in question occurred were categorized as occurring during the day or night and during the weekday or the weekend. The weekend was defined as 18:00 Fridays to 08:00 Mondays. Legal holidays were classified as weekends. There was insufficient information about facility shift, so the day shift was defined as 08:00 to 18:00 and the night shift as 18:00 to 08:00.
The management level was defined as whether the staff managed the patient by psychiatrist’s order, or facility regulation on high-risk patient. The precedent did not reveal whole records of hospitalization, so this study figured out by rulings about the duty of care.
This study had descriptive analysis of the patient and defendant characteristics such as patient’s age, diagnoses, and the defendant’s status. The legal proceeding has information of the amount, malfeasance that the judge ruled, and the limitation of liability ratio, so this study also described the result of civil lawsuit.
The present study’s protocol was reviewed and approved by the Institutional Review Board of Yonsei University Severance Hospital (Y-2018-0144).
RESULTS
The mean patients age was 430.6±149.9 months (range, 181–827 months) and patients were more frequently male (n=38) than female (n=23), but 24 cases did not described the patient’s sex. Most patients had a single diagnosis (n=67) while others had two (n=11), three (n=2), and four (n=1) diagnoses. The most common diagnosis was schizophrenia (n=31). Other diagnoses included pathologic gambling, eating disorder, impulse control disorder, and conduct disorder (Table 1). The defendants were psychiatrists (n=43), medical legal entities (n=28), educational entities (n=13), attending physicians (n=5) and other health care providers (n=13) (These results were collected by multiple response) (Table 2).
Of the examined cases, 1 was adjudicated by the Supreme Court, 29 by appellate court, and 55 by trial courts, and 56 (65.9%) found in favor of the plaintiff. The average initial amount claimed by the plaintiffs was KRW 223,766,865±202,955,300. The average amount awarded was KRW 62,765,780. The limitations of liability ratio of the defendants were an average of 34.1%±18.6.
Findings in favor of the plaintiff were on the ground of negligence (n=49) and violations of facility management duties (n=23), insufficient provision of emergency treatment (n=4), delayed diagnosis or transfer (n=3), failure to obtain informed consent (n=1), violation of medical contract (n=1), the supervisor’s liability to adult incompetent to tort responsibility (n=1), and the employer’s liability (n=7). Some cases included findings of malfeasance on multiple grounds.
The majority of cases were about death (n=53), while the rest were about injuries.
The most common type of accidents was suicide (n=28), followed by escape (n=15), fall (n=6), jumping out a window for an unknown cause (n=6), drug side effect (n=4), transport-related injury (n=3), asphyxiation (n=5), assault by another patient (n=4), delayed treatment or transfer (n=11) and restraint-related injury (n=3). Hanging (n=20) was by far the most common method which patients most commonly committed using their uniforms (Table 3). Bathrooms and showers were common locations for suicide and the ligature fixation points for hanging were taps, door hinges, and door handles. Of those who committed suicide, 14 had been hospitalized as suicide risks or were to have engaged in suicidal behaviors in the past. However medical staff failed to monitor 10 of these patients prior to their suicides (Table 4).
Accidents in which patients jumped from a height occurred because of unlocked doors in closed ward (n=1) or the wards were open (n=2) or patients were outside of the ward to walk or visit with others (n=4). With regard to staff, they were focused on other patients, or they left doors open (Table 5).
Accidents occurred an average of 148.6±412.7 days after admission. The median number of days after admission was 16 with a range of 1 to 2,214. Patients with depressive disorder had accidents an average of 33.2 days after admission while patients with schizophrenia had accidents an average of 268 days after admission. Accidents were more likely to occur at night than during the day and on weekdays than during the weekends (Table 6).
DISCUSSION
The accidents, plaintiffs, defendants, the damages and legal proceedings in civil suits that arose over injuries suffered by psychiatric ward inpatients were analyzed. In many of the cases it was concluded that patients had been injured due to negligence in patient and facility management, so this study’s results have implications for how to prevent suicide and other accident that cause patient injuries in psychiatric ward. This study focused on suicide, because inpatient suicide can prevent when the patient in under proper observation and only access to safe environment. This study’s findings can be used to change operations and guidelines of inpatient psychiatric units, by extension, of medical-surgical units when they care patients comorbid with unstable psychiatric disorder [13].
This study found the most common suicide method was hanging, which was usually committed in the private room using objects like door handles. Other studies about environmental risk factors have emphasized anchor points in inpatient suicide, which were doors, door handles and hinges in 53.8% of cases [11]. Restricting access to or removing anchor point could be an effective way to reduce the number of inpatient suicides [12]. After the Department of Veterans affairs began using the Mental Health Environment of Care Checklist [14] when designing or monitoring psychiatric wards, the suicide rate decreased dramatically from 4.2 to 0.74 per 100,000. This effect was found to have persisted after five years [15].
Sometimes facility modifications are not possible due to privacy concerns, so constant observation is an alternative method for reducing the number of suicides. Bathrooms and showers should be placed close to nurse stations and should be monitored by staff when high-risk patients are using them because security cameras cannot be used to monitor them [16]. In this study, some staffs monitored patient with a history of suicidal behavior poorly. Previous studies have shown that patient under observation untowardly committed suicide [17]. Other studies have found that observation staffs frequently breached procedure because they were responding to other patients or duties. The quality and consistency of observation depends on staffing level and the staff’s knowledge, experience, and communications practices [18]. Therefore, staff levels should be increased [19], staff should be trained about how to manage of high-risk patients, and clear inpatient management policies should be created and disseminated [17,20].
Although patients’ belonging and storage areas are generally regularly inspected, ward should begin collecting unnecessary underwear and uniforms that can be used as method of suicide. Bedding such as covers and sheets should not be allowed in seclusion rooms. Policies on banned items have been criticized as inconsistent because they are based on each facilities’ past events [21]. It may be useful for physicians and safety supervisors to share information about medical accident and modify their regulations based on that information.
Approximately 80% of suicides occurred within three months of admission and the median day of suicide attempt was 14 days after admission. Previous studies have produced similar results [12,22]. The suicidal risk for patients with schizophrenia remains elevated for longer after admission than patients with depression [23], so the suicide risk of patients with schizophrenia should be regularly reassessed.
Unlike previous studies [24,25], accidents were more likely to occur during weekdays. The staffs have to handle a lot of duties for admission, discharges, and interventions during weekdays. Also the higher rate of accidents at weekdays might be the result of a staff shortage. When compared with other OECD countries with the same levels of GDP like Canada and Brazil, the number of psychiatrists per 1,000 population in Korea is 0.07 in 2016 while the average number in Canada or Brazil is 0.17. And the number of total mental health worker per 1,000 population is below than the average of high-income countries [26]. Backup system and clear assignment of duties will reduce staff work overload and guarantee adequate level of observation. And studies for sufficient qualification and number of staff will be required.
This study was limited in that it was only based on partial information of accident, facility regulation, and facility characteristics, so it was impossible to inspect safety and security policies in detail. In addition, the cases were anonymized, so it was impossible to analyze the ages of the defendants, which would likely correspond to their level of experience and whether they had professional liability insurance, which would reduce the burden of the lawsuit. Relevant patient characteristics that might be revealed in psychiatric interview records, nursing records, medical exams, and psychological test results were also not tested in this study. Some of total accidents were included because only civil lawsuits were analyzed, but it is difficult to obtain medical dispute data, so this study can serve as a valuable fundamental data source which inpatient facility managers can draw on to prevent medical accidents.
Future studies should analyze total accidents to better understand psychiatric inpatient ward accidents which cause patient injuries. Psychiatric facilities can voluntarily report laboratory results, medication prescriptions, nursing records, interview records and psychological test results, so it is possible to consistently understand patient and institutional factors that influence occurrence of accidents that cause patient injuries.
In conclusion, this study analyzed civil lawsuits filed over medical accidents in inpatient mental health units that resulted in patient injury. Psychiatrists can reduce the number of these accidents by closely managing high-risk patients and modifying ward environment. Many parts of ward can be used as weapons or suicide methods, so removing anchor points and installing proper locking system and barriers will reduce inpatient suicide. If patients are allowed to leave the ward, guards or staffs should accompany them and security cameras should be installed over windows.
Acknowledgements
None.
Notes
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Song Ii Ahn, Dong Ho Song. Data curation: Song Ii Ahn. Formal analysis: Song Ii Ahn. Funding acquisition: Song Ii Ahn. Investigation: Song Ii Ahn, Won Lee, Dong Ho Song. Methodology: Won Lee. Project administration: Dong Ho Song. Resources: Song Ii Ahn. Software: Song Ii Ahn. Supervision: Won Lee, Dong Ho Song. Validation: Song Ii Ahn, Won Lee. Visualization: Song Ii Ahn. Writing—original draft: Song Ii Ahn. Writing—review & editing: Won Lee, Dong Ho Song.