|
 |
- Search
| Psychiatry Investig > Volume 17(4); 2020 > Article |
|
Abstract
Objective
Methods
Results
ACKNOWLEDGEMENTS
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Bumjo Oh, Je-Yeon Yun, Jin Kim, Bum-Joo Cho. Data curation: Je-Yeon Yun, Eun Chong Yeo, Bum-Joo Cho. Formal analysis: Eun Chong Yeo, Dong-Hoi Kim, Bum-Joo Cho. Funding acquisition: Bum-Joo Cho. Investigation: Bumjo Oh, Je-Yeon Yun, Bum-Joo Cho. Methodology: Dong-Hoi Kim, Jin Kim, Bum-Joo Cho. Project administration: Jin Kim, Bum-Joo Cho. Resources: Dong-Hoi Kim, Jin Kim, Bum-Joo Cho. Software: Eun Chong Yeo, Bum-Joo Cho. Supervision: Dong-Hoi Kim, Jin Kim, Bum-Joo Cho. Validation: Bumjo Oh, Bum-Joo Cho. Visualization: Eun Chong Yeo, Bum-Joo Cho. WritingŌĆöoriginal draft: Bumjo Oh, Je-Yeon Yun, Bum-Joo Cho. WritingŌĆöreview & editing: Bumjo Oh, Je-Yeon Yun, Bum-Joo Cho.
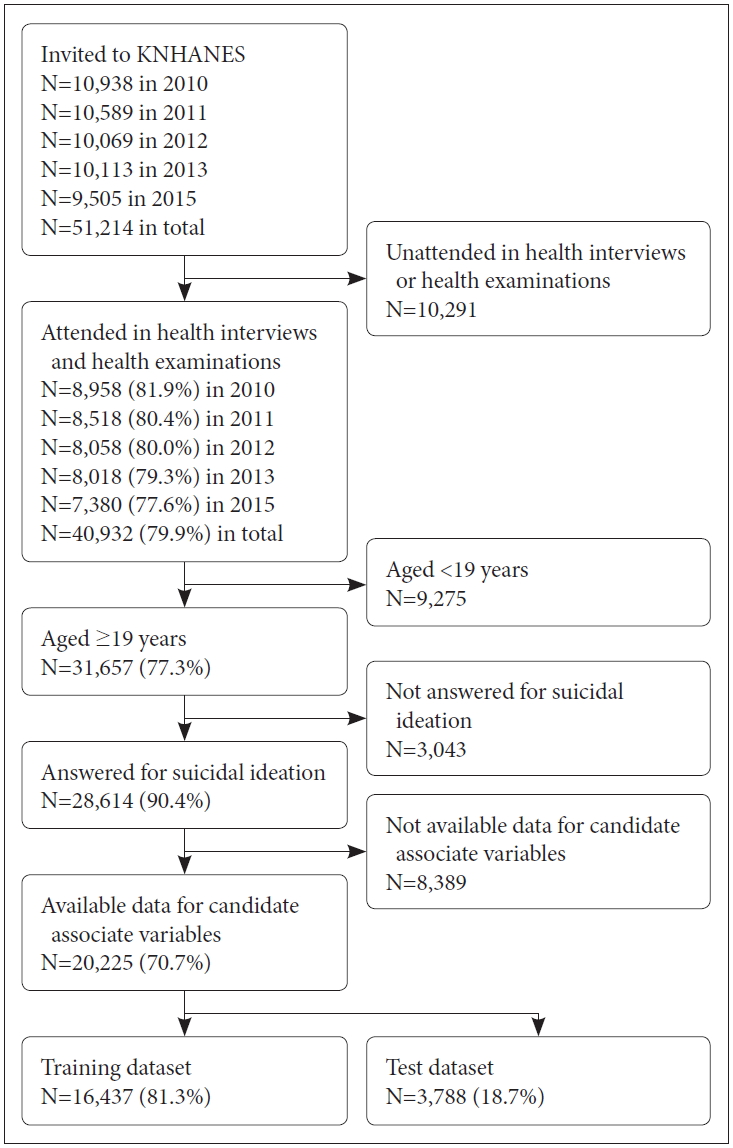
Figure┬Ā1.
Table┬Ā1.
| Total subjects (N=16,437) | Without suicidal ideation (N=14,480) | With suicidal ideation (N=1,957) | p* | |
|---|---|---|---|---|
| Age, year | 49.9┬▒15.8 | 49.4┬▒15.6 | 53.4┬▒16.7 | <0.001 |
| Sex, male | 7,293 (44.4) | 6,646 (45.9) | 647 (33.1) | <0.001 |
| Residency, urban | 13,113 (79.8) | 11,639 (80.4) | 1,474 (75.3) | <0.001 |
| Household income, quartile | <0.001 | |||
| ŌĆāLowest | 2,955 (18.0) | 2,346 (16.2) | 609 (31.1) | |
| ŌĆā2nd | 4,275 (26.0) | 3,738 (25.8) | 537 (27.4) | |
| ŌĆā3rd | 4,554 (27.7) | 4,114 (28.4) | 440 (22.5) | |
| ŌĆāHighest | 4,653 (28.3) | 4,282 (29.6) | 371 (19.0) | |
| Educational status | <0.001 | |||
| ŌĆāŌēżElementary school | 3,716 (22.6) | 2,965 (20.5) | 751 (38.4) | |
| ŌĆāMiddle school | 1,807 (11.0) | 1,571 (10.8) | 236 (12.1) | |
| ŌĆāHigh school | 5,725 (34.8) | 5,171 (35.7) | 554 (28.3) | |
| ŌĆāŌēźUniversity graduate | 5,189 (31.6) | 4,773 (33.0) | 416 (21.3) | |
| Family members | 3.2┬▒1.3 | 3.2┬▒1.2 | 3.0┬▒1.3 | <0.001 |
| Governmental life support | 958 (5.8) | 757 (5.2) | 201 (10.3) | <0.001 |
| Marital status | <0.001 | |||
| ŌĆāNot married | 1,851 (11.3) | 1,655 (11.4) | 196 (10.0) | |
| ŌĆāMarried, live together | 12,773 (77.7) | 11,389 (78.7) | 1,384 (70.7) | |
| ŌĆāMarried, separated | 105 (0.6) | 84 (0.6) | 21 (1.1) | |
| ŌĆāBereavement | 1,208 (7.3) | 959 (6.6) | 249 (12.7) | |
| ŌĆāDivorced | 500 (3.0) | 393 (2.7) | 107 (5.5) | |
| High risk drinking | 1,796 (10.9) | 1,577 (10.9) | 219 (11.2) | 0.719 |
| AUDIT score | 5.7┬▒6.4 | 5.7┬▒6.3 | 6.1┬▒7.5 | 0.015 |
| Smoking | 0.004 | |||
| ŌĆāNever smoker | 9,353 (56.9) | 8,216 (56.7) | 1,137 (58.1) | |
| ŌĆāEx-smoker | 3,718 (22.6) | 3,330 (23.0) | 388 (19.8) | |
| ŌĆāCurrent smoker | 3,366 (20.5) | 2,934 (20.3) | 432 (22.1) | |
| Physical exercise | 9,535 (58.0) | 8,595 (59.4) | 940 (48.0) | <0.001 |
| Subjective health status | <0.001 | |||
| ŌĆāVery good | 746 (4.5) | 698 (4.8) | 48 (2.5) | |
| ŌĆāGood | 4,768 (29.0) | 4,452 (30.7) | 316 (16.1) | |
| ŌĆāNormal | 7,874 (47.9) | 7,074 (48.9) | 800 (40.9) | |
| ŌĆāBad | 2,503 (15.2) | 1,931 (13.3) | 572 (29.2) | |
| ŌĆāVery bad | 546 (3.3) | 325 (2.2) | 221 (11.3) | |
| Hypertension | 3,514 (21.4) | 2,963 (20.5) | 551 (28.2) | <0.001 |
| Stroke | 325 (2.0) | 259 (1.8) | 66 (3.4) | <0.001 |
| MI or angina | 428 (2.6) | 347 (2.4) | 81 (4.1) | <0.001 |
| OA or RA | 1,956 (11.9) | 1,532 (10.6) | 424 (21.7) | <0.001 |
| DM | 1,301 (7.9) | 1,098 (7.6) | 203 (10.4) | <0.001 |
| Retinal failure | 79 (0.5) | 58 (0.4) | 21 (1.1) | 0.001 |
| Liver cirrhosis | 56 (0.3) | 44 (0.3) | 12 (0.6) | 0.046 |
| Thyroid disease | 610 (3.7) | 514 (3.5) | 96 (4.9) | 0.004 |
| Asthma | 496 (3.0) | 401 (2.8) | 95 (4.9) | <0.001 |
| Atopic dermatitis | 365 (2.2) | 311 (2.1) | 54 (2.8) | 0.101 |
| Depressive disorder | 663 (4.0) | 403 (2.8) | 260 (13.3) | <0.001 |
| Cancer | 441 (2.7) | 385 (2.7) | 56 (2.9) | 0.655 |
| Injury within 1 year | 1,132 (6.9) | 946 (6.5) | 186 (9.5) | <0.001 |
| Unmet need for medical service | 2,670 (16.2) | 2,035 (14.1) | 635 (32.4) | <0.001 |
| Stress awareness | <0.001 | |||
| ŌĆāVery much | 663 (4.0) | 380 (2.6) | 283 (14.5) | |
| ŌĆāMuch | 3,428 (20.9) | 2,592 (17.9) | 836 (42.7) | |
| ŌĆāLittle | 9,763 (59.4) | 9,025 (62.3) | 738 (37.7) | |
| ŌĆāVery little | 2,583 (15.7) | 2,483 (17.1) | 100 (5.1) | |
| Continuous depressive mood Ōēź2 weeks | 2,035 (12.4) | 1,075 (7.4) | 960 (49.1) | <0.001 |
| Psychiatric consult within 1 year | 322 (2.0) | 167 (1.2) | 155 (7.9) | <0.001 |
| Absence from work within 1 month | 535 (3.3) | 401 (2.8) | 134 (6.8) | <0.001 |
| EQ-5D score | 0.9┬▒0.1 | 1.0┬▒0.1 | 0.9┬▒0.2 | <0.001 |
| Height | 162.6┬▒8.9 | 162.9┬▒8.8 | 160.0┬▒8.7 | <0.001 |
| Weight | 62.8┬▒11.5 | 63.0┬▒11.5 | 60.9┬▒11.4 | <0.001 |
| BMI | 23.7┬▒3.4 | 23.6┬▒3.3 | 23.7┬▒3.7 | 0.303 |
| Waist circumference | 81.0┬▒9.9 | 81.0┬▒9.8 | 81.4┬▒10.6 | 0.064 |
Table┬Ā2.
Table┬Ā3.
REFERENCES