Personality Traits Do Not Have Influence on Glycemic Control in Outpatients with Type 2 Diabetes Mellitus
Article information
Abstract
Objective
Glycemic control varies based on lifestyle factors and stress coping mechanisms, which are influenced by personality. The psychological factors associated with glycemic control have not yet been established in patients with type 2 diabetes mellitus (T2DM). The relationship between a 5-factor model of personality and glycemic control was evaluated in individuals with T2DM.
Methods
The subjects were 503 Japanese outpatients with T2DM. Glycated hemoglobin A1c (HbA1c) levels, depressive status, insomnia and personality traits were assessed. Lifestyle factors of the patients, such as habitual alcohol consumption and smoking, were also included in the analyses.
Results
Because the influence of insulin therapy on HbA1c is so strong, we stratified the patients according to insulin use. Simple regression analysis showed a significant correlation between HbA1c and neuroticism in patients who did not use insulin. After adjustment for confounders, multiple regression analyses revealed that none of the personality factors, including neuroticism, were found to be associated with HbA1c.
Conclusion
These findings suggest that personality traits do not have a large impact on glycemic control. Further studies are required to confirm the relationships between psychological factors and glycemic control using a longitudinal study design.
INTRODUCTION
Type 2 diabetes mellitus (T2DM) is regarded as a lifestylerelated disease, and T2DM can increase the risk of both serious physical and mental health issues [1]. Prolonged hyperglycemia or hypoglycemia can also induce negative emotional states in T2DM patients [2]. T2DM self-management is known to be burdensome because it requires self-discipline and perseverance to adapt everyday activities (exercise, diet, rest) to medication use and glucose levels [3]. Insulin therapy in particular may be associated with increased psychological distress [4].
Personality variability plays a determinant role in individual stress reactivity and psychological adjustment to diabetes, which may result in the onset of depressive symptoms [5,6]. Previous studies have suggested that individuals with T2DM and depressive and anxious temperaments adjust differently to diabetes and have worse self-management and metabolic control than subjects without a predominant affective personality [7-9].
Recently, the Five-Factor Model has been widely used in both clinical practice and scientific research to conceptualize personality [10]. Goodwin and Friedman have shown that people with diabetes have lower conscientiousness and openness and higher agreeableness than people without diabetes [11]. Goodwin, Cox, and Clara reported that neuroticism was related to an increased risk of diabetes [12]. In addition, a meta-analysis of five cohort studies revealed that diabetes incidence was associated with only low conscientiousness [13]. We have reported that neuroticism is associated with insomnia [14] and depressive status [15] in individuals with T2DM in Japan regardless of confounders such as lifestyle factors.
Several studies tried to find some associations between glycemic control and Five-Factor Model personality using simple regression model, which showed inconsistent results [16-22]. However, few studies have examined the comprehensive links using multifactor analysis, including lifestyle factors and psychological problems such as depression and insomnia, between the Five-Factor Model and glycemic control among individuals with chronic T2DM.
Based on these findings, we aimed to investigate the relationship between personality and glycemic control among individuals with T2DM.
METHODS
Participants
The protocol of the present study was approved by the ethics committee of the Hirosaki University School of Medicine (2015-002), and all subjects provided written informed consent before participating in this study. This study included 728 outpatients with T2DM who received treatment for at least 1 year at the Department of Endocrinology and Metabolism at the Hirosaki University Hospital, who were partly same sample as our previous studies [14,15,23,24]. We recruited 945 patients, and 728 agreed to participate in the survey. The remaining 217 patients were excluded because of refusal to participate (41 patients), moderate to severe dementia (85 patients), blindness (23 patients), and moderate to severe psychiatric diseases (e.g., bipolar disorder and schizophrenia; 68 patients). A total of 611 out of the 728 outpatients returned the questionnaires and were considered for inclusion in the study. Ultimately, 504 (69.2%) outpatients completed the questionnaires and were included in this study. No differences in demographic data were found between individuals who completed the questionnaire (n=504) and those who did not (n=107). Blood samples from these patients were collected routinely for glycated hemoglobin A1c (HbA1c) analysis at least 4 times per year. Among the subjects, 448 were taking an oral hypoglycemic agent and 237 were receiving insulin therapy. The demographic data (age, sex, smoking status, alcohol consumption, solitary living, and exercise habits) and medical histories of the patients were derived from questionnaires and medical records (Table 1).
We measured personality traits using the Japanese version of the Ten-Item Personality Inventory (TIPI-J). The TIPI-J is a measure of the Big-Five personality dimensions: extraversion, conscientiousness, neuroticism, agreeableness and openness to experience [25]. Each item was scored from 1 to 7 points, and the scores were summed. The TIPI-J has been validated and tested for reliability in Japan [26]. The Japanese version of the Center for Epidemiologic Studies Depression Scale (CES-D) was administered to all of the participants to measure their depressive symptoms [27,28]. The CES-D is a 20-item self-reported measure that focuses on the depressive symptoms the patient experienced during the week prior to completing the questionnaire. The maximum score is 60, with higher scores indicating more severe depressive symptoms. Subjective sleep difficulty was assessed using the validated Japanese version of the Pittsburgh Sleep Quality Index (PSQI-J) [29,30]. The PSQI-J is a self-rated questionnaire that measures sleep difficulty over 1 month. Higher PSQI-J scores indicate greater sleep difficulty.
Statistical analysis
The data are presented as the means±standard deviations. Linear regression analyses with forced entry were performed to examine the correlations between glycemic control (average HbA1c) and several factors, such as age, sex, body mass index (BMI), presence/absence of smoking, habitual alcohol consumption, living alone, exercise habits, PSQI-J, CES-D, and each score for the 5 personality factors. The interaction between insulin use and each personality trait was included in the subsequent multiple regression analyses.
We used the dummy variables as follows: male=0, female=1; absence of spouse=0, presence of spouse=1; living alone=0, living with family=1; absence of smoking=0, presence of smoking=1; absence of alcohol consumption=0, presence of alcohol consumption=1; no exercise=1, exercise once a week=2, exercise 2–3 days per week=3, exercise 4–5 days per week=4, and exercise almost every day=5; and insulin nonuse=0, insulin use=1. A p-value <0.05 indicated statistical significance. SPSS software for Windows, version 25.0, was used for all analyses. A p-value <0.05 was regarded as statistically significant.
RESULTS
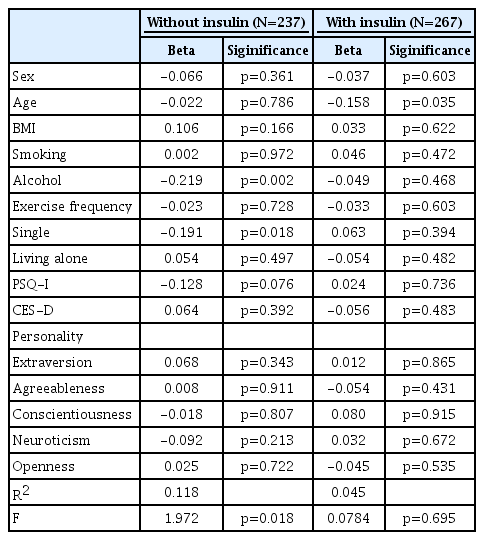
In the whole study sample, simple regression analyses revealed no correlations between HbA1c and any personality scores (Table 2). The multiple linear regression analysis that included age, sex, BMI, presence/absence of smoking, habitual alcohol consumption, living alone, exercise habits, PSQI-J, CES-D, and the score of each of the 5 personality factors revealed no association between HbA1c and any personality scores in the whole study sample (Table 2). Adding interaction variables during the final stage of the analysis revealed different patterns for each health behavior. Insulin showed a significant interaction with all factors in the FFM, while there was a nonsignificant interaction with lifestyle. When we stratified data by insulin use or nonuse, we found an inverse and significant correlation between neuroticism and HbA1c (p<0.05) (Table 3). However, the multiple linear regression analysis revealed that there was no association between HbA1c and any personality trait (Table 4). In addition, there were no differences in any of the personality traits between patients who used insulin and those who did not use insulin (Table 4).

Simple and multiple regression results for factors associated with glycemic control among total patients with type 2 diabetes mellitus
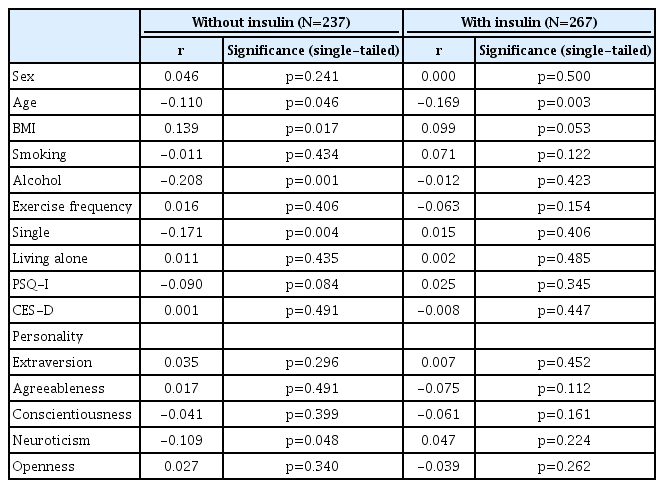
Simple regression results for factors associated with glycemic control among patients with type 2 diabetes mellitus who used and did not use insulin
DISCUSSION
The results of this study indicated that after adjustment for confounders, an association between neuroticism and HbA1c demonstrated an interaction with the use of insulin. Neuroticism was significantly associated with HbA1c in the simple analysis but not in the multiple linear regression analysis. Thus, when stratifying according to insulin use, there was no correlation between neuroticism and HbA1c levels regardless of insulin use. However, neuroticism is not related to the prevalence of obesity [31], the incidence of diabetes, or diabetes-related mortality [14]. The findings of this study indicate that neuroticism is not a protective factor for glycemic control in T2DM patients regardless of insulin use. Previous studies demonstrated nearly consistent results. A previous study revealed no association between abnormal glucose regulation and neuroticism in a population in the US [32]. In the study, better glycemic control at baseline was associated with a higher score of neuroticism, and after 6–12 months, this association remained for self-monitored blood glucose but disappeared for HbA1c [25]. Recent studies have shown no association between neuroticism and glycemic control in patients with type 2 diabetes in Australia [16], Korea [17], Scotland [18], and the US [19], and no association between neuroticism and type 1 diabetes was found in the US [20] or Belgium [21]. On the other hand, a positive relationship between HbA1c and neuroticism has been suggested in Iran, although confounding factors were not controlled [22].
Previous studies have shown that extraversion is consistently and inversely associated with HbA1c in Korean patients [17], Iranian patients [22] and American patients [19] with T2DM. However, we failed to find this association. This discrepancy may be explained by the characteristics of the subjects. The mean age was 25 years for the Korean population and 51 years for the Iranian population, while the mean age of our study population was 64 years. However, the mean age of the American patients was 69, the insulin use rate was 24.2%, which was much lower than that in our sample.
The results of this study indicated that conscientiousness was not associated with glycemic control. Previous studies have demonstrated inconsistent results. Five pooled American and British studies showed that low conscientiousness is associated with an increased risk of incident diabetes and diabetesrelated mortality in adulthood [31]. This association was partially explained by the higher prevalence of obesity [14] and lower physical activity among those with low conscientiousness. Additionally, inverse correlations were found in Iranian patients with T2DM [22] and Bulgarian patients with type 1 diabetes mellitus [21]. On the other hand, a few studies have shown no association between conscientiousness and glycemic control using OGTT in Korean [17] and Australian individuals [16] and American patients [19].
Type D personality is characterized by two stable personality traits: negative affectivity (NA), which is the characteristics of experiencing negative emotions towards time and situations, and social inhibition (SI), which is the characteristic of inhibiting the expression of emotions and associated with glycemic control [33,34]. Type D was found to be more prevalent in diabetes patients than controls. Type D personality is a significant predictor of both poor medication adherence and unhealthy behaviors [33]. HbA1c was significantly higher in T2DM patients with Type D personality than in patients with non-Type D personality [34]. Because Type D personality is correlated with neuroticism [35], it was expected that HbA1c would have been positively correlated with neuroticism. However, HbA1c was inversely correlated with neuroticism. The discrepancy between the associations of Type D personality and neuroticism with HbA1c may be explained by the SI aspect of Type D personality. The association between SI and neuroticism was weak, although statistically significant [36].
This study has several notable limitations. First, we used the TIPI-J to determine the 5 personality factors. Although the TIPI-J is very simple and feasible, it does not correlate perfectly with the gold standard measurements, such as the Neuroticism, Extroversion, Openness (NEO) scale and the FFM. Second, we did not examine the effect of euthymia. Euthymia is a condition characterized not only by the absence of affective disorders but also by the presence of positive psychological factors such as psychological flexibility, frustration tolerance and resistance to stress [37-39]. Such a state of positive mental health was found to be an important health target in patients with diabetes. Finally, this study is limited by its cross-sectional design; thus, we could not determine a causal relationship between personality and glycemic control among the patients in our study population. A follow-up survey is needed to investigate these associations.
In conclusion, personality traits were not associated with HbA1c in Japanese patients with T2DM. The findings indicated that some personality traits may affect glycemic control among individuals with T2DM who do not use insulin to less extent. Further studies using a longitudinal study design and a large sample are required to confirm the relationships between personality traits and glycemic control among T2DM patients.
Acknowledgements
This study was funded by a Grant-in-Aid for Scientific Research (KAKENHI) from the Japan Society for the Promotion of Research JSPS (15K01643 and 15H04754). The funders had no role in the study design, data collection and analysis, the decision to publish, or the preparation of the manuscript.
Notes
Norio Yasui-Furukori has been a speaker for Dainippon-Sumitomo Pharmaceutical, MSD, and Otsuka Pharmaceutical.
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Norio Yasui-Furukori, Hiroshi Murakami. Data curation: Hideyuki Otaka. Formal analysis: Norio Yasui-Furukori. Investigation: Jutaro Tanabe, Miyuki Yanagimachi, Masaya Murabayashi, Koki Matsumura, Yuki Matsuhashi, Hirofumi Nakayama, Satoru Mizushiri. Project administration: Hiroshi Murakami. Resources: Hiroshi Murakami. Software: Norio Sugawara. Supervision: Makoto Daimon, Kazutaka Shimoda. Validation: Norio Sugawara. Writing—original draft: Norio YasuiFurukori. Writing—review & editing: Makoto Daimon, Kazutaka Shimoda.